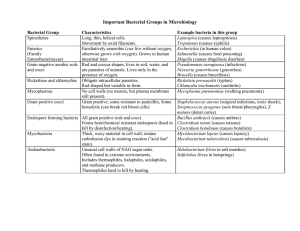
Gram positive
Clostridium: spore-forming, tetani , difficile, botulinum, obligate anaerobes
Bacillus: anthracis (endospores)
Staphylococcus spp.: facultative anaerobes
Staphylococcus aureus
Streptococcus pyogenes
Streptococcus pneumoniae: capsule
Lactobacilli
Diphtheroids
Bacillus anthrax: spore-forming
Gram negative
Pseudomonas aeruginosa: grow in disinfectants
Salmonella: typhi, facultative anaerobes
Vibrio: cholerae
Chlamydia pneumoniae: atypical
Acinetobacter baumannii
Enterobacteriaceae: E. coli (facultative anaerobes), klebsiella
Proteus
Legionella pneumophila: gram - rod, non spore-forming
Mycobacterium tuberculosis: waxy cell wall, mycolic acid, acid-fast bacillus, aerobes, capsule, in
macrophage; atypical, escape phagocytosis
Opportunistic infection
Acinetobacter baumannii
Pseudomonas aeruginosa
Enveloped viruses: HIV, SARS, MERS, retrovirus, Hep B, H5N1, rubies, pertussis
Non-enveloped viruses: polio, norovirus, adenovirus, Hep A, rhinovirus, rotavirus, norovirus,
adenovirus
Fungi
Cryptococcus neoformans: meningitis
Aspergillus fumigatus: respiratory system, mold; aspergillosis
Pneumocystis jirovecii: PCP, pneumocystis pneumonia
Parasites
Entamoeba histolytica, cryptosporidium spp., giardia lamblia: contaminated water
Trichomonas vaginalis: protozoan
Plasmodium falciparum: malaria, protozoa
Clonorchis sinensis
Liver fluke
Live attenuated: measles, mumps, rubella, varicella (MMRV)
Toxoids: tetanus, diphtheria, formaldehyde
Component: strep. Pneumoniae, acellular pertussis
Subunit
Viral vector: adenovirus, spike
Killed: polio, Hep A, rabies, pertussis (whooping cough)
B cells: immunoglobulins; Y-shaped, binds to complement/ phagocyte
IgA: mucosal surface
IgM: first antibody produced after exposure, short life span
IgD: signal B cells to become active
IgE: attach to mast cells, important in allergic reactions e.g. hay fever/ parasitic infection
IgG: most abundant antibody, long term protection; pass from mother to foetus
Antigen-antibody complex -> thru antigenic determinants
1. Opsonization: antibody surrounding antigen for phagocytosis
2. Complement activation: complement attach to antibody on cell surface
3. Neutralisation: prevent binding with mucosa; bind with toxin’s active site
4. Agglutination
T helper cells/ CD4
1. Type 1 Th1: secrete interferon gamma: phagocytosis: T cells and phagocytes
2. Type 2 Th2: interleukins, eosinophils and mast cells: parasitic infection
3. Follicular T cells: activate B cells -> antibody
4. Regulatory T cells: regulate cytotoxicity
Minimum inhibitory concentration MIC
Disk diffusion test (Kirby Bauer test)
Cefoxitin: indicator for MRSA
Trimethoprim-sulfamethoxazole: very effective
Bacillus spp., staphylococcus aureus, ~streptococcus pyogenes, E coli: beta haemolytic
Macconkey agar: only works for gram negative
Lactose fermenters: E coli, klebsiella -> pink-red
Non-lactose fermenters: proteus, salmonella, pseudomonas aeruginosa -> yellow
