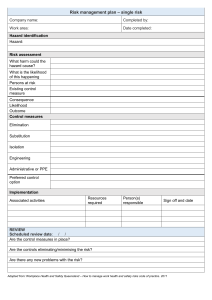
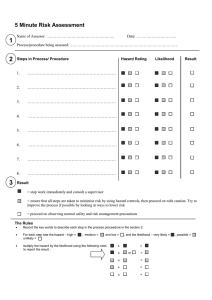
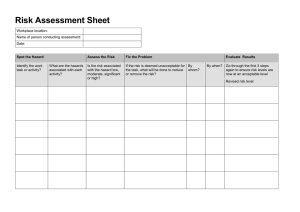
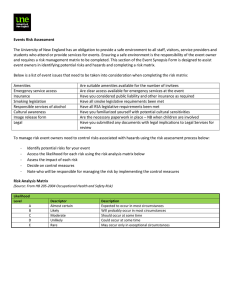
OUTLINE I. Biorisk Assessment VIII. Robust Risk Assessment II. Biorisk A. Risk Acceptance III. AMP Module B. Risk Evaluation A. Hazard IX. Risk Evaluation IV. What is a Risk? A. Risk Distribution V. Risk as an Equation X. BioRAM VI. Multi-Drug Resistant Titan XI. Summary Blue (MDR-TB) XII. References VII. Risk in the laboratory XIII. Appendix OBJECTIVES 1. Understand what risk is. 2. Understand the components of a suitable risk assessment methodology, and the critical resources required. 3. Become familiar with a biorisk assessment model that addresses safety and security. 4. Be able to execute a risk assessment with the model. 5. Identify/justify/quantify key risk drivers. LEGEND REMEMBER ● ● 3. 1 SEMESTER CLINICO-PATHOLOGICAL CONFERENCE & SPECIAL TOPICS 1.01 BIORISK ASSESSMENT: AMP MODULE Dr. Edith Tria | 08/26/2022 How do you know that your risk management is working, and will continue to work? Risk Evaluation of Performance III. AMP MODULE Key Components of Biorisk Management 1. Biorisk Assessment 2. Biorisk Management 3. Biorisk Performance Evaluation FIGURE 1. Overview of BRM AMP Model LECTURE I. BIORISK ASSESSMENT Laboratory biosafety – containment principles, technologies, and practices implemented to prevent unintentional exposure to pathogens and toxins, or their unintentional release Laboratory biosecurity – institutional and personal security measures designed to prevent the loss, theft, misuse, diversion, or intentional release of pathogens and toxins A. GROUP EXERCISE 1 Q: What are the risks of working in a laboratory with biological materials? Possible Answers: o Accidental injury (burns, electrical, chemical, trauma, and spill accidents o Infection thru various mode of transmission (needle prick, inhalation, ingestion, contact thru fomites) o Near missed incidents that have harmful consequence (psychological stress, mental illness, trauma) II. BIORISK All about the risk associated with biological materials in the laboratory incorporating biosafety and biosecurity. Laboratory Biorisk Management Standards o System or process to control safety and security risks associated with the handling or storage and disposal of biological agents and toxins in laboratories and facilities o International Standard: CWA 15793:2011 A. GROUP EXERCISE 2 Question and Answer: 1. How do you identify the risks in a laboratory? Risk Assessment/Hazard Analysis and Identification of likelihood of exposure to hazard that has harmful consequence 2. Which steps do you take to manage these risks? Risk Mitigation/ Reduction/and Prevention of exposure to hazard that may cause harmful consequences POC: DIMAANDAL | GONZALES, MEDIANISTA, TAMAYO A. HAZARD Hazard is a source that has a potential for causing harm Hazard is not a risk without a specific environment or situation. i. EXERCISE 1 Question and Answer: 1. What affects whether there is an incident with the shark? Eg. Shark Bite Factors affecting the likelihood of the exposure incident with shark: small boat, pirates with one eye, pirate with one foot, pirate standing on the edge of the boat, birds to distract pirates, strong winds, strong waves, treasure box underwater, pirates have the desire to get the treasure; pirates went deep sea diving 2. How likely is an incident? Less likely: pirates are a good swimmer; pirates diving is in full geared suit; shark is fed and not hungry; with diversion to distract shark Moderate to happen: playful shark, pirate not an expert swimmer and in half full swimming/ or diving geared PPE Very likely to happen: hungry shark, accident fall or drowning pirates, no swimming geared PPE, not a good swimmer. 3. An incident with the shark would be how severe? Less: scratch injury Moderate: partial amputations, or deep wound injury Very severe: death or total amputation, physical and mental disability – PTSD Post traumatic syndrome disorder 4. What are the consequences of the incident? Give as any outcome from exposure to shark. Consequences: Shark bite, death of pirates, scattered or loss of treasures; drowning incidents; falling accidents; quarrel / squabble / disagreement of two pirates; shark is killed, boats got overturn ii. GROUP EXERCISE 1, STEP 1 Scenario: A two-year-old child is left alone in a kitchen while there is boiling water on the stove. Question and Answer: 1. What could go wrong? List all the possibilities. 