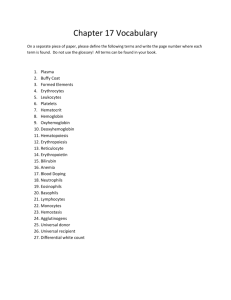
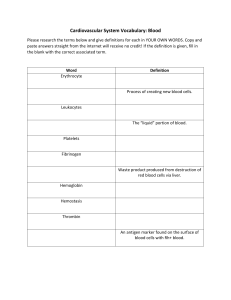
CHAPTER I : INTRODUCTION HEMATOLOGY 1 GEORGINA ANGELINE G. BELO, R.M.T. HEMATOLOGY - the discipline that studies the development and diseases of blood, is an essential medical science. In this field, the fundamental concepts of biology and chemistry are applied to the medical diagnosis and treatment of various disorders or diseases related to or manifested in the blood and bone marrow. - Basic procedures performed in the hematology laboratory, such as the complete blood cell count (CBC), which includes the measurement and examination of red blood cells (erythrocytes), white blood cells (leukocytes), and platelets (thrombocytes), and the erythrocyte sedimentation rate (ESR), frequently guide the primary care provider in establishing a patient’s differential diagnosis. Molecular diagnostics, flow cell cytometry, and digital imaging are modern techniques that have revolutionized the laboratory diagnosis and monitoring of many blood disorders, for example, acute leukemias and inherited blood disorders. The field of hematology encompasses thestudy of blood coagulation––hemostasis and thrombosis. HEMATOLOGY • Medical laboratory scientists, medical laboratory technicians, laboratory assistants, and phlebotomists employed in the hematology laboratory play a major role in patient care. The assays and examinations that are performed in the laboratory can do the following: ■ Establish a diagnosis or rule out a diagnosis ■ Confirm a physician’s clinical impression of a possible hematological disorder ■ Detect an unsuspected disorder ■ Monitor the effects of therapy ■ Detect minimal residual disease following therapy Although the CBC is the most frequently requested procedure, a laboratory professional must be familiar with the theory and practice of a wide variety of automated and manual tests performed in the laboratory to provide quality patient care. Continuing education is a necessity to keep up with continually changing knowledge and instrumentation in the fi eld. HISTORY The first scientists, such as Athanasius Kircher in 1657, described “worms” in the blood, and Anton van Leeuwenhoek in 1674 gave an account of RBCs, but it was not until the late 1800s that Giulio Bizzozero described platelets as “petites plaques.” The development of the Wright stain by James Homer Wright in 1902 opened a new world of visual blood film examination through the microscope. Although automated analyzers now differentiate and enumerate blood cells, Wright’s Romanowsky-type stain (polychromatic, a mixture of acidic and basic dyes), and refinements thereof, remains the foundation of blood cell identification. In the present-day hematology laboratory, RBC, WBC, and platelet appearance is analyzed through automation or visually using 5003 to 10003 light microscopy examination of cells fixed to a glass microscope slide and stained with Wright or Wright-Giemsa stain . The scientific term for cell appearance is morphology, which encompasses cell color, size, shape, cytoplasmic inclusions, and nuclear condensation. A. DEFINITION OF TERMS / PREFIXES POIKILOCYTOSIS POIKILO irregular/varied NORMOCYTIC NORMOCHROMIC ANEMIA B.CHARACTERISTICS OF BLOOD PHYSICAL CHARACTECTERISTICS OF BLOOD: ❑Denser and more viscous than water ❑Feels slightly sticky ❑Temperature of blood is 38C (100.4F) ❑Slightly alkaline pH ranging from 7.35 to 7.45 ❑Color of varies with its oxygen content ❑Blood constitutes about 20% of extracellular fluid ❑8% of the body total body mass ❑Blood volume is 5 to 6 LITERS average sized adult – MALE ❑4 to 5 LITERS an average sized adult -FEMALE Formed Elements and Sizes REACTIVE LYMPHOCYTES C. FUNCTIONS OF BLOOD - Blood is a liquid connective tissue that our body uses for may different functions - Blood transports oxygen from lungs to tissues; clears tissues of carbon dioxide; transports glucose, proteins, and lipids; and moves wastes to the liver and kidneys. - The liquid portion is plasma, which, among many components, provides coagulation enzymes that protect vessels from trauma and maintain the circulation. Plasma transports and nourishes blood cells. There are three categories of blood cells: red blood cells (RBCs), or erythrocytes; white blood cells (WBCs), or leukocytes; and platelets (PLTs), or thrombocytes. Hematology is the study of these blood cells. By expertly staining, counting, analyzing, and recording the appearance, phenotype, and genotype of all three types of cells, the medical laboratory professional is able to predict, detect, and diagnose blood diseases and many systemic diseases that affect blood cells. Physicians rely on hematology laboratory test results to select and monitor therapy for these disorders; consequently, a complete blood count (CBC) is ordered on nearly everyone who visits a physician or is admitted to a hospital. D. COMPOSITION 1 Whole blood includes erythrocytes, leukocytes, platelets, and plasma. When a.) specimen is centrifuged, leukocytes and platelets make up the buffy coat (small white layer of cells lying between the packed red blood cells and the plasma). 