Narrow-spectrum: penicillin G, vancomycin, macrolides
Broad-spectrum: tetracycline, chloramphenicol, carbapenams
Metronidazole: bacteroides fragilis, clostridium difficile
Gastric ulcers: helicobacter pylori
Prophylaxis: gynaecological, bowel surgery
Mycobacterium tuberculosis: hide in macrophages
Rifampicin, isoniazid, pyrazinamide
Intrinsic resistance
Pseudomonas aeruginosa
Gram negative: resistance, cannot cross the outer membrane e.g. vancomycin (peptidoglycan
crosslinking)
Acquired antibiotic resistance
Horizontal gene transfer
Conjugation: bridge/ sex pilus
Transformation: taking free DNA from dead bacteria, recombination
Transduction: from a bacteria to bacteriophage
Degrading, enzymatic destruction, beta-lactamase
Penicillinase, cephalosporinases, carbapenemase
Expelling: efflux pump, ejection, transmembrane protein
MDR
Gram + cocci
M methicillin RSA, VI (intermediate) SA,VRSA, VRE enterococci
Gram - rods
MDR acinetobacter baumannii
MDR pseudomonas aeruginosa
Enterobacteriaceae (E. coli, Klebsiella, proteus): ESBL, carbapenem
-> colistin: targets LPS and phospholipid
Antifungal drugs
Nystatin: thrush by candida albicans
Amphotericin B: broad spectrum, systemic fungal infection
Antiviral
Acyclovir: varicella, shingles, herpes simplex
Microbiota on
1. Skin, scalp, groin and perineum, feet: staphylococcus epidermidis (harmless), S. aureus
(not typical, 20% people have it), diphtheroids, candida albicans (yeast, like moist, only
found e.g. in the vaginal area, between toes, underarm)
2. Intestine: bacteroides (anaerobes, wound and surgery: abdominal/ intestinal infections),
{E. coli, Klebsiella, proteus: from the same big family}, enterococcus, clostridium:
anaerobes, spore-formers, candida albicans
3. Vagina: lactobacilli, candida albicans, UTI
4. Nose: S. epidermidis, diphtheroids
5. Mouth: viridans streptococci (very harmless, CV infections), candida albicans, anaerobes
6. Teeth: streptococcus mutans (tooth decay, mutans means like sugar), viridans
streptococci, candida albicans
7. Throat: viridans streptococci, streptococcus pneumoniae (deep infection in the lungs,
with capsule, can escape phagocytosis), neisseria species (diplococci, very harmless for
young people, passes as droplets)
8. Lungs: pneumocystis jirovecii (yeast, some people have this, HIV/ AIDS may get
infection from this)
Endogenous infection
E. coli: UTI
Bloodstream infections: Staph epidermidis (catheter)
Viridans streptococci: mouth, tooth, throat
Candida albicans: mouth, vagina, skin
Staphylococcus epidermidis: skin, nose
Diphtheroids: skin, nose
Bleach: corrosive
Lysol: toxic and corrosive
Bleaching water: inactivated by blood, faecal material
Cidex, glutaraldehyde: stable for 4-6 weeks
Disinfectants cannot kill
Pseudomonas aeruginosa
Mycobacterium tuberculosis
Hepatitis viruses
Fungal spores
Bacterial endospores
Alcohol
Chlorhexidi
ne
Iodophors
Glutaralde
hyde
Sodium
hypochlorite
Quaternary
ammonium
compound
Bacteria
✓
✓
✓
✓
✓
✓
Fungi
✓
✓
✓
✓
✓
✓
Lipophilic
virus
✓
✓
✓
✓
✓
✓
✓?