1 2. 3. Possibilities can be anything from injury (from boiling water, from fire, from gas explosion, from fall of pot) Kidnapping being alone, boy start to cook, death of the child (from explosion, fire, electrocution, severe degree of scald burn) House will get on fire Choose the most likely single most important risk for this scenario. Scald burn injury Identify the hazard for that risk. Hazards: boiling pot, hot stove, being alone, 2-yearold very young child; possible stool or chair nearby; inquisitive child; light clothing to being naked child. High volume of water in the pot; high thermostat temperature of stove; make-up of the kitchen either wooden or cemented; make-up of the stove either gas stove, and electrical stove; child may be restrained or not; the height of the child; gender of the child –boy are more inquisitive; hungry child IV. WHAT IS RISK? Risk is the likelihood of an event with a hazard that has consequences. A risk can be defined in several ways, but for our purposes we could say that risk is the likelihood of an adverse event of some consequence happening. Thus, risk is thus a function of the Likelihood a particular adverse event will occur, and the Consequences of that event. R = f (L, C) TABLE 1. Factors that influence the likelihood and consequences of the risk DEGREE OF RISK LOW MODERATE HIGH LIKELIHOOD low volume of boiling water in the pot: slight degree of scald burn moderately high volume of boiling water: 2nd degree burn overflowing boiling water: 3rd degree burn CONSEQUENCE child maybe restrain loosely or no stool/low height of child/finger burn child maybe tall, with nearby chair or not restrained/hand burn child maybe tall, with nearby chair or not restrained, inquisitive, hungry child: 3rd degree burn of whole body Low: volume of water, degree of burn, easily reached stove by the child. pot no cover, child is asleep, child wearing a thick cloth. i. HAZARD, THREAT, AND RISK What would be different if the risk were the child being injured by an older brother, whose toy had just been broken by the two-year-old? What is the hazard (threat) now? Answer: The hazard here is the Brother, meaning it’s all about biosafety, biosecurity if the hazard/threat is now a person. Sino magiinjure? Yung brother. What is the difference between a hazard and a threat? o A hazard is an object that can cause harm o A threat is a person who has intent and/or ability to cause harm to other people, animals, or the institution o A risk can be based on either a hazard and/or a threat ii. RISK, LIKELIHOOD, AND CONSEQUENCES How can we define risk, likelihood, and consequences? o Risk is the likelihood of an event with a hazard that has consequences o Likelihood is the probability an event occurring o Consequences is the severity of an event FIGURE 2. Likelihood vs. Consequences One way to visualize risk is to graph it. Shown on the left is a 2- dimensional graph, with Likelihood in the y-axis and Consequences in the x-axis. This graph allows us to fully determine the risk associated with something by assign values to both likelihood and consequences. For example, there are some risks with very low likelihood, but high consequences and vice versa. To become more familiar with this concept of risk we will work through the following example. V. RISK AS AN EQUATION The actual function will depend on the nature of the risk. Risk graphs do well to exhibit this relationship, as well as provide a useful tool in biorisk management. Risk levels equate to specific areas of the graph. Thus, risk is a function of the likelihood a particular adverse event will occur, and the consequences of that event. Formula: R = f (L,C) A. GROUP EXERCISE 1, STEP 2 Scenario: Consider again the two-year-old in the kitchen scenario: Risk: Child being burned by the boiling water Hazard: Pot of boiling water on the stove o Identify the factors that influence the likelihood and consequences of the risk; use post-it notes for each factor o Evaluate the risk (low, moderate, high) FIGURE 3. Risk equation graph POC: DIMAANDAL | GONZALES, MEDIANISTA, TAMAYO 2 i. RISK GRAPH I Risk curves can also be referred to as “isoquants”. An isoquant has the same (iso-) value (-quant) on every point of its line. Previously, when characterizing risk, we used a graph with risk curves, or “isoquants”, showing the different levels of risk, from Very High to Very Low One way to visualize risk is to graph it. Shown on here is a 2-dimensional graph, with likelihood in the y-axis and consequences in