2. Plasma is the liquid portion of unclotted blood. Serum is the fluid that remains after coagulation has occurred and a clot has formed. a.) Plasma is composed of 90% water and contains proteins, enzymes, hormones, lipids, and salts. b.) Plasma normally appears hazy and pale yellow (contains all coagulation proteins), and serum normally appears clear and straw colored (lacks fibrinogen group coagulation proteins). COMMON TYPE OF BLOOD SERUM E. RED BLOOD CELLL METABOLISM The mature erythrocyte is a biconcave disc with a central pallor that occupies the middle one-third of the cell. In the mature cell, the respiratory protein, hemoglobin, performs the function of oxygen–carbon dioxide transport. Throughout the life span of the mature cell, an average of 120 days, this soft and pliable cell moves with ease through the tissue capillaries and splenic circulation. As the cell ages, cytoplasmic enzymes are catabolized, leading to increased membrane rigidity (density), phagocytosis, and destruction. ERYTHROPOIESIS - production. term used to describe the process of erythrocyte Erythropoiesis - Erythropoiesis encompasses differentiation from the hematopoietic stem cell (HSC) through the mature erythrocyte. - To streamline their functional capacity, erythrocyte precursors shed most organelles and produce prodigious amounts of hemoglobin, which eventually comprises approximately 95% of the total cellular protein. Erythropoiesis is regulated partially by the combined actions of cytokine signaling pathways and transcription factors. - Hematopoiesis begins with the development of primitive erythrocytes in the embryonic yolk sac, continues in extramedullary organs such as the liver in the developing fetus, and is ultimately located in the red bone marrow during late fetal development, childhood, and adult life. • Transport of oxygen to the tissues and transport of carbon dioxide from the tissues are accomplished by the HEME pigment in hemoglobin, which is synthesized as the erythrocyte matures. The basic substances needed for normal erythrocyte and hemoglobin production are amino acids (proteins), iron, vitamin B12, vitamin B6 , folic acid (a member of the vitamin B2 complex), and the trace minerals cobalt and nickel. • In adult humans, the daily production of more than 200 billion erythrocytes requires more than 20 mg of elemental iron. The vast majority of this iron comes from the recycling of senescent erythrocytes by macrophages of the mononuclear phagocytic system; only 1 to 2 mg of the daily iron supply derives from intestinal absorption, which at a steady state is sufficient only to replace iron lost by epithelial cell sloughing and functional and dysfunctional bleeding. Abnormal erythropoiesis can result from deficiencies of any of these necessary substances. Defective erythropoiesis is frequently seen in underdeveloped countries where protein deficiencies are common. Other types of anemias can be caused by deficiencies in vitamin B12, folic acid, or iron. ERYTHROPOIETIN • The substance erythropoietin is produced primarily by the kidneys. Peritubular cells are the probable site of synthesis in the kidneys. Extrarenal organs such as the liver also secrete this substance. Ten to fifteen percent of erythropoietin production occurs in the liver, which is the primary source of erythropoietin in the unborn. This glycoprotein hormone, with a molecular weight of 46,000, stimulates erythropoiesis and can cross the placental barrier between the mother and the fetus. Erythropoietin was the first human hematopoietic growth factor to be identified. The gene for erythropoietin is located on chromosome 7 • Erythropoietin has its predominant effect on the committed erythroid cells, colony-forming unit-erythroid (CFU-E), promoting their proliferation and differentiation into erythroblasts. It may also stimulate the differentiation of a more primitive erythroid progenitor, the burstforming unit-erythroid (BFU-E), in association with so-called burst promoting activity. Erythropoietin prevents erythroid cell APOPTOSIS. APOPTOSIS – programmed cell death Recombinant human erythropoietin • produced from mammalian cells and was originally used in patients being treated with dialysis who had anemia due to chronic renal failure. In addition to possible uses in the treatment of various types of anemia, recombinant human erythropoietin is likely to be useful in a broad range of clinical applications. ERYTHROCYTES MATURATION Erythrocytes are rapidly maturing cells. Once the stem cell differentiates into the erythroid cell line, a cell matures through the nucleated cell stages in 4 or 5 days. Bone marrow reticulocytes have an average maturation period of 2.5 days. Once young reticulocytes