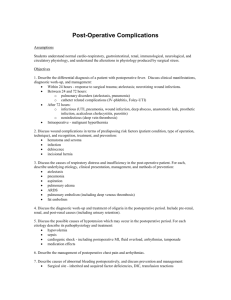
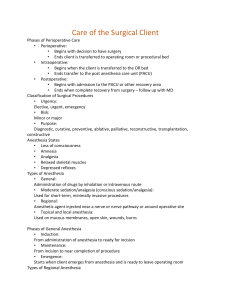
NURS 341: MedSurg Chapter 19 Post-operative Care Notes Postoperative Period Begins immediately after surgery o PACU is usually next to OR Limits transportation Gives ready access to anesthesia and OR staff Nursing care focus o Maintain patient safety o Identify actual and potential patient problems o Frequent assessment and monitoring is required o ECG and more intense monitoring required Initial recovery period in PACU (Post anesthesia care unit) Hand-off report, SBAR Goal to prepare pt to go back to floor or be discharged PACU Admission Report General information Patient history Intraoperative management (anesthesia, meds, Blood loss, Fluids, urine) Intraoperative course (unexpected events during procedure, VS trend, lab tests during procedure) Potential Postoperative Complications Postoperative Assessment…ABC Airway o Oxygenation and ventilation can be affected by residual neuromuscular blockade, use of opioids, and patient characteristics such as sleep-disordered breathing (e.g. central or obstructive sleep apnea [OSA], abnormal airway anatomy). o Patency o Artificial airway: Breathing o RR and quality: 12 to 20 BPM o Breath sounds: minimal amount of congestion is expected; Incentive Spirometer o Supplemental oxygen o Pulse oximetry (95% to 100%) and capnography (Amount of CO2 coming out of pts body): Confused, restless, check for respiratory distress; CO2 may remain in the body due to decrease in breathing Circulation o ECG monitoring o Vital signs o Peripheral pulses: Make sure blood is flowing evenly o Capillary refill: less than 3 seconds means circulation is good o Skin color and temperature: pink and warm are normal; cyanosis shows lack of oxygen, pale indicates blood loss and jaundice indicates issue with the liver; erythema: around incision site means infection Postoperative Assessment Neurologic o LOC/ Glasgow Coma Scale: AAO x3; Checks verbal, eyes, motor; highest is 15; Below 8 indicates comatose state o Orientation o Sensory and motor status. Hearing is the first sense to return, so be sure to explain all activities to the patient. o Pupil size, equality and reaction: Uneven pupils could mean brain death or cranial nerves not intact Genitourinary o Intake (IV fluids) o Output (urine and NG) o Estimated blood loss (EBL) Glascow Coma Scale Postoperative Assessment Gastrointestinal o Bowel sounds (check prior to eating) o NG—Verify placement to suction or clamped; if draining properly o Nausea Surgical site o Dressing…check for drainage or swelling under bandage; Purulent: infection Sanguinous: Red Serosanguinous: watery plasma and blood Pain o Incisional o Other Laboratory and diagnostic tests o Review results of ordered exams; lab results pre and post op should be almost the same Postoperative Complications Respiratory o Airway obstruction (check airway); o Hypoxemia (low oxygen concentration in blood) Atelectasis “lungs partially collapse” (incentive spirometer, cough, deep breath) Pulmonary edema (assess lungs): crackles o Aspiration (listen for cough when swallowing) o Bronchospasm (assess lungs): Wheezing heard o Hypoventilation (check pulse ox or capnography) Nursing Interventions to Prevent Respiratory Complications Proper patient positioning o Lateral “recovery” position: left side, top leg bent and forward o Once conscious—supine position Oxygen therapy Coughing and deep breathing: splinting (pillow to chest) Incentive spirometer o Sustained maximal inspiration (inhale deeply and hold breath, release) Change patient position every 1 to 2 hours Early mobilization Pain management Adequate hydration o Parenteral or oral Chest physical therapy (mobilizes secretions) Nursing Interventions to Prevent Respiratory Complications Splinting for coughing and deep breathing Incentive Spirometer Postoperative Complications…Fluid and Electrolytes Fluid overload: too much IV fluids Fluid deficit: too little fluid Electrolyte imbalances o Hypokalemia from urinary and gastrointestinal tract losses, and can affect contractility of the heart, as well as result in decreased cardiac output and tissue perfusion Acid-base imbalances o may be seen with patients who have irregular breathing patterns or respiratory depression associated with anesthesia Potassium and sodium switch places in the heart in order to create electrical current. When creating that electrical current heart pumps. Not enough potassium or potassium not switching creates a dysrhythmia Postoperative Complications… Cardiovascular Hypotension Caused by: hypoperfusion to vital organs unreplaced fluid and blood loss Hypertension Caused by: pain, anxiety, bladder distention, respiratory distress, hypothermia Dysrhythmias hypoxemia, hypercapnia, electrolyte and acid-base imbalances, circulatory instability, and preexisting heart disease, as well as hypothermia, pain, surgical stress, and many anesthetics VTE (can develop within hours) inactivity, body position, and pressure Syncope decreased cardiac output, fluid deficits, or defects in cerebral perfusion Nursing Interventions to Prevent Cardiovascular Complications…Vital Signs Frequent (every 15 min) Compare Notify surgeon/ACP (anesthesia care provider) if any of the following occur: o Systolic BP <90 mm Hg or >160 mm Hg o Pulse rate <60 or >120 beats/min o Pulse pressure (difference between systolic and diastolic BP) narrows. 