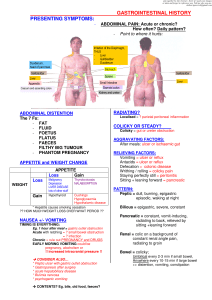
Gastrointestinal History The structure of the history will follow the usual structure you have been shown: Introduce yourself Gain consent to take the gastrointestinal history Presenting complaint History of presenting complaint Past history, medical and surgical Medications and allergies Social history Family history Ideas, Concerns and Expectations Before taking a gastrointestinal history you should be familiar with: The major gastrointestinal symptoms Major Gastrointestinal Symptoms 1. 2. 3. 4. 5. 6. 7. 8. 9. Abdominal pain Appetite/Weight change Nausea/Vomiting Heartburn/Acid regurgitation Dysphagia Disturbed defecation (diarrhoea, constipation, faecal incontinence) Abdominal distension Bleeding (haematemesis, melaena, haematochezia) Jaundice Introduction and Consent Introduce yourself, explain your role, obtain patient’s name, age/date of birth and where they are from. Ask their consent to proceed with history taking. Presenting Complaint (PC) The main symptom the patient presents with. It is likely to be one of the gastrointestinal symptoms listed above. ‘What problem brought you here today?’ ‘How can I help you?’ History of Presenting Complaint (HPC) This is the background to the presenting complaint/problem. Through a series of open, and then closed questions, you try to get as much information as you can about the PC. How/ when the problem started, how it has progressed over time, any pattern that is evident, factors which worsen or ease the problem, why the patient has now come to discuss it further, how it is impacting on their life/family etc? Are there any other associated gastrointestinal symptoms? Is there any history of gastrointestinal problems or previous diagnosis of gastrointestinal disease? 1. Abdominal pain you want to get more information about the pain to help you determine the likely cause. Site - ask the patient to point to the area affected by pain and the point of maximum intensity Epigastric – oesophagitis, gastritis, peptic ulcer disease, pancreatitis or gallstones Right Upper Quadrant – bilary colic, cholangitis or cholecystitis Central Abdominal – irritable bowel syndrome, inflammatory bowel disease or early appendicitis Suprapubic – diverticular disease, irritable bowel syndrome, inflammatory bowel disease or urinary tract infection Flank – renal colic Right Iliac Fossa – appendicitis, hernia, ovarian pathology ?(cyst or ectopic pregnancy) Left Iliac fossa – diverticulitis, ovarian Sites of Gastrointestinal pain Radiation –where the pain moves to, examples below; Pancreatitis pain can radiate from the epigastric region through to the back. Gall bladder pain can radiate around into the flank and the back. Renal pain can radiate down along the ureters and into the groin. Pain associated with subdiaphragmatic irritation (gall stones, perforated ulcer) may also be felt in the shoulder and tip of the scapula. Character – sharp/dull/burning. Colicky pain comes in waves e.g. from obstruction of a hollow viscous (i.e. bowel or ureters) Severity – score from 1 to 10, 1 being very mild, 10 being worst pain ever experienced. Onset – sudden/gradual Periodicity – constant/intermittent. How often does pain occur? Duration – minutes/hours/days. How long does/did it last? Aggravating factors– precipitants/makes it worse. Relieving factors - eases pain. Pain due to peptic ulcer may or may not be related to meals. Eating may precipitate ischemic pain in gut. Antacids or vomiting may relieve peptic ulcer pain or pain of gastro-oesophageal reflux pain. Patients who get relief from rolling around are more likely to have colicky type pain while those who lie very still are more likely to have peritonitis. 2. Appetite/Weight change can be a presenting symptom of gastrointestinal disease. As with pain you will need to explore the history of the appetite/weight change. The presence of both loss of appetite (anorexia) and weight loss should make one think of an underlying malignancy but may occur with depression and other diseases. It is important to determine how much weight loss has occured and over what time period. 3. Nausea/Vomiting nausea is the sensation of wanting to vomit. Heaving and retching may occur but there is no expulsion of gastric contents. Acute suggests gastrointestinal infection e.g. Food poisoning (staphylococcus aureus) or small bowel obstruction. Chronic - pregnancy and drugs (eg. digoxin, chemotherapy, opiates), peptic ulcer disease or alcoholism should to ruled out. Also remember to think of raised intracranial pressure and eating disorders. Timing is important, early morning vomiting prior to eating suggests raided ICP (intracranial pressure), pregnancy or alcoholism Contents old food suggests gastric outlet obstruction. Bile suggests open connection between duodenum and stomach, while blood suggests ulceration. Ask about contents – old food e.g. Gastric outlet obstruction. 4. Heartburn/Acid regurgitation Heartburn refers to the presence of a burning pain or discomfort in the retrosternal area. This symptom is due to regurgitation of stomach contents into the Oesophagus. Associated with gastro-oesophageal reflux may be acid regurgitation, in which the patient experiences a sour or bitter-tasting fluid coming up into the mouth. 5. Dysphagia is difficulty in swallowing. Such difficulty may occur with solids or liquids. Painful swallowing (odynophagia) which occurs with a severe inflammatory process involving the oesophagus (eg infective oesophagitis) should be distinguished from dysphagia. Causes of dysphagia include Oesophageal spasm, Oesophageal stricture, Oesophageal Carcinoma (progressive), mediastinal mass, Neurodegenerative disorder. 