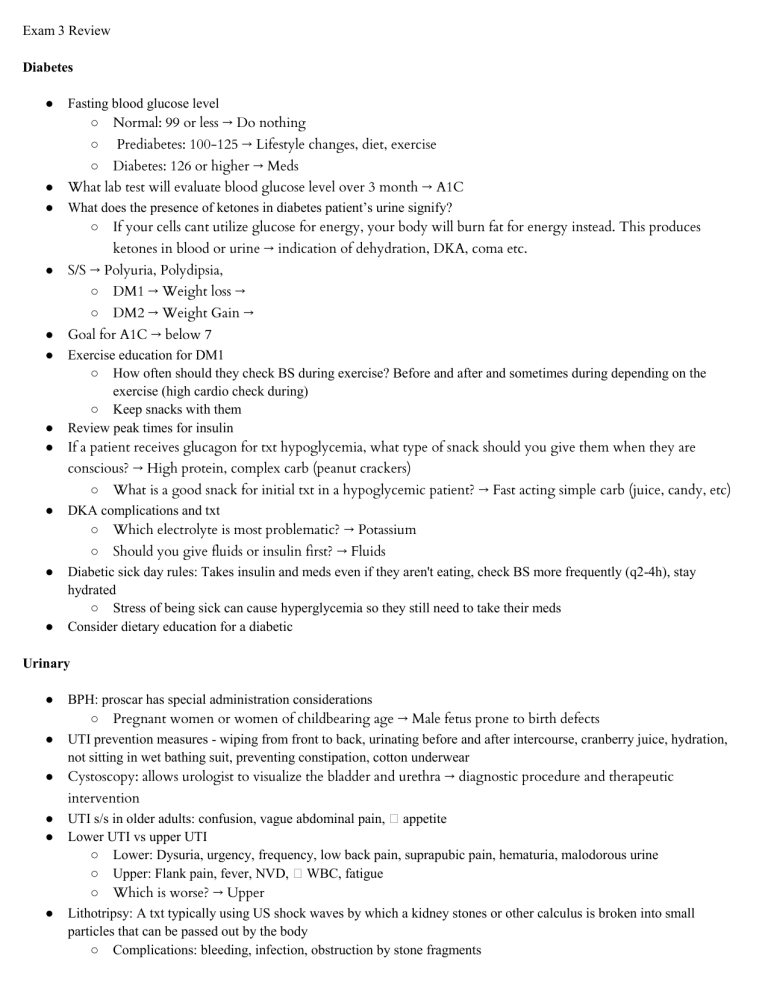
Exam 3 Review Diabetes ● ● ● Fasting blood glucose level ○ Normal: 99 or less → Do nothing ○ Prediabetes: 100-125 → Lifestyle changes, diet, exercise ○ Diabetes: 126 or higher → Meds What lab test will evaluate blood glucose level over 3 month → A1C What does the presence of ketones in diabetes patient’s urine signify? ○ If your cells cant utilize glucose for energy, your body will burn fat for energy instead. This produces ketones in blood or urine → indication of dehydration, DKA, coma etc. ● ● ● ● ● S/S → Polyuria, Polydipsia, ○ DM1 → Weight loss → ○ DM2 → Weight Gain → Goal for A1C → below 7 Exercise education for DM1 ○ How often should they check BS during exercise? Before and after and sometimes during depending on the exercise (high cardio check during) ○ Keep snacks with them Review peak times for insulin If a patient receives glucagon for txt hypoglycemia, what type of snack should you give them when they are conscious? → High protein, complex carb (peanut crackers) ● ● ● ○ What is a good snack for initial txt in a hypoglycemic patient? → Fast acting simple carb (juice, candy, etc) DKA complications and txt ○ Which electrolyte is most problematic? → Potassium ○ Should you give fluids or insulin first? → Fluids Diabetic sick day rules: Takes insulin and meds even if they aren't eating, check BS more frequently (q2-4h), stay hydrated ○ Stress of being sick can cause hyperglycemia so they still need to take their meds Consider dietary education for a diabetic Urinary ● ● ● ● ● ● BPH: proscar has special administration considerations ○ Pregnant women or women of childbearing age → Male fetus prone to birth defects UTI prevention measures - wiping from front to back, urinating before and after intercourse, cranberry juice, hydration, not sitting in wet bathing suit, preventing constipation, cotton underwear Cystoscopy: allows urologist to visualize the bladder and urethra → diagnostic procedure and therapeutic intervention UTI s/s in older adults: confusion, vague abdominal pain, � appetite Lower UTI vs upper UTI ○ Lower: Dysuria, urgency, frequency, low back pain, suprapubic pain, hematuria, malodorous urine ○ Upper: Flank pain, fever, NVD, � WBC, fatigue ○ Which is worse? → Upper Lithotripsy: A txt typically using US shock waves by which a kidney stones or other calculus is broken into small particles that can be passed out by the body ○ Complications: bleeding, infection, obstruction by stone fragments ● TURP: Transurethral resection of the prostate → treats BPH ○ Postop complications: hematuria, low UOP ○ How to obtain a urine sample from a catheter? → Port ● ● ● CAUTI → prevent by avoiding catheters and dc them asap Prevention for urinary incontinence: kegels, empty bladder regularly Kidney stone patient education: urine straining (helps determine stone type), how to prevent future occurrence, recommend 2-3 L of water Priority interventions for patient with kidney stone ○ Pain control ○ UOP ○ Hydration ● Pre/Post-Op ● ● ● ● ● ● ● ● Pre Op