✓
✓
✓
Some ✓
Non-envel
oped virus
Spore
✓
TB
✓
Hepatitis
viruses
Residual
activity
uses
✓
✓
✓
✓
✓
Hand rub
Handwash,
bath
-
✓
preoperativ
e
Fibre optic
endoscope
Wipes, no
toxic
residual
Corrodes
Pungent
Corrodes,
inactivated
by organic
matter
environmen
t
Sterilisation
1. Autoclaving
15 psi x 15 min x 121 degree celsius; denaturation of cell membrane, bacterial protein
and nucleic acid, except thermophiles
2. Hot air oven: 170 60-90 min
3. Ethylene oxide gas, alkylating agent, cross-linking of DNA and proteins, non-corrosive,
55 4-12hrs, plastic, syringe
4. Upper room germicidal ultraviolet irrigation (UGVI): thymine dimer, airborne
240-280nm, retina injury, skin burn
5. Filtration: separated not killed; solution, 0.22hm bacteria 0.025hm virus; millipore filter
HEPA: smaller than 0.3hm bacteria, 2 min, OT, ICU
Biofilm: staphylococcus epidermidis
Viruses: bleach and cidex (glutaraldehyde)
Prions: CJD, bovine spongiform encephalopathy
NaOH then autoclave 134-136 8 min; protease
-release enzyme: Clostridium botulinum: botox; collagenase, protease
-exotoxins: clostridium tetani; tetanus toxin, neurotoxin
-enterotoxins: vibrio cholerae; cholera toxin
-endotoxin: LPS, endotoxic shock, septicaemia
Incubation period: infection to clinical symptoms
Convalescent period: infectious after recovering
Asymptomatic: neisseria meningitidis (meningococcus), streptococcus pneumoniae,
staphylococcus aureus, MRSA
STD:
Treponema pallidum: syphilis
Neisseria gonorrhoeae: gonorrhoeae
Herpes simplex II: genital herpes
Mother to foetus: direct contact, vertical transmission, rubella, HIV
Droplet: larger than 5um; pertussis
Airborne: smaller than 5um; measles, TB, chicken pox
Arthropod-borne: flavivirus (dengue fever, enveloped), plasmodium falciparum
Zoonoses
Avian flu: H5N1, enveloped
Anthrax: bacillus anthracis, form endospore, gram + rods
Rhinovirus, rotavirus, norovirus, adenovirus: not enveloped
Clostridium tetani: gram + rod, endospore forming, exotoxin (neurotoxin)
Legionella pneumophila: gram - rod, non spore-forming
Plasmodium falciparum: malaria, protozoa
Rabies virus; rhabdovirus, bullet-shaped
Lecture 1
Flagellum: only in rods, motility
Capsule: evasion, slippery, polysaccharide coat, negative stain using indian ink
Pilus/ fimbriae: attachment
Endospores: survival, dipicolinic acid
Atypical: no cell wall; mycoplasma pneumoniae, chlamydia pneumoniae, legionella pneumophila
Gram stain:
Procedure: heat fix -> crystal purple > iodine > alcohol > safarnin
Positive: purple, thick peptidoglycan wall
Negative: pink/ red, thin peptidoglycan wall, LPS
NO: mycobacterium tuberculosis (waxy cell wall, mycolic acid, acid-fast bacillus),
Ziehl-Neelsen stain: carbol fuchsin -> acid alcohol > methylene blue
Spore stain: malachite green -> safarnin
Obligate aerobes: P Aeruginosa, acinetobacter baumannii
Microaerohile: campylobacter jejuni, helicobacter pylori
Facultative anaerobes: staphylococcus spp., Escherichia coli, Salmonella
Obligate anaerobes: clostridium
Virus: virion
Capsid: helical and icosahedral
Envelop: lipid and polysaccharide
Obligate intracellular parasite
Virus replication
1. Attachment
2. Penetration: endosome/ vesicle in cell
3. Uncoating
4. Replication by RNA synthesis: RNA molecules, capsomere (subunit of capsid), spike
5. Assembly
6. Release
Prions: CJD, bovine spongiform encephalopathy, chronic wasting disease
Inherited and transmissive spongiform encephalopathy
Dungi: yeasts (asexual budding), mold; eukaryotes
Dimorphic fungi
Hyphae
Superficial fungi: dermatophytes
Systemic fungi: systemic mycoses
Cryptococcus (fungi) neoformans; cryptococcosis, latent-living, cryptococcal meningitis
(meninges)
Candidas albicans (thrush), tetracycline; candidas auris
Aspergillus fumigatus: respiratory system, mold; aspergillosis
Pneumocystis jirovecii: PCP, pneumocystis pneumonia
Ringworm
Sequence of infection
1.
