structural and functional changes in the heart during pregnancy in women with cardiovascular diseases
advertisement

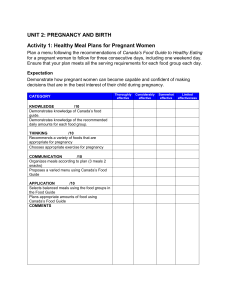
Structural and functional changes in the heart during pregnancy in women with cardiovascular diseases 2021-08-13 14:03 In a healthy woman with a normal pregnancy, structural and functional changes in the heart are adaptive in nature, slightly expressed and completely normalized after childbirth. #07/21 Keywords: Angiology , Pregnancy , Gynecology , Cardiology , Peripartal cardiomyopathy , Heart defects , Cardiovascular risk , Echocardiography , Pregnancy , Gynecology , Cardiology , Peripartal cardiomyopathy , Heart diseases , Cardiovascular risk , Echocardiography NO ADS Summary. In a healthy woman with a normal pregnancy, structural and functional changes in the heart are adaptive in nature, slightly expressed and completely normalized after childbirth. In a pregnant woman with certain heart diseases, adaptive capabilities are reduced, therefore, at any stage of pregnancy, pathological changes can occur that complicate its course and lead to adverse outcomes. In addition, any pregnancy can develop new heart conditions that can be fatal. That is why an echocardiographic assessment of structural and functional changes in the heart is necessary both during normal pregnancy and against the background of concomitant cardiovascular diseases. The importance of echocardiography (EchoCG) in the examination of pregnant women for the detection of structural and functional changes in the heart today is beyond doubt, and its place is determined by a number of modern clinical recommendations. Thus, in 2018, the revised recommendations of the European Society of Cardiology (ESC) for the management of patients with cardiovascular diseases (CVD) during pregnancy were published [1], which confirmed and clarified the main provisions for the use of echocardiography in this group of women. . A little earlier, the Russian national guidelines “Diagnostics and treatment of cardiovascular diseases during pregnancy” [2] were approved, summarizing domestic and most significant foreign clinical recommendations for 2011-2017. In addition, systemic reviews and meta-analyses have been published in recent years, devoted to intracardiac hemodynamics, cardiac remodeling, cardiovascular pathology in pregnant women, to some extent considering issues related to the analysis and interpretation of data obtained from echocardiography. In this regard, the purpose of this article is to consider the key points that doctors of the so-called “multidisciplinary team” (cardiologist, obstetrician-gynecologist, anesthesiologistresuscitator and other involved specialists) need to know to assess the state of the heart during planning, during and after pregnancy. Determination of cardiovascular risk when planning pregnancy To date, according to health statistics and based on clinical practice, it has been established that, in general, cardiovascular pathology is detected in at least 10% of pregnant women and steadily occupies the second place, after anemia, among extragenital pathologies [2, 3]. These are arterial hypertension (AH), congenital and acquired heart defects (CHD and PPS, respectively), cardiac arrhythmias, cardiomyopathy and some other diseases. The nature of the disease and the functional state of the heart determine the course of pregnancy, the risk of complications, and sometimes contraindications for pregnancy. In this regard, when planning pregnancy, it is advisable to assess the cardiovascular maternal risk. Determination of risk in women of childbearing age with CVD should be carried out according to the modified classification of the World Health Organization (WHO) (Table 1) [1]. Along with this, the risk should be clarified by the presence of predictors of complications, the significance of which has been proven in the CARPREG, ZAHARA and ROPAC studies. These predictors of the risk of complications in a mother with cardiovascular pathology are summarized in Table 1. 2. ADVERTISING ADVERTISING As can be seen from the tables, both the WHO classification and the list of predictors of complications are largely based on the structural and morphological signs of heart and aorta damage, ventricular dysfunction, and pressure in the pulmonary artery detected and calculated by echocardiography. So, for example, in diseases of the aorta (this group includes the bicuspid aortic valve, Marfan, Ehlers-Danlos syndromes and others), in the absence of its dilatation, the maternal risk is considered low, but it is assessed as very high with dilatation over 45-50 mm, depending on pathology. Based on the combination of signs indicating the possibility of aortic dissection, pregnancy is contraindicated. Quantitative echocardiographic parameters, such as left ventricular ejection fraction (LVEF), valve orifice area are of the same importance. The risk is assessed not only before the first, but also with each subsequent pregnancy. The need for reassessment is understandable, since the state of the heart can change both during the onset of pregnancy and after it due to various circumstances. Structural and functional changes in the heart during a normal pregnancy The first EchoCG examination of a pregnant woman is usually carried out at 12 weeks and repeated in subsequent trimesters as necessary if indicated [2]. During pregnancy in a healthy woman, the volume of fluid increases by 40-100%, and the volume of circulating blood - by 30-50%, which inevitably leads to an increase in preload [4]. The first changes can be determined with echocardiography already at the 5th week of