6. Disturbed defecation (altered bowel habit) Diarrhoea can be defined in a number of different ways. Patients may complain of frequent stools (more than 3 per day) or they may complain of change in the consistency of the stools which have become loose or watery. There are a large number of causes of diarrhoea and finding out if it acute (infective cause) or chronic can help determine the possible cause. Constipation is a common symptom and can refer to the passage of infrequent stools (less than 3 per week), hard stools or stools that are difficult to evacuate. It can be an acute or chronic problem. It is important to determine what the patient means by constipation. Causes include, metabolic disorders eg hypokalaemia (low potassium) or endocrine disorders eg hyothyroidism or partial colonic obstruction from carcinoma. Other causes include pregnancy, multiple sclerosis and low-fibre diet. 7. Abdominal distension a feeling of swelling may result from excess gas or hypersensitive intestinal tract (irritable bowel syndrome). Persistent swelling can be due to ascitic fluid accumulation (liver disease). Don't forget pregnancy. 8. Bleeding Haematemesis: vomiting blood, bleeding from upper GIT Melaena: passage of dark black tarry stools, bleeding from upper GIT/ right side colon/small bowel lesions Haematochezia: Bright red blood per rectum, usually indicates bleeding from lower GIT Causes of upper GIT bleeding: Peptic ulcer disease Oesophageal varices Oesophageal/Gastric neoplasm Arteriovenous malformations Mallory-Weiss tears (superficial oesophageal tears after repeated vomiting) Causes of lower GIT bleeding: Cancers/polyps Colitis/ulcers (including Inflammatory bowel disease and infectious) Anorectal disease (hemorrhoids, fissures, and rectal ulcers) Diverticular disease 9. Jaundice Jaundice: yellow discoloration of the sclera or skin, due to the presence of excess bilirubin. Have you noticed your skin or your eyes looking a little yellow? Has anyone else commented on it? Has your urine been any darker (obstructive jaundice)? How about your stools – are they paler than usual (obstructive jaundice)? Causes of jaundice Intra-hepatic (Liver disease) Viral Alcohol Drug Pregnancy Cirrhosis – any type Extra-hepatic Common duct stones Carcinoma – head of pancreas/ampulla/bile duct Pancreatitis/pseudocyst Biliary stricture Past History : past medical history(PMH), past surgical history (PSH) Open ended questions initially ‘How is your health generally?’ Does the patient have any known medical problems/illnesses? Are they attending a doctor regularly- when/ why were they last there? Have they had any medical investigations? Have they had any operations at all? Have they had colonoscopy or oesophago-gastro-duodenoscopy(OGD)? Any previous gastrointestinal problems? Screen for conditions using closed questions (short checklist) Have they ever been diagnosed as having any of the following: Peptic ulcer disease Irritable bowel syndrome Jaundice Hepatitis GIT malignancy Inflammatory Bowel Disease High blood pressure/High cholesterol Heart disease/Cerebrovascular disease (angina, heart attacks or strokes) Diabetes Medication Are they currently taking any medication/tablets? Any prescribed medicines, over the counter medicines from a pharmacy or health shop or herbal remedies? Any ‘recreational drug’ use? If the patient is taking meds you want to know what they are for, who prescribed them and is the patient complying/ taking them as they were advised? Examples of GIT medications that may be in use Anti-diarrhoeal agents Laxatives Anti-emetics Analgesics, especially paracetamol (can cause liver damage) and Non Steroidal Anti-Inflammatory Drugs (cause peptic ulcer disease/GIT bleeds) Allergies Do they have any known allergies to anything at all – drugs/medications/ latex? Ask them to explain what they mean by allergy. What exactly happened to them? Nausea/vomiting/rash/swelling/breathing difficulty? This will help you determine if it was a true allergy. Social History (SH) Home situation- Who do they live with? (Spouse/ partner/ children/ parents). Any dependants? What support do they have at home? Can they manage stairs, if present , in their house? Bathroom up/ downstairs? Occupation? Stress, physical activity, can they manage the work? Hobbies/sports/sedentary lifestyle? Risk of hepatitis transmission – healthcare worker (vaccinated)/travel/sexual behaviour/intra-venous drug usage? Smoking History- do they smoke, have they ever smoked, has it changed recently? How much do they smoke and how long have they smoked for? Alcohol History- Do they drink alcohol, if so how much? Has this changed? Calculate how many units they drink weekly. 11 units is the recommended maximum for women and 17 units is the max recommended for men. Glass of beer- 1 unit Pint beer- 2 units Family History (FH) Enquire about parents and siblings. Are they alive? If so are they well or do they have any medical problems? In this case do they have any history of gastrointestinal problems in particular, eg bowel cancer, inflammatory bowel disease or liver disease (haemochromatosis)? If they are deceased you need to ask at what age they died and what was the cause of their death? Remember to be sensitive and empathise as appropriate. Ideas, Concerns, Expectations and Impact on patient’s daily life. Try to give the patient an opportunity to tell you if there is anything that they want explained or if there is something they are particularly worried about. For example- they may be terrified that they have colonic cancer as their brother died from colonic cancer. They may be concerned that if they are unable to work for some time their business will not survive or their bills will be unpaid. It is important to explore this with the patient at the end of the consultation. E.g. do you have any questions? Is there anything that you are particularly worried about?