40 to 60 is wnl. Increases with age. Hypotension normal pulse and warm, dry skin is usually related to residual vasodilating effects of anesthesia and needs continued observation. Hypotension with rapid or weak pulse and cold, clammy, pale skin may indicate impending hypovolemic shock and requires immediate treatment. Hypotension may indicate volume depletion. Assess surgical site to determine if excessive bleeding is the cause of volume loss or hypotension. IV fluid boluses will be given to normalize BP. Hypertension may indicate pain. Administer pain medications as prescribed. Hypertension may indicate need for BP meds. May need to administer BP medications. Patient may have been NPO and may not have taken daily regimen of medications. Monitor for orthostatic BP with increase in mobility o Check BP when moving from positions of sitting standing or laying Continuous ECG monitoring (dysrhythmias) o Low O2? Adequate fluid replacement Assess surgical site for bleeding Intake and output Monitor laboratory results o Chem, H/H (Hemoglobin and Hematocrit), BUN, CR (check renal function) VTE prophylaxis (sc heparin): give blood thinner Slow changes in body position Early ambulation: to prevent VTE Postoperative Complications…Neurologic/Psychologic Emergence delirium (restlessness, disorientation, thrashing, and agitation) Delayed emergence (failure to regain consciousness 30 to 60 min after sx) Postoperative cognitive dysfunction (memory loss and inability to concentrate for weeks or months) Anxiety/Depression (grieving for a lost body part or function). Increased likelihood of complications. Alcohol withdrawal delirium (restlessness, insomnia, nightmares, irritability, and auditory or visual hallucinations) Nursing Interventions to Prevent Neuropsychologic Complications Monitor oxygen levels with pulse oximetry Oxygen therapy Pain management Reversal agents (Phase I): especially with delayed emergence Assess for anxiety and depression Alcohol protocols: last for days; will be hallucinating Safety Fluid/Electrolyte Balance Nutrition Sleep Listening Postoperative Complications…Pain and Discomfort Physiologic factors o Irritation of skin and underlying tissues by incision and retraction during surgery o Reflex muscle spasms o Positioning during surgery o Placement of various tubes Psychologic factors o Anxiety o Fear Other sources o Coughing and deep breathing after sx o Ambulating after sx o Shivering o Nausea, Vomitting Nursing Interventions to Prevent Pain and Discomfort Behavioral modalities o Develop a plan for pain control o Patient teaching regarding how to report pain and how it will be managed postop Single modalities o Med Multimodal analgesia o Two or more analgesics, given by various routes, with different mechanisms of action (opioid and nonsteroidal anti-inflammatory) Patient-controlled analgesia (PCA) o Self control for immediate pain relief o Pt can not overmedicate; maximum dosage during a o Certain time frame is implemented to prevent OD Epidural analgesia o Directly into spinal cord to pain receptors o Constant circulating level of pain med Complementary and alternative therapy o Music, Accupuncture, exercise, herbal supplements Postoperative Complications…Temperature Hypothermia o Less than 96.8F o Contributing factors: skin exposure during the surgical procedure, use of cold irrigants, d skin preparations, unwarmed inhaled gases. Shivering o Can increase resting energy expenditure and oxygen consumption, carbon dioxide production o Increased heart rate, BP, and intracranial pressure, contribute to significantly affect the patient’s comfort level. Fever o Infection? What kind? Who do you tell-Surgeon, ACP? Malignant hyperthermia (MH) )can be genetic) o Rapid rise in core body temperature to 105°F (40.5°C) or higher and severe muscle contractions, as well as tachycardia, hypercarbia (increased CO2), metabolic and respiratory acidosis, myoglobinuria, and elevated creatine kinase levels after receiving general anesthesia. o MH is a life-threatening complication that most often occurs during general anesthesia, but may also be seen in the 1-hour period immediately following surgery. Nursing Interventions to Prevent Hypothermia and Fever Passive warming Active warming Oxygen therapy…shivering? Opioids Meticulous asepsis Airway clearance…Coughing/deep breathing Dantrolene (Dantrium) for