2.
3.
4.
5.
6.
Attachment/ adhesion
Penetration
Replication
Damage to tissue
Spread
cure/ death
Immune system
Immunity
Non-specific immune response; innate
First line of defence: external
skin; dry and acidic; vagina: 4.5; skin: 5.6
Mucus membrane:
secretions, saliva, at trachea: mucus goblet cells secrete mucins, a kind of glycoprotein; ciliated
columnar cells -> mucociliary escalator
(saliva, gastric juice, sweat: high salt concentration),
Gastrointestinal tract: extreme pH, immunoglobulin (IgA) antibody: for immune function of
mucous membrane, neutralises many pathogens
Urinary system: washing action during voiding of urine, slightly acidic, lysosomes
Vagina: lactobacilli (normal flora), produce lactic acid from glycogen, slightly acidic
Eye (conjunctiva), nasal secretion & saliva: lysosomes, washing action, immunoglobulins in
tears
Second line of defence:
Phagocytes: internal (macrophages in tissues and neutrophils in blood, shorter life span then
marcophages, highly motile, basophils, dendritic cells, eosinophils)
High number of phagocytes in the lungs
Dendritic cells: antigen-presenting cells, part of the antigen on the cell membrane, on skin,
mucous membranes and lymphoid tissues
Kupffer cells in liver, microglia in nerve tissues
Natural killer cells,
Chemicals: cytokines, interferons, interleukins, complement proteins
Inflammation and fever
Neutrophils: polymorphonuclear neutrophils, polymorphs, can change to another form; highly
motile; engulfer and killer of bacteria
Phagocytosis: streptococcus pneumoniae (capsule); mycobacterium tuberculosis (waxy cell
wall)
Natural killer cells: virus infection (virus-infected cells), cancer cells
Mediate cytotoxicity, secrete cytokines, IFNgamma, TNFalpha,
Third line of defence
Humoral immune system: B cells and T cells
Cellular/cell-mediated immune system: T cells
The endpoint of phagocytosis and digestion in a macrophage is the presentation of the antigen
on its surface -> beginning of the specific immune recognition
Specific immune response, third line of defence; adaptive
Humoral immunity (antibody): B & T cells
Cell-mediated immunity: T cells
PAMPs: pathogen-associated molecular patterns
Viral envelope protein: some viruses are covered in an envelope
Peptidoglycan: cytoplasmic membrane in most of the bacteria
Lipopolysaccharide on the cell wall of gram negative bacteria
Resistant: mycobacterium tuberculosis and staphylococcus pneumoniae
Natural killer cells
-lymphocytes
-both innate (viral infection and tumorigenic cells)
and adaptive immune response
-mediate cytotoxicity, secrete cytokines e.g. interferons
Phagocytosis
1. Chemotaxis
2. Attachment
3. Ingestion -> form phagosome
4. Lysosome combine with phagosome -> phagolysosome
Eosinophils: anti-parasitic, fungal infection, inflammation, allergies,
Basophils: inflammation and allergies
Mast cells: similar to basophils (originate from putative mast cell precursor)
Inflammatory response
-itis
Non-specific response to injury, tissue damage, infections
Histamines: vasodilation
Symptoms:
1. Redness
2. Swelling: edema, increase in plasma flow to the site
3. Pain
4. Heat
5. Pus: purulent (containing pus) exudate, consists of live and dead phagocytes
Inflammation
-formation of fibrin, lead to fibrosis: occludes the lymphatic vessels -> limit the spread of
pathogens
-abscess
-some TB organisms: hide in macrophages and cause chronic inflammation
Soluble mediators: cytokines, prostaglandins (responsible for both promotion and resolution of
inflammation, NSAIDs), leukotrienes