the x-axis. This graph allows us to fully determine the risk associated with something by assign values to both likelihood and consequences iv. RISK GRAPH IV FIGURE 7. Small amount of cold water in the pan over a hot stove, step stool next to stove, child not restrained High likelihood because the child is no restrained with stool beside the child, but low consequence because only small amount of cold water. v. RISK GRAPH V FIGURE 4. Risk curves ii. RISK GRAPH II FIGURE 8. Small amount of cold water over a hot stove, no step stool, child strapped in a high chair Very low — low kasi wala naman mainit na tubig at hindi rin gagalawin. FIGURE 5. Large amount of boiling water on front of stove, step stool next to stove, child not restrained Very high iii. RISK GRAPH III FIGURE 6. Large amount of boiling water, no step stool, child strapped in a high chair There is high consequence kasi high amount of boiling water, pero low likelihood kasi the child is strapped, so the answer is high consequences and low likelihood. POC: DIMAANDAL | GONZALES, MEDIANISTA, TAMAYO VI. MULTI-DRUG-RESISTANT TITAN BLUE (MDR-TB) Scenario B Multi-Drug-Resistant Titan Blue (MDR-TB) Summary of Experiment: DSSM, Culture and Sensitivity of MTB A laboratory is culturing of MDR-TB for antibiotic susceptibility testing. MDR-TB isolates are grown and exposed to a variety of antibiotic drugs to determine susceptibility. Agent Criteria: Infectious Dose: 10 bacilli by inhalation for humans and animals Stability: SUSCEPTIBILITY TO DISINFECTANTS: Greater resistance to disinfectants and require long contact times for most disinfectants to be effective; 5% phenol, 1% sodium hypochlorite (only if low organic matter and longer contact times), iodine solutions (high concentration of available iodine required), glutaraldehyde and formaldehyde (longer contact time) are effective PHYSICAL INACTIVATION: Sensitive to moist heat (121° C for at least 15 min), light SURVIVAL OUTSIDE HOST: Guinea pig carcasses - 49 days; carpet - up to 70 days; dust - 90 to 120 days; cockroaches - 40 days; manure 45 days; paper book - 105 days; sputum (cool, dark location) - 6 to 8 months; clothing - 45 days 3 Incubation Period: 4-12 weeks from infection to primary lesion or significant titan blue antigen skin reaction. The risk of progressive pulmonary or extrapulmonary tb is greatest within 1 to 2 years after infection. It may persist for a lifetime as a latent infection. Mortality Rate: 50-70% of untreated patients with active pulmonary tb, within 2 years. Rates are higher for those with concurrent HIV infection. Morbidity: Duration of Illness: as an active disease, 6 months to 2 years. Survival ranges from 1.5 months in immune compromised HIV patients to 14.3 months in normal patients with drug susceptible TB. Severity of Illness: High. ● Duration of Infection: Possibly lifetime. ● Long term effects after infection: Active disease can be triggered at any time after the establishment of a latent infection, though the probability of developing active disease is higher 1-2 years after infection, in immune compromised patients, small children, young adults, and the very old. The morbidity rate in bovines is around 40%. Agent known to infect other species but is most prevalent in bovines. Allergen (yes/no): No Carcinogenic/mutagenic (yes/no): No Abortogenic (yes/no): No Toxin Production (yes/no): No Immune Suppression (yes/no): No Ability to Mutate in Host or Environment (yes/no): Yes Infection Mitigation Measures: For human pathogens o Immunization: Yes o Prophylaxis: No (standard TB prophylaxis of isoniazid is ineffective for MDR-TB) o Post Infection Treatment: First line TB drugs isoniazid and rifampin are ineffective for MDR-TB. A variety of second-line drugs are available to treat MDRTB, usually done so in combination with each other, though they are less effective than the first line options. One common combination for suspected MDR-TB patients includes streptomycin, isoniazid, rifampin, ethambutol, pyrazinamide, MXF & cycloserine (Isoniazid and rifampin are maintained due to their effectiveness against regular TB). o Existence of Diagnostic tests: Yes. Traditional skin test or TST, and newer interferon release assays (IGRA) Routes of Infection in Humans: Inhalation: Yes Contact: No Vector-Borne: No Sexual Transmission: No Vertical Transmission: No Routes of Infection in Bovine: Inhalation: Yes Ingestion: Possible Percutaneous: No Contact: No Vector-Borne: No Sexual Transmission: No POC: DIMAANDAL | GONZALES, MEDIANISTA, TAMAYO Vertical Transmission: No Communicability: Human to Human: Yes, though less likely for MDR-TB compared to normal TB Human to Animal: No Evidence Animal to Animal: No Evidence Animal to Human: No Evidence Multiple Species: Yes. Where is it present: Worldwide. One third of the world’s population is infected with TB. MDR-TB is much less prevalent. However, cases of MDR-TB are rising. It is highly endemic in the population surrounding the laboratory. Perception of malicious use: LOW. Culture: Sputum from patients suspected of having TB can be cultured for evidence of TB in several different media, the most common of which is Lowenstein-Jensen medium. While not particularly difficult to culture, TB has an unusually slow growth rate, and it takes 6-8 weeks to grow enough bacteria for diagnosis and drug susceptibility testing. Equipment: Bench, culture plates, liquid cultures, wire loops, burners, glass flasks, glass tubes, vortexer.. Lab Environment: Open window ventilation, lab coats, no vaccination available, humid environment, surgical masks, gloves worn occasionally, lab waste is hauled away for offsite treatment, open campus with no locks on doors, cultures not secured or inventoried, no personnel verification program.VIII VI. RISK IN THE LABORATORY A. GROUP EXERCISE 2, STEP 1 Consider the first biological scenario (MTB): Define the risks in this scenario. How do you assess risk in this set up? Write down your listing as many as you can answers, in the meta cards? i. GUIDE & STUDY QUESTIONS FOR THE SEMINARWORKSHOP Given the following case scenario: 1. What could go wrong? List all the possibilities. 2. Choose the single most important possibility for this scenario 3. Identify the factors that may lead to this possibility. 4. What affects whether or not there is an incident with this TB exposure? 5. How likely is an incident? 6. What are the consequences of the incident? 7. Identify the factors that influence the likelihood and consequences of that possibility; use post-it notes for each factor. 8. Evaluate such possibility to happen as low, moderate, high. 9. What control measures can you do to address/solve this problem? 10. How will you know whether or not your solutions worked? ii. EXERCISE 1 Question: On what aspect of biorisk did you focus? Possible Answer: 4 TABLE 2. Factors to consider in a laboratory biosafety risk The focus aspects include range of practices and procedures to ensure the biosecurity, biosafety, and biocontainment of those infectious agents and toxins. These also include the full spectrum of safety and security measures for laboratories, from standard operating procedures to physical measures to individual practices in the laboratory. See Appendix A and B for the risk assessment for MTB scenario RISK CHARACTERIZATION AGENT PROPERTIES (PATHOGENS) LABORATORY INFRASTRUCTURE: (PLACE) HUMAN FACTORS (PEOPLE) ENVIRONMENT AND COMMUNITY FACTORS: FIGURE 9. Flow Chart for MTB Process B. GROUP EXERCISE 2, STEP 2 Using the MTB scenario: 1. Choose one (1) risk to assess 2. Define the hazard and/or threat 3. Can you evaluate the risk of this scenario? If so, what is it (low/moderate/high)? 4. Capture answers on a flip chart and report to the class? Using the MTB scenario: What different type of information do you need to do a risk assessment? List all questions that you think need to be asked. Risk Characterization: What factors should be considered in a laboratory biosafety risk assessment? (What are the factors that affect Likelihood and/or Consequences) Categorize the criteria: Put the questions, or criteria, into four or five general categories. Categorize the questions, or criteria, according to o Likelihood o Consequences Which of these criteria are relatively more important than the others? How might the result of your risk assessment change using this process (compared to your earlier method)? • How has your risk assessment improved? Think about how you assessed the risk of the two-year-old in the kitchen/ tiger attack and how you assessed the HIV scenario the first time. POC: DIMAANDAL | GONZALES, MEDIANISTA, TAMAYO OPERATIONAL FACTORS: PRACTICES/ PROCEDURES FACTORS AFFECTING THE RISK Pathogenicity / Virulence Infectious Dose Potential Outcome of Exposure Morbidity / Mortality Availability of therapeutic Interventions Potential Routes of Infection Stability of the Agent in the environment Heating, Ventilation, and Air Conditioning (HVAC) System Control Open Windows Public Access Work Surfaces Workflow Pest Control