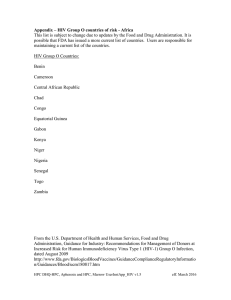
crossmark The Brief Case (For answers to the self-assessment questions and take-home points, see page 1176 in this issue [doi:10.1128/JCM.02648 -15].) A Reactive HIV Rapid Antibody Test in a Pregnant Woman Melanie L. Yarbrough, Neil W. Anderson CASE A 32-year-old pregnant woman presented to her obstetrician for routine prenatal care during her 3rd month of pregnancy. She reported no major health concerns, with the exception of mild morning sickness that had been gradually improving. Upon physical examination, she appeared healthy and her vitals were stable and within normal limits. Abdominal ultrasound revealed reassuring fetal heart tones, and her remaining physical exam was unremarkable. She was counseled regarding the need for several routine prenatal laboratory tests, including testing for human immunodeficiency virus (HIV), to which she agreed. A rapid HIV test performed in the obstetrician’s office was positive for antibodies against HIV. The positive rapid antibody result was shared with the patient. She denied any risk factors for HIV infection, including intravenous drug use and sex with multiple partners. The obstetrician stressed that the results were only preliminary and required confirmatory testing. Prior to sending the patient home, a blood sample was drawn for submission to the local clinical laboratory for additional testing. The obstetrician called the laboratory asking how long it would take for the Western blot confirmatory test to be performed. A representative from the testing laboratory informed him that they now used the fourth-generation algorithm and therefore no longer performed confirmatory testing by Western blot assay. Upon receipt of the patient sample, the laboratory performed a fourth-generation antigen/antibody test. This test was reactive, indicating the presence of HIV-specific antibodies or antigen. A second test capable of distinguishing HIV-1 and HIV-2 antibodies from one another (the HIV-1/2 differentiation assay) was performed and was nonreactive. Given these conflicting results, a separate specimen was sent for qualitative HIV-1 testing by nucleic acid amplification. HIV nucleic acid was not detected by this assay. Upon receipt of the test results, the obstetrician contacted the patient. He assured her that, based on her confirmatory test results, she was not infected with HIV. Though her antigen/antibody test was also positive, the negative HIV-1/2 differentiation assay and negative molecular test ruled out a diagnosis of HIV. Her initial rapid antibody and antigen/antibody screening tests were therefore false positives. DISCUSSION Approximately 1.2 million people in the United States are infected with HIV (1). HIV-1 and HIV-2 are acquired through contact with infected bodily fluids, such as blood, semen, vaginal fluids, or breast milk (2). The Centers for Disease Control and Prevention (CDC) recommend that all persons aged 13 to 64 years be 826 jcm.asm.org screened for HIV using an opt-out approach, meaning that individuals are notified that testing for HIV will be performed unless the person declines. The CDC also recommends that all pregnant women be screened for HIV in the first trimester of pregnancy and retested during the third trimester if the woman exhibits high-risk behaviors (3). Prenatal HIV screening has reduced the incidence of perinatal HIV infection, as women who test positive can be started on antiretroviral therapy and managed appropriately during delivery to reduce the risk of transmission (4). Diagnosis of HIV is accomplished by the detection of virologic and serologic markers. The appearance of these markers follows a predictable pattern (Fig. 1). Immediately after HIV infection, low levels of viral RNA may be present, although this is not consistently detectable by today’s methods. This period before HIV RNA and serologic markers are detectable is known as the eclipse period. Approximately 10 days after infection occurs, viral RNA rises to high enough levels that it can be detected by molecular assays. This is followed by increasing concentrations of the HIV p24 antigen, which are present in the blood of infected individuals around 15 to 20 days after infection. This is followed by host expression of immunoglobulin M (IgM) antibodies against the virus. Lastly, IgG antibodies appear and remain throughout HIV infection. The time between onset of infection and seroconversion is known as the window period. During this time, interpretation of results may be challenging since not all laboratory markers are positive. However, the sequential emergence of HIV markers is highly