Cytokines: interferons, interleukins, tumour necrosis factor, chemokines, lymphokines, some
growth factor)
Alpha and beta interferons: viral infection, attach to an infected cells and induce them to make
antiviral proteins
Gamma interferons: to stimulate the phagocytic activity of neutrophils and macrophages
Fever
-Hypothalamus: pyrogens
Complement system: innate immunity
Plasma proteins, enzymatic cascade system; opsonization: make pathogens more susceptible
to phagocytosis
Factor C1 to C9
Classical, alternative, and lexin: cellular lysis, destruction of the pathogen
Interferons
Type I interferons: alpha and beta; viral infection
Type II interferons: gamma; phagocytosis
T cells: sets of glycoproteins, CD
B cells: immunoglobulins; Y-shaped, binds to complement/ phagocyte
IgA: mucosal surface
IgM: first antibody produced after exposure, short life span
IgD: signal B cells to become active
IgE: attach to mast cells, important in allergic reactions e.g. hay fever/ parasitic infection
IgG: most abundant antibody, long term protection; pass from mother to foetus
Antigen-antibody complex -> thru antigenic determinants
1. Opsonization: antibody surrounding antigen for phagocytosis
2. Complement activation: complement attach to antibody on cell surface
3. Neutralisation: prevent binding with mucosa; bind with toxin’s active site
4. Agglutination
T helper cells/ CD4
1. Type 1 Th1: secrete interferon gamma: phagocytosis: T cells and phagocytes
2. Type 2 Th2: interleukins, eosinophils and mast cells: parasitic infection
3. Follicular T cells: activate B cells -> antibody
4. Regulatory T cells: regulate cytotoxicity
Cytotoxic cells/ CD8 cells
Secrete cytotoxic granules: apoptosis; antigen-presenting cells
Immunological memory: memory lymphocytes
Immunological tolerance, major histocompatibility complexes (MHCs), autoimmune disease
Live attenuated
Toxoids: tetanus, diphtheria
Component
Subunit
Viral vector: adenovirus, spike
Primary immunodeficiency: severe combined immunodeficiency disease
Secondary immunodeficiency: rheumatoid arthritis, systemic lupus erythematosus (attack DNA
and RBCs)
Anaphylaxis, anaphylactic shock, hypersensitivity
HIV-> AIDS: attack cells with CD4 receptors, destroy T cells in lymph nodes
Antiretroviral therapy ART
Live attenuated: measles, mumps, rubella, varicella (MMRV)
Killed: polio, Hep A, rabies, pertussis (whooping cough)
Toxoid: formaldehyde
The endpoint of phagocytosis and digestion in a macrophage is the presentation of the antigen
on its surface -> beginning of the specific immune recognition
Specific immune response, third line of defence; adaptive
Humoral immunity (antibody): B & T cells
Cell-mediated immunity: T cells
PAMPs: pathogen-associated molecular patterns
Viral envelope protein: some viruses are covered in an envelope
Peptidoglycan: cytoplasmic membrane in most of the bacteria
Lipopolysaccharide on the cell wall of gram negative bacteria
Resistant: mycobacterium tuberculosis and staphylococcus pneumoniae
Natural killer cells
-lymphocytes
-both innate (viral infection and tumorigenic cells)
and adaptive immune response
-mediate cytotoxicity, secrete cytokines e.g. interferons
Phagocytosis
1. Chemotaxis
2. Attachment
3. Ingestion -> form phagosome
4. Lysosome combine with phagosome -> phagolysosome
Eosinophils: anti-parasitic, fungal infection, inflammation, allergies,
Basophils: inflammation and allergies
Mast cells: similar to basophils (originate from putative mast cell precursor)
Inflammatory response
-itis
Non-specific response to injury, tissue damage, infections
Histamines: vasodilation
Symptoms:
