Perinatal Mental Health Care: Essay on Postpartum Depression
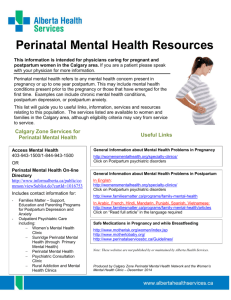
advertisement

Nava 1 Natasha Nava Walls ENG 111 April 1, 2021 Perinatal Mental Health Care Thesis: Providing psychological assistance to mothers who experience these needs to become common practice among health care providers when bringing their children in for their well child visits after birth. I. Perinatal care is an essential part of a woman’s mental health. a. What is perinatal care b. How is it essential and why? II. Pregnancy should be the most exciting time in a woman’s life, but yet some women struggle with finding their glow and the excitement everyone talks about. a. Discuss mental health occurrences b. Hormones/changes to the brain III. Two major postpartum mental health diseases are postpartum blues and postpartum depression. a. Discuss blues and depression after birth and what is the difference IV. After having a baby one should be happy, joyful, proud that they brought this new life into the world, yet for some reason, they are the exact opposite. a. What is depression b. Symptoms Nava 2 V. A decrease in cognitive performance in children has been reviewed and has begun to show a link to postpartum depression a. Language development b. Anxiety c. ADHD VI. Postpartum blues and depression are not the only mental health issues that can arise after having a child a. Anxiety b. PTSD c. Panic attacks d. OCD VII. Another of the unfortunate mental health issues that can arise in the postpartum period is postpartum psychosis. a. Discuss what it is VIII. Another devastating disorder associated with perinatal mental health is suicide a. Discuss where it comes from and how it is now on provider’s radar IX. Hair is a mess, clothes are piled up on the floor because the hamper is over loaded, balled up tissues are next to the trash from nights of crying from so much worrying and sadness. a. Provide survey results on mother’s and their actual feelings on the subject b. How do they feel things would have changed if they were asked by their doctor how they were doing? Nava 3 X. The mother isn’t the only one that is affected after the birth of a child. a. Discuss the spouse’s perspective XI. Once it is identified that there is a mental health crisis occurring it is vital that treatment is started within two to six weeks so that the mental illness cannot progress further to an unsafe level. a. Discuss different treatment types and their affects b. Include types of support XII. When a mother takes their child to the doctor for their regular checkups after birth the doctor always asks about how the child is doing but it is not common practice to ask mom or dad how they are doing. a. Discuss interview with Suzie b. Provider’s input XIII. Conclusion. Tie everything together. Nava 4 Natasha Nava Walls ENG 111 April 1, 2021 Perinatal Mental Health Care Most women find pregnancy and motherhood a wonderful and enjoyable experience. For some women though, this can be such a life changing event that it will result in mental illnesses to include anxiety and depression. Providing psychological assistance to mothers who experience these needs to become common practice among health care providers when bringing their children in for their well child visits after birth. Perinatal care is an essential part of a woman’s mental health before and after birth. According to Maria Noonan author of Family Physicians Perceived Role In Perinatal Mental Health: An Integrative Review the perinatal period is best described as the time for a mother and infant immediately before birth and the first 12 months after birth (2). This is an essential time for a mother and a child as this is the period when a mother bonds with her child. Noonan also describes the perinatal period as a “recognized time of significant risk for development, relapse or recurrence of mental health problems” (2). Mothers who have previously had mental disorders are at an increased risk of worsening their condition postpartum. The perinatal period can also be referred to in two separate parts, prenatal and postpartum. Pregnancy should be the most exciting time in a woman’s life, yet some women struggle with finding their glow and the excitement everyone talks about. According to Agnes Higgins author of There is more to perinatal mental health care than depression: Public health nurses reported engagement and competence in perinatal mental health care “It is estimated that 15%- Nava 5 25% of women will experience a mental health problem during or post pregnancy, either as a new problem or a reoccurrence of a pre-existing problem” (https://pubmed.ncbi.nlm.nih.gov/28771981/) Hormones are often responsible for and the major contributing factor for when it comes to mental health during pregnancy. Research has shown that during pregnancy biological changes occur in a women’s brain. Neurotransmitters in the brain are altered and this in turn can impact a women’s ability to regulate her emotions. Two major postpartum mental health diseases are postpartum blues and postpartum depression. Some may not understand the difference between them though. According to Adele Viguera, MD author of Postpartum Blues “The postpartum blues develop in roughly fifty percent or more of women within a week of delivery” (UptoDate). Some of the many symptoms of mild depression include things such as loss of interest in everyday things, insomnia, loss of energy and diminished ability to think or concentrate. This can develop into major depression when the continue for more than four weeks postpartum. After having a baby one should be happy, joyful, proud that they brought this new life into the world, yet for some reason, they are the exact opposite. Once a mother gets past the fourweek window and she continues to feel depressed she has now began showing signs of postpartum depression. According to