consistent, which has facilitated the development of sensitive and specific algorithms for diagnosis. In 2014, the CDC released the most updated version of the HIV diagnostic testing algorithm. The recommended algorithm starts with a fourth-generation, combined antigen/antibody immunoassay (IA). Fourth-generation IAs combine serologic testing for antibodies against HIV-1 and HIV-2 with antigenic testing for the presence of the p24 antigen expressed by both HIV-1 and HIV-2. Previously implemented third-generation assays did not include p24 antigen detection. Therefore, fourth-generation assays shorten the window period for detection of acute infection by 5 to 10 days compared to third-generation assays by recognizing HIV infection before seroconversion occurs (Fig. 1). Evaluations of patients with acute HIV have demonstrated that third-generation Citation Yarbrough ML, Anderson NW. 2016. A reactive HIV rapid antibody test in a pregnant woman. J Clin Microbiol 54:826 – 828. doi:10.1128/JCM.02647-15. Editor: A. J. McAdam Address correspondence to Neil W. Anderson, NAnderson@path.wustl.edu. Copyright © 2016, American Society for Microbiology. All Rights Reserved. Journal of Clinical Microbiology April 2016 Volume 54 Number 4 Downloaded from https://journals.asm.org/journal/jcm on 09 March 2023 by 165.225.125.35. Department of Pathology and Immunology, Washington University School of Medicine, St. Louis, Missouri, USA The Brief Case low levels of HIV RNA may be present but undetectable. This is known as the eclipse period. Approximately 10 days after infection onset, viral RNA rises to a level detectable by nucleic acid amplification testing (NAAT). Around day 15, the expression of HIV p24 antigen is detectable by fourth-generation antigen/antibody (Ag/Ab) combination assays, which detect both the p24 antigen and antibodies to HIV-1 and HIV-2. Third-generation antibody assays detect only HIV antibodies, which are measurable beginning approximately 20 days after infection. HIV-1 Western blotting, which identifies HIV-1 antibodies separated by electrophoresis, does not indicate a positive result until approximately 45 days after infection onset. assays were reactive in 20 to 37% of cases and that fourth-generation assays were reactive in 62 to 83% of cases (5). In patients with established HIV, fourth-generation assays have sensitivities ranging from 99.7 to 100%. The fourth-generation assays also exhibit high specificity for the diagnosis of HIV, ranging from 99.5 to 100% (5). Specimens with a reactive antigen/antibody IA require confirmatory testing with an IA that differentiates HIV-1 antibodies from HIV-2 antibodies (5). Differentiation is important because HIV-2 strains are not detected by commonly used molecular tests. Advantages of the differentiation IAs over HIV-1 Western blots include an earlier time to positivity, a faster turnaround time, ease TABLE 1 Interpretation of fourth-generation algorithm testing resultsa Test Result Interpretation HIV rapid antibody test Negative No further testing HIV rapid antibody test Positive Follow 4th-generation algorithm (see below) HIV-1/2 Ag/Ab combo Negative No further testing HIV-1/2 Ag/Ab combo HIV-1/2 Ab differentiation Positive HIV-1 Ab reactive Positive for HIV-1 infection HIV-1/2 Ag/Ab combo HIV-1/2 Ab differentiation Positive HIV-2 Ab reactive Positive for HIV-2 infection HIV-1/2 Ag/Ab combo HIV-1/2 Ab differentiation HIV-1 NAAT Positive Negative/indeterminate HIV-1 RNA detected Consistent with acute HIV-1 infection HIV-1/2 Ag/Ab combo HIV-1/2 Ab differentiation HIV-1 NAAT Positive Negative Not detected False positive or acute HIV-2 infection HIV-1/2 Ag/Ab combo HIV-1/2 Ab differentiation Positive HIV-1 and HIV-2 Ab reactive (undifferentiated) Positive for HIV antibodies but unable to differentiate between HIV-1 and HIV-2 a Ag, antigen; Ab, antibody. April 2016 Volume 54 Number 4 Journal of Clinical Microbiology jcm.asm.org 827 Downloaded from https://journals.asm.org/journal/jcm on 09 March 2023 by 165.225.125.35. FIG 1 Timeline of HIV laboratory results. Immediately after HIV infection, of interpretation, and lower cost. Differentiation IAs are thirdgeneration assays. Therefore, they do not detect HIV antigen and are not recommended as the initial screening test due to a lack of sensitivity (5). Confirmatory testing with the HIV-1/2 differentiation assay after a positive screen may be nonreactive despite true infection. This is especially true during acute infection, since these assays are not as sensitive as the screening method. If this is the case, the specimen should be tested with HIV-1 nucleic acid amplification testing (NAAT) to