1. Redness
2. Swelling: edema, increase in plasma flow to the site
3. Pain
4. Heat
5. Pus: purulent (containing pus) exudate, consists of live and dead phagocytes
Inflammation
-formation of fibrin, lead to fibrosis: occludes the lymphatic vessels -> limit the spread of
pathogens
-abscess
-some TB organisms: hide in macrophages and cause chronic inflammation
Soluble mediators: cytokines, prostaglandins (responsible for both promotion and resolution of
inflammation, NSAIDs), leukotrienes
Cytokines: interferons, interleukins, tumour necrosis factor, chemokines, lymphokines, some
growth factor)
Alpha and beta interferons: viral infection, attach to an infected cells and induce them to make
antiviral proteins
Gamma interferons: to stimulate the phagocytic activity of neutrophils and macrophages
Fever
-Hypothalamus: pyrogens
Complement system: innate immunity
Plasma proteins, enzymatic cascade system; opsonization: make pathogens more susceptible
to phagocytosis
Factor C1 to C9
Classical, alternative, and lexin: cellular lysis, destruction of the pathogen
Interferons
Type I interferons: alpha and beta; viral infection
Type II interferons: gamma; phagocytosis
T cells: sets of glycoproteins, CD
B cells: immunoglobulins; Y-shaped, binds to complement/ phagocyte
IgA: mucosal surface
IgM: first antibody produced after exposure, short life span
IgD: signal B cells to become active
IgE: attach to mast cells, important in allergic reactions e.g. hay fever/ parasitic infection
IgG: most abundant antibody, long term protection; pass from mother to foetus
Antigen-antibody complex -> thru antigenic determinants
5. Opsonization: antibody surrounding antigen for phagocytosis
6. Complement activation: complement attach to antibody on cell surface
7. Neutralisation: prevent binding with mucosa; bind with toxin’s active site
8. Agglutination
T helper cells/ CD4
5. Type 1 Th1: secrete interferon gamma: phagocytosis: T cells and phagocytes
6. Type 2 Th2: interleukins, eosinophils and mast cells: parasitic infection
7. Follicular T cells: activate B cells -> antibody
8. Regulatory T cells: regulate cytotoxicity
Cytotoxic cells/ CD8 cells
Secrete cytotoxic granules: apoptosis; antigen-presenting cells
Immunological memory: memory lymphocytes
Immunological tolerance, major histocompatibility complexes (MHCs), autoimmune disease
Live attenuated
Toxoids: tetanus, diphtheria
Component
Subunit
Viral vector: adenovirus, spike
Primary immunodeficiency: severe combined immunodeficiency disease
Secondary immunodeficiency: rheumatoid arthritis, systemic lupus erythematosus (attack DNA
and RBCs)
Anaphylaxis, anaphylactic shock, hypersensitivity
HIV-> AIDS: attack cells with CD4 receptors, destroy T cells in lymph nodes
Antiretroviral therapy ART
Live attenuated: measles, mumps, rubella, varicella (MMRV)
Killed: polio, Hep A, rabies, pertussis (whooping cough)
Toxoid: formaldehyde
Antimicrobials
Selective toxicity
Therapeutic dose: LD:ED lethal:effective
Narrow-spectrum: penicillin G, vancomycin, macrolides
Broad-spectrum: tetracycline, chloramphenicol, carbapenams
Synergy
E.g. sulphonamides and trimethoprim (bacteriostatic)
Septrin and cotrimoxazole
Antagonism: penicillin and tetracycline
Folic acid: nucleic acid
Carbapenems: meropenem, ertapenem, imipenem -> very strong antibiotics
Vancomycin: MRSA, developing resistance, gram +
Metronidazole: bacteroides fragilis, clostridium difficile
Gastric ulcers: helicobacter pylori
Prophylaxis: gynaecological, bowel surgery
Mycobacterium tuberculosis: hide in macrophages
Rifampicin, isoniazid, pyrazinamide
