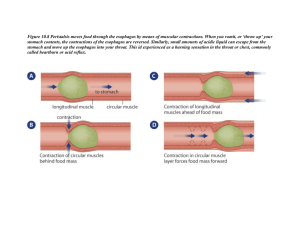
GI Pathology Digestion => Absorption => Excretion DIGESTION Reverse in the digestive system = vomiting o Vomiting: loss of fluid + electrolyte + acid = danger of creating alkalosis Too fast in the digestive system = diarrhea o Diarrhea: lose alkaline fluid = danger of creating acidosis (with chronic diarrhea) Too slow through the digestive system = constipation The stomach lining is made up of RUGAE, within the rugae, moving down the stomach, there are gastric pits. A number of cell types within the gastric pits have the responsibility of creating the gastric juices (really acidic) One of the cell types in the stomach is MUCOUS PRODUCING CELL – is a mechanical barrier so the acids produced by other cells are not going to corrode Acids are very potent protein digestive – breakdown protein bonds and take acids towards amino acids From voluntary swallowing to small intestine = digestion Can’t absorb proteins till it get to amino acids Can’t absorb carbohydrates till it gets to mono/disaccharides Lipids need to be broken down as close to fatty acids. Can absorb lipid molecules, but have to be small Anything not small get picked up by lymphatics, go through lymphatic system Any system where there is a transition increases chance for pathology o Sphincters regulate introduction to next segment o Weak sphincter b/w esophagus and stomach Pyloric sphincter – regulate dumping contents from the stomach to small intestine Ileocecal – last part of the small intestine, ileum, the pouch part of the beginning of the large intestine – tells us where to find it Smooth muscle creates peristalsis and then the valves will regulate how quickly or slowly they will be emptied ESOPHAGUS GERD – Gastro (stomach) Esophageal Reflex Disease (enteral – intestine) o Signs/Symptoms: Retrosternal pain (heartburn) Epigastric pain Burning sensation Gnawing Timing (key differential for heart issues) For gastroesophageal, going to be associated with eating and positioning. Wheezing Difficulty breathing o With repeated exposure, possibility of scaring. Repeated exposure with incomplete repair strictures may form. Strictures are going to narrow the esophageal or upper part of the stomach opening and put an imbalance in normal functioning of the passage of food from one segment to another, reduce efficiency of peristalsis and increase possibility esophageal weakness The anatomy of the esophagus not designed to resist the acids of the stomach; acids will burn, irritate causing inflammation, the esophageal epithelium o burning Different anatomy different function Inflammation of the esophagus called esophagitis o Chronic exposure to acid is going to create some type of cellular response. These cells are going to try to adapt to the chronic exposure of the acid, and try to convert to columnar. When you have that transition going on, called metaplasia. When metaplasia occurs, not by design, increase chance for mutations. Increase chance for mutation, increase chance for neoplasia (cancer) o Increase risk for Barrett’s cancer o Causes: a) *Incompetent L.E.S. (Lower Esophageal Sphincter) a) Weak b) Not preventing reflux c) Caffeine, alcohol, chronic exposure to acid will weaken esophageal sphincter b) *Hiatal Hernia (Hiatus – opening in the diaphragm, allows esophagus to enter the stomach) Sliding – L.E.S. is going up and down with eating & breathing. Rolling – Esophagus stays where it is supposed to, but part of the stomach can squeeze up, pulls everything. The valve has lost its patency, not as effective due to additional pressure In the esophagus the predominant epithelium is a stratified squamous epithelium, most of the esophagus is stratified squamous. In the stomach, it’s a columnar epithelium (simple columnar) o Longer than they are wide o More activity going on o They produce gastric juices c) Under Producing Saliva create esophagitis for a different reason, not from acid reflux, symptomology will be similar might lead to damage up to the L.E.S. which allows for some reflux to occur. Peristalsis – food it not being delivered effectively. o PSNS – Promoting peristalsis o SNS CAT Scan – relation b/w esophagus and diaphragm Protein stimulates gastric secretion Treatment o Not to lay down after eating o Smaller, more frequent meals o Chewing slower, completely o Antacids – careful b/c of people w/ heartburn Overindulging on antacids your not going to digest proteins effectively o Surgery (last resort) STOMACH PUD – Peptic (protein, pepsinogen, start in stomach) Ulcer (erosion of 1/more layers (4 layers in digestive system)) Disease. o 4 layers: 1. Mucosal layer (inner) 2. Submucosal (glands located) 3. Muscular layer (muscularis) (deeper) Halfway through to the esophagus, is smooth muscle. All the way through the tube at least 2 layers of smooth muscle. A circular layer that can squeeze the diameter shut or expand the diameter. The longitudinal layer that shortens the length of the tube. Squeeze and then shorten it, is how you get peristalsis. The stomach has the third layer. Stomach is a mixer. Not only will the stomach reduce its diameter and shorten but allow it to twist (3rd layer of muscle). Small intestine back to 2 layers of muscle. The large intestine will be a bit pouched, the longitudinal layer changes a bit, chronically short segments that create pouching. 