detect viral nucleic acid. Since HIV-1 nucleic acid is the first virologic marker to appear, it should be positive in a true acute infection with a positive antigen/antibody screen. A reactive HIV-1 NAAT result confirms acute HIV-1 infection, while a negative result denotes a false-positive result of the screening test (5). If a patient is positive by molecular testing alone, serologic conversion should be demonstrated for a definitive diagnosis of HIV infection. Of note, there is currently no FDAapproved NAAT for detection of HIV-2 viral nucleic acid. See Table 1 for common test results that occur with the updated algorithm and the corresponding interpretations. Rapid HIV screening tests are designed for use at the point of care. The vast majority are third-generation assays that detect antibodies to HIV-1 and HIV-2. Rapid tests offer the advantage of permitting a preliminary diagnosis in less than 30 min. According to traditional algorithmic testing, reactive rapid tests were confirmed by Western blotting. However, it is now recommended that reactive rapid tests be confirmed according to the fourthgeneration algorithm, starting with the initial antigen/antibody combination IA. This is due to the increased clinical sensitivity and specificity of antigen/antibody assays relative to those of rapid antibody assays (5). Thus, patients with positive rapid tests should undergo further testing by the fourth-generation algorithm in order to confirm a diagnosis of HIV (Table 1). A nonreactive antigen/antibody IA result after a positive rapid test result is indicative The Brief Case SELF-ASSESSMENT QUESTIONS 1. After a positive HIV rapid antibody test, which of the following tests should be ordered next? (a) HIV-1 Western blot assay. (b) HIV-1 nucleic acid amplification test. (c) HIV antigen/antibody immunoassay. (d) HIV-1/2 differentiation assay. 2. In a low-risk patient, which of the following results require 828 jcm.asm.org confirmatory testing with a qualitative molecular assay for HIV-1 as the next step? (a) HIV antigen/antibody immunoassay positive and HIV-1/2differentiation assay negative. (b) HIV antigen/antibody immunoassay positive and HIV-1/2 differentiation assay positive. (c) HIV rapid antibody test positive and HIV antigen/ antibody immunoassay negative. (d) HIV rapid antibody test positive and HIV antigen/ antibody immunoassay positive. 3. Which of the following is not an advantage of the HIV-1/2 differentiation assay for serologic confirmation as opposed to Western blot assay? (a) An earlier time to positivity following infection. (b) The ability to distinguish HIV-1 antibodies from HIV-2 antibodies. (c) The ability to rule out HIV infection based on a negative result. (d) A faster turnaround time. REFERENCES 1. Hall HI, An Q, Tang T, Song R, Chen M, Green T, Kang J, Centers for Disease Control and Prevention (CDC). 2015. Prevalence of diagnosed and undiagnosed HIV infection—United States, 2008 –2012. MMWR Morb Mortal Wkly Rep 64:657– 662. 2. Centers for Disease Control and Prevention. 2015. Diagnoses of HIV infection in the United States and dependent areas, 2013. HIV Surveil Rep 25. 3. Workowski KA, Bolan GA, Centers for Disease Control and Prevention. 2015. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 64(RR-03):1–137. 4. Fowler MG, Gable AR, Lampe MA, Etima M, Owor M. 2010. Perinatal HIV and its prevention: progress toward an HIV-free generation. Clin Perinatol 37:699 –719, vii. http://dx.doi.org/10.1016/j.clp.2010.09.002. 5. Centers for Disease Control and Prevention and Association of Public Health Laboratories. 2014. Laboratory testing for the diagnosis of HIV infection: updated recommendations. Centers for Disease Control and Prevention, Atlanta, GA. 6. Wesolowski LG, Delaney KP, Lampe MA, Nesheim SR. 2011. Falsepositive human immunodeficiency virus enzyme immunoassay results in pregnant women. PLoS One 6:e16538. http://dx.doi.org/10.1371/journal .pone.0016538. Journal of Clinical Microbiology April 2016 Volume 54 Number 4 Downloaded from https://journals.asm.org/journal/jcm on 09 March 2023 by 165.225.125.35. of a false positive, and no further testing along the algorithm is necessary (5). False-positive HIV screening tests can cause serious emotional distress and unnecessary follow-up. False positives have been documented in individuals with autoimmune disorders and in women who are pregnant, as in the case of this patient (5). An important contributor to the positive predictive value of HIV screening tests is the seroprevalence of the population being tested. A population of women without risk factors undergoing prenatal testing for HIV likely has a