Intrinsic resistance
Pseudomonas aeruginosa
Gram negative: resistance, cannot cross the outer membrane e.g. vancomycin (peptidoglycan
crosslinking)
Acquired antibiotic resistance
Horizontal gene transfer
Conjugation: bridge/ sex pilus
Transformation: taking free DNA from dead bacteria, recombination
Transduction: from a bacteria to bacteriophage
Degrading, enzymatic destruction, beta-lactamase
Penicillinase, cephalosporinases, carbapenemase
Expelling: efflux pump, ejection, transmembrane protein
MDR
Gram + cocci
M methicillin RSA, VI (intermediate) SA,VRSA, VRE enterococci
Gram - rods
MDR acinetobacter baumannii
MDR pseudomonas aeruginosa
Enterobacteriaceae (E. coli, Klebsiella, proteus): ESBL, carbapenem
-> colistin: targets LPS and phospholipid
Antifungal drugs
Nystatin: thrush by candida albicans
Amphotericin B: broad spectrum, systemic fungal infection
Antiviral
Acyclovir: varicella, shingles, herpes simplex,
Antibiotic stewardship
Prevent development of antibiotic resistant strain, reduce side effect, reduce cost
Prophylaxis
Intestinal surgery
Dirty wounds
Dental extraction, heart valve abnormalities
Human microbiota
Vagina: lactobacilli; metabolise glycogen, on the membrane lining of the vagina, ferment and
produce lactic acid, pH 4.5
Disinfection and sterilisation
Critical items: catheter (cardiac, urinary), implants, surgical instruments, ultrasound probes used
in sterile body cavity
Semi-critical items: gastrointestinal endoscopes, laryngoscopes, bronchoscopes, using
glutaraldehyde
Cleaning
Lyse blood, to prevent blood protein clotting by heat during sterilisation
80% m/os
Detergent
Ultrasonic cleaning: dislodge organic debris
Disinfection
Vomit, faeces, blood, organic matter
Prevent cross-infection
Non-invasive, contact with mucous membrane
Always cleaned first
Pseudomonas aeruginosa: grow in disinfectant
Kill vegetative microbes not spores
Heat
In water: bedpans, linen
Hot water at least 5 min
Washer-disinfectors
Disinfectants: not toxic, effective, broad spectrum, non corrosive, fast acting, odourless, cheap,
easy to prepare
Bleach: corrosive
Lysol: toxic and corrosive
Bleaching water: inactivated by blood, faecal material
Cidex, glutaraldehyde: stable for 4-6 weeks
Disinfectants cannot kill
Pseudomonas aeruginosa
Mycobacterium tuberculosis
Hepatitis viruses
Fungal spores
Bacterial endospores
Antiseptics
On skin; prevent cross-contamination, before insertion of intravascular device
Antisepsis: alcohol (hand rub); chlorhexidine (preoperative bath); iodophors (pre surgery)
Alcohol: can kill enveloped viruses, fungi, TB by denaturing protein; ethyl/ isopropyl alcohol
No: non-enveloped viruses, hepatitis viruses
Chlorhexidine gluconate: gram +
Residual activity: damage cell membrane, leakage of cytoplasmic content
No: TB, spores, some viruses
Iodophors: bacteria, fungi, virus
Betadine: non-staining, non-irritating
No: cannot use on silicone catheter, corrode metals, inactivated by organic materials
Disinfectants
Glutaraldehyde, cidex in pH 7.5-8.5: alkylating agent, alter RNA, DNA, protein synthesis
All form of microbial life
For fibre optic endoscopes, do not corrode
Sodium hypochlorite: virus, fungi, bacteria, TB. some endospores
fast-acting, no toxic residue
Corrodes, inactivated by organic matter
Quaternary ammonium compound: enveloped (lipophilic) virus, fungi, bacteria
Environmental sanitization, residual activity
Alcohol
Chlorhexidi
ne
Iodophors
Glutaralde
hyde
Sodium
hypochlorite
Quaternary
ammonium
compound
Bacteria
✓
✓
✓
✓
✓
✓
Fungi
✓
✓
✓
✓
✓
✓
Lipophilic
virus
✓
✓
✓
✓
✓
✓
✓?