4. Subserosa + Serosa G-cell => produce hormone called Gastrin. Will act on parietal cell. Parietal Cell = HCL(Pepsinogen) + intrinsic factor o Gastrin stimulates the parietal cells to produce HCL o Intrinsic factor is an important protein, that binds to vitamin B12 If the intrinsic factor can’t absorb B12, can’t make red blood cells, DNA, & can’t create myelin Chief cell => Pepsinogen o Pepsinogen + Acid (HCL) = Pepsin o Pepsin is an enzyme that is now active that breaks up peptide bonds (protein bonds) b/w amino acids. We are after pepsin for digestion. Mucosal Cell => Protect from acid o Produces mucous, mucous coats the lining of the stomach to protect from the acid Common cause for PUD is from a bacteria called: o Helicobacter pyloris (80%, most common cause) Flagellum gives this bacterium motility. It burrows away from the acid towards the mucous. When it gets out in the mucous starts to colonize and erodes some of the mucous. When it erodes the mucous, the acid can be exposed to the cells and they become inflamed and irritated. We exposed/interrupted the mucosal layer and the acids are all to start the digestion process on the cells in the stomach, ulceration. o NSAID’s (20%) (side effect concern) Break up the prostaglandin pathway (prostaglandin produced in the stomach promote mucous production & inhibit HCL acid production) When taking NSAID’s with the goal of reducing pain + inflammation, your blocking mucous production and promoting HCL acid production, creating an imbalance o Helicobacter pyloris (asymptomatic) + NSAID’s = Increased risk for PUD The concern when we start erosion, relatively minor if we erode the mucosal layer. The mucosal and epithelial layer don’t have a blood supply, so not bleeding. When you reach submucosal layer, and into muscularis there is bleeding. Bleeding will show up in the stool. If the bleeding is occurring in the stomach and shows up in the stool, its old blood. If the erosion is allowed to progress will go through the mucosal, submucosal, muscularis and if allowed through the outer layer, you have perforation. The contents of the stomach will be able to get into the peritoneum and spread, the bacteria will go crazy. This will cause systemic infection called sepsis (leads to shock). Shock is life threatening, drops BP means can’t deliver oxygen + nutrients to all the cells in the body, the cells become ischemic and organ shutdown Risk Treatment NSAIDS Weakened immune system Alcohol* Caffeine* Smoking* Remove NSAID’s Regulate alcohol, caffeine, smoking (limit/eliminate/modified) Manipulate acid-base balance o Antacids would reduce the presence/effectiveness of HCL acid Surgery – if concerned about perforation Dumping syndrome – resection of the stomach (take a section out of the stomach) o Reduce absorption of B12 vitamin o Taking out a section of parietal cells and intrinsic factor o Create a fluid shift in the interests of equalizing. o A large volume of chyme introduced to the small intestine. Goal of small intestine is absorption. If we dump a load in there, it becomes a hypertonic load, it will create a fluid shift (first concern) in the interest of equalizing fluid balances. Fluid shifting will occur in the intracell equilibrium. From the blood supply to small intestine. If pulling from blood supply create hypovolemia = hypovolemic shock. Blood glucose from a dump = hyperglycemia then hypoglycemia. Will be b/w hyper and hypoglycemia b/w meals, will put stress on beta cells and pancreas. This stress can cause Type 2 diabetes. GASTROENTERITIS Tells us its stomach or intestinal inflammation o Common cause: Infection 1. Food 2. Water o Treatment: fluid and electrolyte replacement o Higher up = vomiting, lower down = diarrhea S. Aureus o o o o o o o o o o E. Coli Enterotoxin Few hours Cooperative on skin, part of normal flora Issue – resistant to heat (less than 30 min of heating) Release exotoxin Fast to create an immune response Nausea (2-3hrs) -> vomiting (predominant) (last several days) -> diarrhea Fast, leads to upper GI Cause - Under cooked food, water Demand on oxygen o o o o o o o o o Salmonella Enterica o o o o o o Endotoxin Small intestine 2-3 days Eggs/poultry Sensitive to HCL Hard to figure source, b/c take 2-3 days to show (salmonella poisoning) Enterotoxin More hours (10-12hrs) Found in undercooked food/water