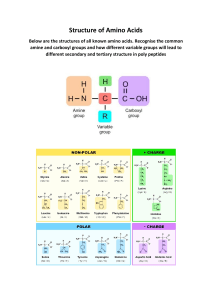
A SHORT NOTE ON HISTIDINEMIA & MAPLE SYRUP URINE DISEASE (MSUD) BY UBAH CHIOMA MIRACLE DEPARTMENT: BIOCHEMISTRY REGISTRATION NUMBER: 2019/249697 COURSE CODE: BCH 353 LECTURER: DR. E.J. NWEZE February, 2023 HISTIDINEMIA Histidinemia is a rare autosomal recessive metabolic disorder caused by a deficiency of the enzyme histidase. Histidase is needed for the metabolism of the amino acid histidine. Although originally thought to be linked to multiple developmental disorders, histidinemia is now accepted as a relatively benign disorder, leading to a reduction in the prevalence of neonatal screening procedures. Skeletal formula of histidine Histidinemia has an autosomal recessive pattern of inheritance. Histidinemia occurs as the result of an inborn error of metabolism that may result in either an inactive or a severely reduced histidine ammonia-lyase (HAL) enzyme activity. The gene that encodes for HAL spans a roughly 25 kb and consists of 21 exons located at the 12q22-q24.1 position of human chromosome 12. There are eight mutations currently associated with autosomal recessive histidinemia, that include: four missense mutations, two exonic polymorphisms and two intronic polymorphisms. DIAGNOSIS Histidenemia is characterized by increased levels of histidine, histamine and imidazole in blood, urine and cerebrospinal fluid. This also results in decreased levels of the metabolite urocanic acid in blood, urine, and skin cells. A typical characteristic of histidinemia is an increase in the blood histidine levels from normal levels (70–120 μM) to an elevated level (290–1420 μM). TREATMENT It has been suggested that a possible method of treatment for histidinemia is through the adoption of a diet that is low in histidine intake. However, the requirement for such dietary restrictions is typically unnecessary for 99% of all cases of histidinemia. MAPLE SYRUP URINE DISEASE (MSUD) Maple syrup urine disease (MSUD) is an autosomal recessive metabolic disorder affecting branched-chain amino acids. It is one type of organic acidemia. The condition gets its name from the distinctive sweet odor of affected infants' urine and earwax, particularly prior to diagnosis and during times of acute illness. The symptoms of MSUD depends on the severity of the disease. In older individuals, symptoms include erratic behavior, hypoglycemia, anemia, ketoacidosis, ataxia, etc. Death from cerebral edema will likely occur if there's no treatment. CAUSES Mutations in the following genes cause maple syrup urine disease: BCKDHA, BCKDHB, DBT and DLD. These four genes produce proteins that work together as the branched-chain alpha-keto acid dehydrogenase complex. The complex is essential for breaking down the amino acids leucine, isoleucine, and valine. These are present in some quantity in almost all kinds of food, but in particular, protein-rich foods such as dairy products, meat, fish, soy, gluten, eggs, nuts, whole grains, seeds, avocados, algae, edible seaweed, beans, and pulses. Mutation in any of these genes reduces or eliminates the function of the enzyme complex, preventing the normal breakdown of isoleucine, leucine, and valine. As a result, these amino acids and their byproducts build up in the body. Because high levels of these substances are toxic to the brain and other organs, this accumulation leads to the serious medical problems associated with maple syrup urine disease. DIAGNOSIS Prior to the easy availability of plasma amino acid measurement, diagnosis was commonly made based on suggestive symptoms and odor. Affected individuals are now often identified with characteristic elevations on plasma amino acids which do not have the characteristic odor. The compound responsible for the odor is sotolon (sometimes spelled sotolone). Newborn screening for maple syrup urine disease involves analyzing the blood of 1–2 day-old newborns through tandem mass spectrometry. The blood concentration of leucine and isoleucine is measured relative to other amino acids to determine if the newborn has a high level of branched-chain amino acids. Once the newborn is 2–3 days old the blood concentration of branched-chain amino acids like leucine is greater than 1000 μmol/L and alternative screening methods are used. Instead, the newborn's urine is analyzed for levels of branched-chain alphahydroxyacids and alpha-ketoacids. CLASSIFICATION Maple syrup urine disease can be classified by its pattern of signs and symptoms, or by its genetic cause. The most common and severe form of this disease is the classic type, which appears soon after birth, and as long as it remains untreated, gives rise to progressive and unremitting symptoms. Variant forms of the disorder may become apparent only later in infancy or childhood, with typically less severe symptoms that may only appear during times of fasting, stress or illness, but still involve mental and physical problems if left untreated. The sub-divisions of MSUD are Classic MSUD, Intermediate MSUD, Intermittent MSUD and Thiamine-Responsive MSUD. The amount and type of enzyme activity in an affected individual with MSUD will determine which classification the affected individual will identify with: 1. Classic MSUD: Less than 2% of normal enzyme activity 2. Intermediate MSUD: 3-8% normal enzyme activity 3. Intermittent MSUD: 8-15% of normal enzyme activity 4. Thiamine-Responsive MSUD: Large doses of thiamine will increase enzyme activity. TREATMENT Monitoring: Keeping MSUD under control requires careful monitoring of blood chemistry, both at home and in a hospital setting. DNPH or specialized dipsticks may be used to test the patient's urine for ketones when metabolic stress is suspected. Toxin Removal: Following diagnosis, rapid removal of excess leucine from the body reduces the impact of the disease on development. Exchange transfusion, hemodialysis, or hemofiltration may be used. Diet control: A diet with carefully controlled levels of the amino acids leucine, isoleucine, and valine must be maintained at all times in order to prevent neurological damage. Since these three amino acids occur in all natural protein, and most natural foods contain some protein, any food intake must be closely monitored, and day-to-day protein intake calculated on a cumulative basis, to ensure individual tolerance levels are not exceeded at any time. Other treatments include liver transplantation and control of metabolism during pregnancy.