Equipment/ Proper lab supplies Level of Training/Skills/ Competency Level of Experience Proper Technique/ Follow SOPS Proper work management/ Workload and Fatigue Health and Immune Status of the Workforce Presence of the Agent in the Environment Around the Laboratory Immune Status of the Community Population Density of the Community Presence of Suitable Hosts or Vector Good Laboratory Practices Housekeeping and Cleanliness Use of Biological Safety Cabinets Use of Personal Protective Equipment Proper Decontamination Waste Management Occupational Health Other Administrative Controls VIII. ROBUST RISK ASSESSMENT What are the benefits of a robust risk assessment? o Facilitate a risk assessment process; repeatable/reproducible o Facilitate risk mitigation decisions o Provide quality control documentation What are the properties of robust risk? o Takes into account all possible factors directly related to performing laboratory procedures involving biologically hazardous material o Details considered are specific to the agents, procedures, and other conditions in the laboratory Limitations of Robust Risk Assessment o The concept of “acceptable” risk. In just about every situation there will be an amount of risk that will need to be accepted and it is often up to the institution to determine the level of acceptable risk. o Cannot address factors not directly related to, but can affect, laboratory work: 5 Social (current events) Political (Management) Cultural (ethical issues) Personal Experience Financial (resources) It helps with selection of appropriate mitigation measures to reduce the likelihood and consequences of what? Expected Responses: Exposure, sickness, theft, diversion, misuse, accidents, incidents, mistakes, etc. A. RISK ACCEPTANCE Risk acceptance is how tolerable or acceptable a particular risk is to an institution, the community, or a person. Think about what acceptability is in the real world, and to focus on the potential differences between individuals, institutions, and communities. Accurately assigning risk levels can be honed with experience and a thorough understanding of the pathogens and procedures But perceiving risk as acceptable will ultimately depend on who will be at risk (risk owner) What is acceptable risk? o Technical risk assessments generally do not include perceived social, cultural, political, and ethical concerns. o Risk acceptance will depend on the ‘owner’ of the risk: risk averse or risk tolerant o Risk evaluation is largely in the eye of the beholder, whether it be an individual, institution, or a community. IX. RISK EVALUATION Unfortunately, there is no systematic way of evaluating risk and determining risk acceptability. This will depend on the perceptions of individuals, institutions, and the community. Risk Tolerant Drives investment decision in an institution. If an institution is particularly risk-averse, it will spend more resources attempting to reduce the risks it faces If a similar institution faces the same risk but is risk tolerant, it might proceed with procedures others may find too dangerous FIGURE 10. Risk evaluation FIGURE 11. Biosafety risk of direct exposure to individuals in the laboratory and to the community equal risk distribution The risk under this evaluation (star) is high to very high compared to the risk-Default graph, where it is listed as moderate. This evaluation puts higher emphasis on the overall risk. Consequently, many risk assessments will fall into the High to Very High category and may not be acceptable. A. RISK DISTRIBUTIONS TABLE 3. Differences between likelihood averse and consequence averse LIKELIHOOD AVERSE This scenario focuses more on the effects of likelihood on overall risk and the institution will be more focused on mitigation efforts used to decrease the likelihood of an incident For example – This institution would focus more on improving staff training, PPE usage, BSC certification etc CONSEQUENCE AVERSE This scenario focuses more on the effects of consequences on overall risk and the institution will be more focused on mitigation efforts used to decrease the consequences of an incident For example – This institution would focus on providing vaccination programs based on the risk of the agent they were working with The curves on the graph called “isoquants”, show the different levels of risk, from very low to very high. It is important to recognize that the precise locations of these isoquants on the graph are in fact arbitrary. This is the essence of risk