Don’t have antibodies to fight when in different region (to drink water in diff’t region) Cause ulceration if aggressive Ex: Pork mixed with digestive contents of animal cause e.coli Depend on oxygen Diarrhea (Predominant), vomitting Targets intestine, Increase motility Clostridium Botulinum o o o o 1-2 days Anaerobic Colonized in canned food ( when dented, etc.) Very resistant to heat/cold when switch to sporform o Resistant to temp, releases very toxic chemical that targets ACH o Paralysis Treatment: replace electrolyte and fluids LARGE INTESTINE Diverticular Disease: o The walls of the large intestine become weak, and create out pouching along the pathway of the intestine b/c location for bacterial colonization, may create imbalance to normal flora creating an immune response, inflammation repair process may leave with scaring and further weakening. Bouts of constipation + diarrhea (class of presentation) Pouching visible in colonoscopy Diverticulosis – condition of extra pouching o Asymptomatic Diverticulitis – further down o Inflammation o Cramping o Burning Treatment: antibacterial, damaged area may need to be surgically removed Crohn’s Disease Ulcerative Colitis Present in proximal part of small intestine Reginal (scalp lesion) enteritis (localized) Skip lesions Very Aggressive Perforation Can affect all layers in the area its irritated at Low grade/acute, relatively constant Chronic (granulation, scarring) Surgery Distal in large intestine Cramping Exacerbation, remission Colon cancer No skip lesions Tends to be mucosal, submucosal, not all layers (out of muscularis) Increase risk by low fibre diet Treatment: frequent/smaller meals, high fiber Risk: smoking, alcohol, caffeine Increase risk for colon cancer COMMON Treatment: anti-inflammatory (corticosteroids), surgery Problem: chronic use of corticosteroids Idiopathic LIVER Ducts – drain products from the hepatocytes, liver cells, on daily basis Bile stored in gallbladder Bile drained from right & left hepatic duct into common hepatic duct and join with the pancreatic duct Pancreatic duct will drain the product from the bulk of the cells in the pancreas that produce enzymes for digestion Bile drained R/L hepatic ducts > common hepatic duct -> join pancreatic duct Gallbladder = cyst, small muscular pouch, an expansion for storing bile For healthy person, when food is introduced into the small intestine, pancreatic juices (from pancreatic cells) produce alkaline filled with enzymes (carboxypeptidase (peptidase act on peptides(protein), amylase(act on carbohydrates), lipase(act on lipids)). Alkaline neutralizes the acid from the stomach and enzymes activated once exposed to the mix of alkaline and acid in small intestine. Those enzymes are designed to finish the job of digestion Bile produced by hepatocytes –> collected by the duct system -> drained into small intestine to help with digestion Bile addresses small molecules of fat called micelles Bile eliminates cholesterol ADEK - Fat soluble Vitamin K -> Coagulation Vitamin K o Activated in large intestine o Allows osteoid to attract calcium to form mineralization Small intestine releases hormones: CCK, Cholecystic, Secretin o Cholecystokinin – encourages the pancreas to produce and release pancreatic juices (enzyme + alkaline) PANCREASE Exocrine Endocrine o Makes insulin(hypoglycemic) + glucagon(hyperglycemic) = homeostasis Auto digestion Pancreatitis – infection/ inflammation o Acute: short episode than treat for symptoms (respiratory and renal function are support after cause has been removed) o Chronic: Alcoholism (common), drugs(street drugs), abnormal duct formation, enzyme production, high levels blood calcium, trauma – slower progression/destruction o Invasive: damage to integrity of the pancreatic tissue than concerned about enzymes not staying at the duct but get outside the duct. If enzymes like peptidases get outside the duct, the will target other proteins in the body o Autodigestions – enzymes that are not where they belong, start autodigestive process in the pancreas o What started as an exocrine can change to endocrine b/c start to digest the cells that produce insulin(more concerned about insulin b/c only one that lowers blood glucose, no back up) and glucagon (has back up) Anything that can challenge the liver can challenge pancreas GALLBLADDER Stores bile Release bile when food in small intestine Problem: Formation of stones -> cholelithiasis (80% cholesterol, 20% +calcium++) Cholelithiasis (chole = cholesterol), Bile eliminates cholesterol Ultrasound can identify stones in gallbladder Cholecystitis o Acute/chronic o Hard to differentiate o May radiate upward o Inflamed gallbladder o Treatment: Chronic – removal of gallbladder Acute – wait a few days o Problem: when the stone is bigger than the diameter of the duct o Diagnosis: Ultrasound