low seroprevalence and a resultant decrease in positive predictive value. A 2012 study among 921,438 pregnant patients with HIV screening by a thirdgeneration assay demonstrated that this positive predictive value can be as low as 30% (6). Thus, positive screening results should be handled delicately with these patients, and appropriate confirmatory testing should always be pursued. Testing under the fourth-generation algorithm has several advantages over previous methods. The increased sensitivity of fourth-generation screening tests allows for a higher likelihood of recognition of acute HIV infection. Additionally, the elimination of Western blotting as the confirmation test decreases turnaround time, decreases the chance of a false-negative result, and permits appropriate classification of HIV-2-infected individuals. Lastly, molecular testing for viral nucleic acid addresses potential false positives in the initial screening assay and confirms the presence of acute HIV infection. Thus, the updated algorithm facilitates a rapid and definitive diagnosis that can alleviate the confusion and anxiety triggered by false-positive screening results. crossmark Closing the Brief Case: A Reactive HIV Rapid Antibody Test in a Pregnant Woman (See page 826 in this issue [doi:10.1128/JCM.02647-15] for case presentation and discussion.) Melanie L. Yarbrough, Neil W. Anderson Department of Pathology and Immunology, Washington University School of Medicine, St. Louis, Missouri, USA 1. After a positive HIV rapid antibody test, which of the following tests should be ordered next? (a) HIV-1 Western blot assay. (b) HIV-1 nucleic acid amplification test. (c) HIV antigen/antibody immunoassay. (d) HIV-1/2 differentiation assay. Answer: c. According to the 2014 CDC recommendations for the diagnostic testing of HIV, patients with positive rapid antibody assay results should be tested by the fourthgeneration algorithm in its entirety. Therefore, the most appropriate next test is the HIV antigen/antibody immunoassay. 2. In a low-risk patient, which of the following results require confirmatory testing with a qualitative molecular assay for HIV-1 as the next step? (a) HIV antigen/antibody immunoassay positive and HIV-1/2 differentiation assay negative. (b) HIV antigen/antibody immunoassay positive and HIV-1/2 differentiation assay positive. (c) HIV rapid antibody test positive and HIV antigen/ antibody immunoassay negative. (d) HIV rapid antibody test positive and HIV antigen/ antibody immunoassay positive. Answer: a. The fourth-generation testing algorithm recommends confirmatory testing using a qualitative molecular technique for all patients with positive antigen/antibody immunoassay positive and negative HIV-1/2 differentiation assays. This is to detect possible cases of acute HIV-1. (a) An earlier time to positivity following infection. (b) The ability to distinguish HIV-1 antibodies from HIV-2 antibodies. (c) The ability to rule out HIV infection based on a negative result. (d) A faster turnaround time. Answer: c. HIV-1/2 differentiation has an earlier time to positivity, faster turnaround time, and lower cost than HIV-1 Western blotting. Negative results still require confirmation with a molecular test to rule out acute HIV. TAKE-HOME POINTS • Compared to third-generation antibody assays, fourth-generation antigen/antibody assays are more sensitive, more specific, and capable of earlier detection of HIV infection. • Testing for HIV by the fourth-generation algorithm entails screening with an antigen/antibody assay and confirmatory testing with an HIV-1/2 differentiation assay. • Patients with a reactive antigen/antibody assay but nonreactive HIV-1/2 differentiation assay should have molecular testing performed to distinguish acute HIV infection from a false-positive screen result. • Rapid HIV antibody tests offer a quick turnaround time, but reactive results should be confirmed using the fourth-generation algorithm. Citation Yarbrough ML, Anderson NW. 2016. Closing the Brief Case: A reactive HIV rapid antibody test in a pregnant woman. J Clin Microbiol 54:1176. doi:10.1128/JCM.02648-15. Editor: A. J. McAdam 3. Which of the following is not an advantage of using the HIV-1/2 differentiation assay for serologic confirmation as opposed to Western blot assay? 1176 jcm.asm.org Address correspondence to Neil W. Anderson, NAnderson@path.wustl.edu. Copyright © 2016, American Society for Microbiology. All Rights Reserved. Journal of Clinical Microbiology April 2016 Volume 54 Number 4 Downloaded from https://journals.asm.org/journal/jcm on 09 March 2023 by 165.225.125.35. ANSWERS TO SELF-ASSESSMENT QUESTIONS