evaluation. FIGURE 12. Risk Averse (L), Risk Tolerant (R) POC: DIMAANDAL | GONZALES, MEDIANISTA, TAMAYO 6 The risk under this evaluation (star) is in the Very Low category compared to the risk-default graph, where it is listed as moderate. This evaluation puts lower emphasis on the overall risk. Consequently, many risk assessments will fall into the Very Low category and will be considered acceptable. FIGURE 13. Risk Default (L), Risk Averse (M), Risk Tolerant (R) TABLE 4. Differences between risk averse and risk tolerant RISK AVERSE RISK TOLERANT A risk averse evaluation may come from an institution where very heavy fines may be impose if an incident were to occur, therefore a risk averse approach to biosafety and biosecurity is paramount A risk tolerant evaluation may come from an institution that has little regulation and may not adequately know or understand the likelihood and consequences of working with a particular agent, yet feels like the situation is under control and that risk is being accurately assessed and controlled X. BIORAM If a similar institution faces the same risk but is risk tolerant, it might proceed with procedures others may find too dangerous BioRAMs were designed for use by biorisk officers at laboratories and provide visualization of the relative risks and help to identify risk mitigation measures. BioRAM asks a series of questions o If the question contributes to risk, the score is 0-4 o If the question mitigates risk, the score is 4-0 BioRAM has embedded weights for the questions, and the categories of the questions XI. SUMMARY Hazard (threat) is a source that can cause harm Risk is the combination of the likelihood and consequences of an undesirable event related to a specific hazard (or threat) o R = f (L, C) Likelihood is the probability of an event occurring Consequences is the severity of an event Benefits of a robust risk assessment o Facilitates risk assessment process; repeatable/reproducible o Facilitates risk mitigation decisions o Provides quality control documentation XII. REFERENCES Dr. Tria’s PPT Lecture Batch 2021 Trans POC: DIMAANDAL | GONZALES, MEDIANISTA, TAMAYO 7 XIII.APPENDIX Pre-Analytical Phase MTB HAZARD ASSESSED RISK Patient walk in Vulnerable patients Infection MD assess px request DSSM/Xray Sputum collection/DSSM specimen obtained Incomplete data/assessment Insufficient volume/wrong specimen Repeat request or delayed proces Repeat submission of specimen/delayed process Transport to the lab Lost specimen/rined sample Repeat submission of specimen/delayed process LIKELIHOOD Exposure to infected patient Lack of appropriate trained staff at R&R Lack of trained personnel to collect sample Less likely interlaboratory/high if referred outside lab CONSEQUENCES Infection/depends on source of infected patient Repeat request/wrong test/delayed TAT Repeat request/wrong test/delayed TAT Patient complaints/legal lawsuit Pre-Analytical Phase MTB HAZARD ASSESSED RISK LIKELIHOOD Patient walk in Vulnerable patients Infection Exposure to infected patient MD assess px request DSSM/Xray Incomplete data/assessment Sputum collection/DSSM specimen obtained Insufficient volume/wrong specimen Transport to the lab Lost specimen/rined sample Analytical Phase Processing of Specimens Work on DSS/C&S of MTB NaOH mixed with sputum spx to break mucous 250 ml conical tube sputum spx solution + 15 ml water Centrifuge 3000x g 15 minutes Strive 50 ml H2O added to sediment to wash pellet Decant supernatant Selective growth medium agar in slant tube cultured small amount of pellet using application stick 7 weeks incubation Culture is smeared Head fix the slide/open flame sterilization Staining Repeat submission of specimen/delayed process Patient complaints/legal lawsuit Pathogen/old crack benchtop PPE worn occasionally/lab coats take home/inadequacy of resources Specimen mixed improperly/spillage or leakage of samples No sealed rotor or safety caps LAI (Lab Acquired Infection) Moderate Moderate LAI (Lab Acquired Infection) Moderate Moderate Air droplets transmission Moderate Moderate Aerosolization transmission Moderate Moderate Infrequent handwashing LAI (Lab Acquired Infection) Moderate Moderate Untreated lab waste/contamination of the environment LAI (Lab Acquired Infection) Moderate Moderate Inoculating loops old and rusty, open window ventilation Injury from loop and burns from Bunsen burners Moderate Moderate Cut/prick injury Moderate Moderate LAI (Lab Acquired Infection) Moderate Moderate High likelihood Severe Moderate Severe