Dr. Wenzel who is a contributor to the book by Rebecca Fox Starr, Beyond the Baby Blues Anxiety and Depression During and After Pregnancy “Depression affects approximately 9% to 13% of pregnant women” (25). As described by Dr. Viguera postpartum depression is classified as “depressed mood most of the day and nearly every day, diminished interests or pleasure in almost all activities, significant weight loss or gain without diet, agitation, insomnia or hypersomnia nearly every day, diminished ability to think or concentrate nearly everyday and recurrent thoughts of death” (UptoDate). Many mothers who Nava 6 are affected by postpartum depression tend to have previous mental health illnesses prior to becoming pregnant. A decrease in cognitive performance in children has been reviewed and has begun to show a link to postpartum depression. In a study that was cited by Adele Viguera, author of Postpartum depression: Risks of cognitive impairment and psychopathology in the children analyzed 296 mothers and their children and found “that language development was poorer in the infants of mothers who were depressed at both assessments, compared with infants of mothers who were not depressed at each assessment” (UptoDate). Dr. Viguera also goes on to describe how children are at an increased risk of developing anxiety and attention deficit hyperactivity disorder, or ADHD. A mother who is depressed can unintentionally be causing delays to her child because of her own mental illness. This shows that our emotions can ultimately have an impact the others around us. Postpartum blues and depression are not the only mental health issues that can arise after having a child. Pregnant women can also suffer from anxiety, post-traumatic stress disorder, panic attacks, obsessive behaviors and other psychopathological disorders not mentioned. Anxiety is one of the most common that usually coincides with depression. The main things that women worry about when having anxiety during the postpartum time are fear of loosing their child to other diseases like sudden infant death, lack of support from their spouse or family members and inadequacy of being a good mother. All of these can be a root cause to a mother’s anxiety in the perinatal period. Another of the unfortunate mental health issues that can arise in the postpartum period is postpartum psychosis. This is often seen in patients who have been clinically diagnosed with bipolar disorder, but this can also occur in women with major depression with psychosis or even Nava 7 schizophrenia. Jennifer Payne, MD author of Postpartum psychosis: Epidemiology, Pathogenesis, Clinical Manifestations, Course, Assessment And Diagnosis summarizes the “rapid onset of psychotic symptoms includes hallucinations and delusions, bizarre behavior, confusion, and disorganization that may appear to be delirium” (UptoDate). Dr. Payne also mentions “Postpartum psychosis, which is considered the most severe mental health problem in the puerperium, is estimated to affect one or two women per 1,000 births across all cultures” (UptoDate). Psychosis can be very debilitating for a mother to go through as often they can lose touch with reality. Another devastating disorder associated with perinatal mental health is suicide. As explained by Louise M. Howard and Hind Khalifeh authors of Perinatal Mental Health: A Review Of Progress And Challenges “Suicide risk in the perinatal period is drastically increased in women with moderate to severe mental illness as compared with mothers with no psychiatric history” (3). Although suicide does not occur without a precursor mental illness it does account for a type of perinatal mental illness that is becoming more noticed in the eye of medical professionals. Hair is a mess, clothes are piled up on the floor because the hamper is over loaded, balled up tissues are next to the trash from nights of crying from so much worrying and sadness. During the survey conducted to support this paper it was asked of thirty mothers how they felt their mental health was during the perinatal period. Sixteen admitted feeling some form of depression during the postpartum period. Twelve admitted to having anxiety during that same time. Seven admitted having some form of anxiety and depression during their pregnancy. One mother admitted to having a psychosis episode that required hospitalization for twelve days at three months post-partum. Only 10 of the mothers admitted to their child’s provider checking on their mental health status during the well child visits. Twenty-two of these mothers felt that it would Nava 8 be beneficial for doctors to check on the parents when having visits with their children and that this should become a normal practice. Eight of the mother’s felt that it would not have made a difference in their health if a doctor checked on them sooner. The mother isn’t the only one that is affected after the birth of a child. Many forget that the father has also now has had his world shaken up by a new child arriving in the world. When babies are in their mother’s stomachs, they hear their heartbeat and their voice. Something they come to know and find comfort in before they are even born. They have already started to bonded with their mother. You can see this when a baby cries, the mother picks him or her up and then they are soothed. However, when the father or other parent picks them up they struggle to get them to calm down as they just have not created that bond yet. This can take a toll mentally on a father if they are not prepared for that reaction. This can also cause depression or anxiety among the fathers. He could feel he isn’t connected, that his child would not love him or even the fact that he is doing something wrong. If left unchecked by a medical professional, a father’s mental health can easily spiral out of control and become a severe illness. Ensuring his