✓
✓
✓
Some ✓
✓
✓
✓
✓
Non-envel
oped virus
Spore
TB
✓
✓
Hepatitis
viruses
Residual
activity
uses
-
✓
Hand rub
Handwash,
bath
✓
preoperativ
e
Fibre optic
endoscope
Wipes, no
toxic
residual
Corrodes
Pungent
Corrodes,
inactivated
by organic
matter
environmen
t
Sterilisation
6. Autoclaving
15 psi x 15 min x 121 degree celsius; denaturation of cell membrane, bacterial protein
and nucleic acid, except thermophiles
7. Hot air oven: 170 60-90 min
8. Ethylene oxide gas, alkylating agent, cross-linking of DNA and proteins, non-corrosive,
55 4-12hrs, plastic, syringe
9. Upper room germicidal ultraviolet irrigation (UGVI): thymine dimer, airborne
240-280nm, retina injury, skin burn
10. Filtration: separated not killed; solution, 0.22hm bacteria 0.025hm virus; millipore filter
HEPA: smaller than 0.3hm bacteria, 2 min, OT, ICU
Biofilm: staphylococcus epidermidis
Viruses: bleach and cidex (glutaraldehyde)
Prions: CJD, bovine spongiform encephalopathy
NaOH then autoclave 134-136 8 min; protease
1.
2.
3.
4.
5.
6.
7.
Acquisition
Adhesion
Penetration
RNA/ DNA synthesis/ multiplication
Damage to tissues
Spread to other cells
Cure of death
Pathogenicity is measured by virulence.
Virulence: ratio disease: exposed
Virulence factor: pili, capsule, flagella, extracellular enzymes, exotoxins, ability to convert to
endospore
-release enzyme: Clostridium botulinum: botox; collagenase, protease
-exotoxins: clostridium tetani; tetanus toxin, neurotoxin
-enterotoxins: vibrio cholerae; cholera toxin
-endotoxin: LPS, endotoxic shock, septicaemia
Chain of infection
Infectious agent -> reservoir -> portal of exit -> mode of transmission -> mode of entry -> host
Host susceptibility
Reservoir: where the pathogen is naturally found, may not be the source (depends on the mode
of transmission)
Salmonella typhi: typhoid fever
Incubation period: infection to clinical symptoms
Convalescent period: infectious after recovering
Asymptomatic: neisseria meningitidis (meningococcus), streptococcus pneumoniae,
staphylococcus aureus, MRSA
Fomite: inanimate objects that carry and spread infectious agent
Zoonotic: from animal to human
STD:
Treponema pallidum: syphilis
Neisseria gonorrhoeae: gonorrhoeae
Herpes simplex II: genital herpes
Mother to foetus: direct contact, vertical transmission, rubella, HIV
Droplet: larger than 5um; pertussis
Airborne: smaller than 5um; measles, TB, chicken pox
Arthropod-borne: flavivirus (dengue fever, enveloped), plasmodium falciparum
Zoonoses
Avian flu: H5N1, enveloped
Anthrax: bacillus anthracis, form endospore, gram + rods
Rhinovirus, rotavirus, norovirus, adenovirus: not enveloped
Clostridium tetani: gram + rod, endospore forming, exotoxin (neurotoxin)
Legionella pneumophila: gram - rod, non spore-forming
Plasmodium falciparum: malaria, protozoa
Rabies virus; rhabdovirus, bullet-shaped