Breakage of glasswares Occasional/weekly cleaning of lab/no tarsh cans/improper handling of infectious waste Humid environment/limited and crowded lab space/improper ventilation Experimentation done through subcultures Susceptibility testing Improper drainage Validation of Test Results No vaccination and occupational health sx for personnel Inaccurate validation Releasing and reporting of test results Typographical error/clumsy staff Post Analytical Phase Repeat submission of specimen/delayed process Lack of appropriate trained staff at R&R Lack of trained personnel to collect sample Less likely interlaboratory/high if referred outside lab Based in the Pathogen Safety Data Sheet Aerosol generation Unsecured culture/no locks of lab storage/ref/equipment No personnel verification program Identification of MDR Titan Blue Repeat request or delayed proces CONSEQUENCES Infection/depends on source of infected patient Repeat request/wrong test/delayed TAT Repeat request/wrong test/delayed TAT Inhalation of toxic fumes/gas/LAI/contamination of the specimen LAI (Lab Acquired Infection) Exposure of pathgen to LAI Moderate Moderate Cause threat to bioterrorism Risk of pathogen survivability in environment Moderate Severe Moderate Moderate LAI (Lab Acquired Infection) Moderate Moderate Wrong results Low Less consequence Wrong results/patient’s complaints Low Less consequence APPENDIX A. Risk Assessment of MTB Scenario (MTB DSSM, Culture, and Sensitivity) POC: DIMAANDAL | GONZALES, MEDIANISTA, TAMAYO 8 MTB HAZARD ASSESSED RISK MITIGATION CONTROL MEASURES BIOSAFETY (BS) DRIVERS/BIOSECU RITY (BC) DRIVERS Vulnerable patients Incomplete data/assessment Insufficient volume/wrong specimen Infection Repeat request or delayed process Repeat submission of specimen/delayed process Repeat submission of specimen/delayed process Separate triage, OPD space Trained receptionist/nurse to assist MD Both Both E A Verification of samples by lab tech Both A Training of staff BS A Provide signages/PSDS Personnel training about pathogen/fix benchtop Proper PPE usage and training of staff/proper SOPS/PPE made available by the management Both BS A/S A/E BS A/S/P SOPS/Decontamination of the spillage BS S Aerosolization transmission Rotor safety caps provision of centrifuges BS E LAI (Lab Acquired Infection) BS S Injury from loop and burns from Bunsen burners Cut/prick injury SOPS/Decontamination/hand hygiene practices Proper waste management/ decontamination/PPE usage and training of staff Provision of electrical incinerator instead of Bunsen burner not to be used under BSC Replacement of plastic wares BS E/S BS E/S LAI (Lab Acquired Infection) Proper housekeeping SOPS BS S BSC/Fume hoods BS E/A/S BSC/Fume hoods BS E/A/S Exposure of pathogen to LAI Inventory of culture/safety caps Both E/A/S Cause threat to bioterrorism Risk of pathogen survivability in environment Background checks of personnel/PRM/Access control/MCA BC A Proper drainage provision BC E No vaccination and occupational health sx for personnel LAI (Lab Acquired Infection) Provision of regular medical checkup Both A Inaccurate validation Wrong results 2-3 signatories provided Lost specimen/ruined sample Based in the pathogen safety data sheet Pathogen/old cracked benchtop PPE worn occasionally/lab coats take home/inadequacy of resources Specimen mixed improperly/spillage or leakage of samples No sealed rotor/safety caps Infrequent handwashing Untreated lab waste/contamination of the environment Inoculating lobs old and rusty, open window ventilation Breakage of glassware Occasional/weekly cleaning of lab/no trash cans/improper handling of infectious waste Humid environment/limited and crowded lab space/improper ventilation Aerosol generation Unsecured culture/no locks of lab storage/ref/equipment No personnel verification program Improper drainage Typographical error/clumsy staff Legend: LAI (Lab Acquired Infection) LAI (Lab Acquired Infection) Air droplets transmission LAI (Lab Acquired Infection) Inhalation of toxic fumes/ gas/ LAI/ contamination of the specimen LAI (Lab Acquired Infection) Wrong results/patient’s complaints Personnel training/conduct client satisfaction survey APPENDIX B. Mitigation of MTB Scenario (MTB DSSM, Culture and Sensitivity) S Both E – Engineering control S – SOPS P – PPE A – Administrative Control BS – Biosafety BC – Biosecurity PRM – Personnel Reliability Management MCA – Material Control Accountability POC: DIMAANDAL | GONZALES, MEDIANISTA, TAMAYO CATEGORIES OF MITIGATION CONTROL 9 S/A