Malignant Hyperthermia Postoperative Complications… Gastrointestinal Check Bowel sounds. May be decreased, but not absent. Exception…abdominal sx for a couple of hours, but must continue to monitor for return Nausea/Vomiting Postop (PONV) Constipation o Risk factors: use of Opioids/meds, change in diet and fluid intake, immobility Postoperative ileus o Impairment of gastrointestinal (GI) motility o Risk factors: use of opioids, immobility, old age, after intraabdominal or nonabdominal surgery. o Characterized by bowel distention, lack of bowel sounds, accumulation of GI gas and fluid, and delayed passage of flatus and stool Hiccups o Phrenic nerve irritated after sx by gastric distention or intestinal obstruction Nursing Interventions to Prevent GI Complications PONV o NPO, IV fluids, clear liquids o Antiemetics/Prokinetics: Nausea o Alternative therapy: Oils, herbals Adequate hydration Assess bowel sounds/check for flatulence Early mobilization Postoperative Complications… Urinary o Retention (800-1500mL/24 hrs) o Oliguria (<400mL/24 hrs) o Anuria (<100ML/24 hrs) o Catheter-associated urinary tract infection (CAUTI) o Average urine output: 0.5mL/kg/hr Nursing Interventions to Prevent Urinary Complications Monitor urine output: Input is equal to output Adequate hydration Normal positioning for elimination No void? Palpate Bladder; distension Bladder scan/straight catheter per orders Remove urinary catheter when no longer indicated Postoperative Complications… Surgical Site Infection (SSI) Surgical site infection (SSI)…Contamination of the wound from the following: Exogenous flora (environment and skin) Oral flora (usually to lungs) Intestinal flora High Risk: immunosuppressed, malnourished, older, traumatic injury, bowel sx, accumulation of fluid in the wound, diabetes, colitis, alcoholism Normally after 3rd postop day Signs: Local: red, swelling, increase pain Systemic: fever, leukocytosis (white blood cells elevated) Nursing Interventions to Prevent Surgical Site Infection (SSI) and Wound Problems Assess the wound o Many surgeons prefer to change the first postoperative dressing, but nurse should be there to document appearance; red first day; red/yellow day 2+ o Note drainage color, consistency, and amount o Assess effect of position changes on wound/drain tube drainage . May indicate accumulation of drainage associated with an infection o Signs/symptoms of infection o Administer antibiotics or probiotics as ordered o Maintain glycemic control. Hyperglycemia can contribute to risk for wound infection Other Wound problems… (Not medical emergency) Wound dehiscence o Surgical incision reopens either internally or externally. It tends to happen most often within two weeks of surgery and following abdominal or cardiothoracic procedures. Notify surgeon Wound evisceration o Surgical incision opens (dehiscence) and the abdominal organs then protrude or come out of the incision (evisceration). Cover the wound with a saline soaked gauze and notify surgeon o Wound Problems Discharge from PACU Criteria Patient awake (or neurologically at baseline) Vital signs at baseline or stable No excess bleeding or drainage (more than 50mL in 15 minutes) No respiratory depression Oxygen saturation greater than 92% Pain managed Nausea and vomiting controlled Pt safe to discharge SBAR Report given to nurse [floor or ECF] or instructions given to pt if discharged When back on hospital unit, encourage c, db, is, ambulate, medicate before getting OOB for first time, check bowel sounds before eating or drinking. o Ambulatory Surgery Discharge criteria o All PACU discharge criteria met o No IV opioids in past 30 minutes o Able to tolerate fluids o Voided o Able to ambulate, if not contraindicated; o Responsible adult present to drive patient home o Written discharge instructions given and understood Ambulatory Surgery…Discharge Teaching o Provided to patient and caregiver o Specific to type of surgery and anesthesia used o Care of incision(s) and dressings o Actions and side effects of any medications o Activities allowed and prohibited o Dietary restrictions and modifications o Symptoms that should be reported o Where and when to return for follow-up care o Reasons to seek help after discharge o Answers to questions Common reasons to seek help after discharge o Unrelieved pain o Questions about medications o Wound drainage and/or bleeding o Increased drainage from a drainage device o Fever greater than 100°F Gerontologic Considerations …Postoperative Patient Decreased respiratory function Altered vascular function Drug toxicity…slows elimination of drugs Mental status changes (confusion, memory loss, etc)…anesthesia concerns Pain control PREOP HERBS Herbal Supplements and Surgery Ginseng can increase BP before and during surgery Garlic, Vitamin E, Ginko and Fish Oil can increase bleeding Kava and valerian can cause excessive sedation