assessment: VS, height, weight, BS, consents, make sure concerns are addressed ○ Special considerations: some patients may need clearance from other providers prior to surgery depending on hx Normal UOP → at least 30mL/hr If patient has OSA and needs surgery, should they bring their home C-PAP → yes What meds should be held on the day of surgery? Blood thinners, Review obtaining consents ○ Need qualified hospital interpreter if they speak diff language After a patient returns from surgery, what should you assess first? → ABCs After general anesthesia, how long until the patient can drive? → 24 hrs If a patient has abdominal surgery and does not have adequate pain control, what complication are they at risk for? ○ Atelectasis: partial lung collapse → risk for pneumonia ○ ○ ○ What can we do to help w/ this? → Control their pain, turn cough deep breath q2h, incentive spirometer Early ambulation to prevent DVT How is diest advanced after surgery? ■ Ice chips, clear liquid, fulls, etc. Menopause, Osteoporosis, gender dysphoria ● ● ● ● ● ● ● Hormone replacement therapy for menopause: � risk for blood clots, � risk for osteoporosis Osteoporosis vs osteopenia ○ Penia → precursor Findings assc w/ menopause ○ Hot flashes, stop cycle, mood swings Post hysterectomy: early ambulation Measures to prevent osteoporosis - Ca + Vit D ○ What foods are high in vitamin D? ■ Milk, spinach, eggs How should patients take ca supplements? Divided doses to � absorption ○ Examples of weight bearing exercises: walking, running, weights, yoga, sports ■ NOT swimming or stationary bike ○ Risk factors for osteoporosis ( age (postmenopausal), gender (female), ethnicity (white, asian), meds (steroids, heparin), weight) ○ Diagnostics for osteoporosis: DEXA scan - at what age does screening start? 65 unless they are on steroids → screen early Review therapeutic communication techniques and gender dysphoria ○ ○ ○ ○ Example: gender identity disorder → patient may believe they were born as the wrong gender Associated conditions RF for gender dysphoria Therapeutic communication Fractures and Amputations ● ● ● ● ● ● ● ● ● Complications of Fx: fat embolism/venous embolism, compartment syndrome, infection, delayed health or malunion Traction: what is the purpose? Reducing muscle spasm, immobilizes, stabilizes Patient education during the first 24 hrs after fx or musculoskeletal injury: RICE Red flags for patient with a cast: unrelieved pain, paresthesia, pallor, pulses, paralysis ○ Remember neurovascular check ○ Compartment syndrome Plaster cast application: do you use fingers or palm when handling the cast while it is still wet? Palms ○ Fingertips could leave indents in the cast Intervention for phantom pain post amputation → mirror therapy Risk factors for amputation ○ trauma, osteomyelitis Post limb residual s/p amputation: don't use lotions and creams unless prescribed, prevention of contractures, compression wrapping/limb shrinking - figure 8 Measures to prevent contractures in LE amputations ○ Lay on their stomach for 30 min 3-4x a day