mental health is followed up on as well during a child’s wellness visit could really be beneficial for all. Once it is identified that there is a mental health crisis occurring it is vital that treatment is started within two to six weeks so that the mental illness cannot progress further to an unsafe level. As discussed in the book by Rebecca Fox Starr “A positive social support system is crucial for a woman who is recovering from any form of perinatal distress. Support can come in many forms, including a woman’s spouse or partner, friends, children, therapist, family members, doctors, doulas, lactation consultants, support groups, online forums, and psychopharmacologists” (91) Various types of support and assistance are available to parents in Nava 9 the postpartum time outside of those mentioned above. For certain diagnosis parents can undergo a variety of interventions like cognitive behavior therapy, pharmacological interventions, or couple’s therapy. Cognitive behavior therapy is explained as helping a person work through making changes in their lives to better deal with their mental illnesses by different exercises that involve talking and even physical exercises. Pharmacological interventions can include different classes of medications based on which mental illness is the target. Couple’s therapy can help mothers and fathers learn to adjust to being new parents or even repeat parents together by talking through things as to keep from feeling overwhelmed or triggering further mental illnesses. When a mother takes their child to the doctor for their regular checkups after birth the doctor always asks about how the child is doing but it is not common practice to ask mom or dad how they are doing. Suzie Shibla, DNP, FNP-BC stated “Screening parents at their children’s wellness visits is essential as a family practitioner because you are not only taking care of the children but the family as well. Mentally unwell parents cannot care for their children to the best of their abilities.” A survey completed to support this paper asked fifteen medical doctor’s their thoughts on if it was important to screen parents during well child visits. All agreed that it was highly important. Seven providers mentioned they routinely make it common practice to follow up with the mother at follow up visits but only 2 mentioned also following up with the fathers. Many times, parents forget to take care of themselves because they are so focused on their kids. Identifying, diagnosing, and treating a child’s parents at the earliest sign of a mental disorder is essential to help the child grow. Making this a normal part of a child’s wellness visit with their medical provider should become a standard for all medical doctors for the safety and wellbeing of the parents and the children. Nava 10 Work Cited Brockington, Ian, et. al. “An International Position Paper On Mother-infant (Perinatal) Mental Health, With Guidelines For Clinical Practice” Springerlink.com https://link.springer.com/content/pdf/10.1007/s00737-016-0684-7.pdf Accessed 4 April 2021 Higgins, Agnes, et. al. “There is more to perinatal mental health care than depression: Public health nurses reported engagement and competence in perinatal mental health care” John Wiley & Sons Ltd 2017 https://pubmed.ncbi.nlm.nih.gov/28771981/ Accessed 12 April 2021 Howard, Louise and Khalifeh, Hind “Perinatal Mental Health: A Review Of Progress And Challenges” World Psychiatry October 2020 https://onlinelibrary.wiley.com/doi/epdf/10.1002/wps.20769 Accessed 10 April 2021 Fox Starr, Rebecca Beyond the Baby Blues Anxiety and Depression During and After Pregnancy Rowman & Littlefield 2018 Nava, Natasha “The Physician’s input and suggestions” Survey Completed 9 April 2021 Nava, Natasha “Prenatal and Postnatal Mental Concerns” Survey Completed 16 April 2021 Noonan, Maria, et. al. “Family Physicians Perceived Role In Perinatal Mental Health: An Integrative Review” BMC Family Practice 2018 https://link.springer.com/content/pdf/10.1186/s12875-018-0843-1.pdf Accessed 7 April 2021 Payne, Jennifer, Medical Doctor “Postpartum psychosis: Epidemiology, pathogenesis, clinical manifestations, course, assessment, and diagnosis” 27 February 2018 https://www.uptodate.com/contents/postpartum-psychosis-epidemiology-pathogenesis- Nava 11 clinical-manifestations-course-assessment-anddiagnosis?search=postpartum%20anxiety&source=search_result&selectedTitle=7~150& usage_type=default&display_rank=7 UptoDate Accessed 23 April 2021 Shibla, Suzan, Doctor of Nursing Practice, Family Nurse Practitioner Board Certified. Personal Interview by Natasha Nava 23 April 2021 Taylor, Billie Lever, et. al. “How Do Women’s Partners View Perinatal Mental Health Services? A Qualitative Meta-synthesis” Division of Psychiatry, University College London 30 August 2017 https://discovery.ucl.ac.uk/id/eprint/1572314/1/Morant_Lever%20Taylor%20et%20al%2 02017%20accepted.pdf Accessed 12 April 2021 Viguera, Adele, Medical Doctor “Postpartum Blues” UptoDate 22 Feburary 2021 https://www.uptodate.com/contents/postpartumblues?search=post%20partum%20unipolar%20depression:%20prevention&topicRef=107 697&source=see_link Accessed 22 April 2021 Viguera, Adele, Medical Doctor “Postpartum unipolar depression: Prevention” UptoDate 9 December 2019 https://www.uptodate.com/contents/postpartum-unipolar-depressionprevention?search=post%20partum%20unipolar%20depression:%20prevention&source= search_result&selectedTitle=4~150&usage_type=default&display_rank=4 Viguera, Adele, Medical Doctor “Postpartum depression: Risks of cognitive impairment and psychopathology in the children” UptoDate 14 October 2020 https://www.uptodate.com/contents/postpartum-depression-risks-of-cognitiveimpairment-and-psychopathology-in-the- Nava 12 children?search=paternal%20postpartum%20depression&source=search_result&selected Title=3~7&usage_type=default&display_rank=3 29 April 2021