enter the circulating blood, they remain in the reticulocyte stage for an average of 1 day and represent approximately 0.5% to 1.5% of the circulating erythrocytes. Rubriblast (Pronormoblast) The rubriblast or pronormoblast has an overall diameter of approximately 12 to 19 mm. The nuclear-to-cytoplasmic (N:C) ratio is 4:1. The large, round nucleus contains from zero to two nucleoli, is usually dark appearing, and has a fine chromatin pattern. The cytoplasm stains a distinctive blue (basophilic) color with Wright stain and lacks granules. The distinctive blue color reflects the RNA activity needed to produce the protein required for hemoglobin synthesis. Studies with radioactive iron have demonstrated that most of the iron destined for hemoglobin synthesis is taken into the cell at this stage. Prorubricyte (Basophilic Normoblast) • The second stage, the prorubricyte or basophilic normoblast, has an overall cell diameter of 12 to 17 mm and is only slightly smaller than the rubriblast. The N:C ratio remains high (4:1); however, this stage demonstrates morphological evidence of increasing maturity. The nuclear chromatin becomes more clumped. Nucleoli are usually no longer apparent. The cytoplasm continues to appear basophilic with a Wright stain. This cell contains no evidence of the pink color that indicates hemoglobin development. Metarubricyte (Orthochromic Normoblast) • The rubricyte matures into the metarubricyte or orthochromic normoblast. The overall cell is smaller (8 to 12 mm). The chromatin pattern is tightly condensed in this maturational stage and can be described as pyknotic (dense or compact). In the later period of this stage, the nucleus will be extruded from the cell. The metarubricyte is characterized by an acidophilic (reddish pink) cytoplasm. This coloration indicates the presence of large quantities of hemoglobin. Three mitoses are believed to occur in the 2- to 3-day interval between the rubriblast and the end of the metarubricyte stage. Two thirds of these mitoses have been shown to occur in the rubricyte stage. After this stage, the cell is no longer able to undergo mitosis RETICULOCYTE • The reticulocyte stage is the next maturational stage. Part of this phase occurs in the bone marrow, and the later part of the stage takes place in the circulating blood. This cell demonstrates a characteristic reticular appearance caused by remaining RNA if stained with a supravital stain, such as new methylene blue. In a Wright-stained blood smear, young reticulocytes with a high amount of RNA residual have a blue appearance, which is referred to as polychromatophilia. The overall cellular diameter ranges from 7 to 10 mm. This cell is anuclear. • As the erythrocyte develops, the nucleus becomes more and more condensed and is eventually lost. After the loss of the nucleus, an immature erythrocyte (reticulocyte) remains in the bone marrow for 2 to 3 days before entering the circulating blood. During this period in the bone marrow and during the first day in the circulation, this immature erythrocyte is referred to as a reticulocyte. • Although the reticulocyte lacks a nucleus, it contains various organelles, such as mitochondria, and an extensive number of ribosomes. The formation of new ribosomes ceases with the loss of the nucleus in the late metarubricyte; however, while RNA is present, protein and heme synthesis continues. During reticulocyte maturation, the RNA is catabolized, and the ribosomes disintegrate. The loss of ribosomes and mitochondria, along with full hemoglobinization of the cell, marks the transition from the reticulocyte stage to full maturation of the erythrocyte. • Under normal conditions, the quantity of reticulocytes in the bone marrow is equal to that of the reticulocytes in the circulating blood. To maintain a stable reticulocyte pool in the circulation, the bone marrow replaces the number of erythrocytes that have reached their full life span. Because the normal life span or survival time is 120 days, 1/120th of the total number of erythrocytes is lost each day, and an equal number of reticulocytes is released into the circulation. • If, under the stimulus of erythropoietin, increased numbers of young reticulocytes are prematurely released from the bone marrow because of such conditions as acute bleeding, these reticulocytes are referred to as stress or shift reticulocytes. This situation is analogous to the appearance of immature leukocytes in the peripheral blood during the stress of infection ERYTHROCYTE • Mature Erythrocyte After the reticulocyte stage, the mature erythrocyte is formed. This cell has an average diameter of 6 to 8 mm. The survivability of erythrocytes can be determined by using radioactive chromium (51Cr). A shortened life span can be observed in the hemolytic. REFERRENCE : • • • • Rodak’s HEMATOLOGY ; CLINICAL PRINCIPLES AND APPLICATIONS TURGEON HEMATOLOGY 5TH EDITION GOOGLE IMAGES HEMATOLOGY TEXTBOOK