gestation, when an increase in stroke volume and cardiac output by an average of 20% is determined. By the 20th week of gestation, the shifts increase, and the increase in these indicators can be 30–50% higher compared to the initial ones. By the end of the first trimester, an increase in the size of the left atrium is clearly recorded, by the end of the second trimester, an increase in the size and volume of the left ventricle is possible, which gradually increase until childbirth [5]. In the third trimester, the LV sphericity index increases. When comparing indicators, LV volumes increase to the greatest extent - by 30-50%, to a lesser extent, its size by an average of 11% [5]. However, they do not go beyond the generally accepted norm. At the same time, “physiological hypertrophy of pregnant women” (pregnancy-induced hypertrophy) is described, in which the thickness of the walls of the left ventricle and the mass of the myocardium increase. The maximum mass of the myocardium is determined in the III trimester of pregnancy. The total increase in myocardial mass is sometimes up to 70-80% relative to the original [6, 7]. It is important that there are no violations of the function of the heart. ADVERTISING In the first trimester, Doppler sonography can detect an increase in early diastolic filling velocity (Ve) and a decrease in atrial systole blood flow velocity (Va) of the transmitral diastolic flow. At the end of the II and III trimesters, the contribution of left atrial contraction to left ventricular filling increases, which is reflected in an increase in the Va velocity and, accordingly, a relative decrease in the E/A ratio. The isovolumetric contraction time (IVRT) and flow deceleration time (DT) are lengthened, but the acceleration time (AT) remains stable [7]. In the first trimester, the rate of systolic blood flow slightly increases and, at the same time, the rate of diastolic blood flow in the pulmonary veins decreases. It is important that these changes occur in pregnant women with normal blood pressure or slightly elevated diastolic blood pressure due to the expression of fetal genes, physiological hormonal changes. A decrease in systolic longitudinal strain of the basal, middle and apical segments of the left ventricle and systolic strain of the right ventricle, which are detected during a more in-depth study using the strain, strain-rate modes, is described. At the same time, no significant changes in the radial and circular deformation of the ventricles are recorded [8]. It should be noted that this decrease is insignificant, short-term, not accompanied by any clinical symptoms and spontaneously resolves without treatment. At the same time, no significant changes in the radial and circular deformation of the ventricles are recorded [8]. It should be noted that this decrease is insignificant, short-term, not accompanied by any clinical symptoms and spontaneously resolves without treatment. At the same time, no significant changes in the radial and circular deformation of the ventricles are recorded [8]. It should be noted that this decrease is insignificant, short-term, not accompanied by any clinical symptoms and spontaneously resolves without treatment. ADVERTISING Systolic pressure in the pulmonary artery sometimes increases to 40 mm Hg. Art. Slightly, by 2-3 mm, the size of the aortic root increases. The appearance of mitral and tricuspid regurgitation of 1-2 degrees is possible [1]. All these changes are reversible. Full normalization is noted by 3-6 months after delivery. Observations are described in which recovery was recorded only after 1 year. ADVERTISING Cardiac hemodynamics in multiple pregnancy Cardiac hemodynamics in singleton and multiple pregnancies has a number of differences. This is due to higher levels of peripheral vascular resistance to arterial blood flow in the fetal-placental circulation, which can be considered as an adaptive reaction in conditions of its increased functional stress in multiple pregnancies. If in the first trimester of pregnancy, the indicators of uteroplacental hemodynamics in multiple and singleton pregnancies do not differ significantly, then in the future there is an intensive decrease in vascular resistance of blood flow in the uterine arteries, which leads to a change in hemodynamic parameters, which are more pronounced in multiple pregnancies. So, In multiple pregnancy, the volume of circulating blood rapidly increases in the II-III trimesters of pregnancy and by the 34th week increases by 50-70% of the initial values. Such changes lead to a significant increase in the work of the heart, while the stroke volume of the heart increases by more than 30%, the heart rate increases by 15-20%, and the total peripheral resistance decreases by about 25%. Pregnant women with arterial hypertension The following clinical variants of hypertension during pregnancy are distinguished: ADVERTISING • Hypertension before pregnancy; • chronic hypertension; • hypertension or symptomatic hypertension; • gestational hypertension; • chronic hypertension complicated by preeclampsia; • preeclampsia/eclampsia. Determination or clarification of heart damage as a target organ in hypertension, i.e. detection of LV hypertrophy in conjunction with the assessment of systolic and diastolic myocardial function, are the primary tasks of echocardiography in the management of patients with hypertension and are necessary to obtain additional information about prognosis and risk. When hypertrophy is detected, it is necessary to carry out a differential diagnosis with physiological myocardial hypertrophy (pregnancy-induced hypertrophy), which is detected from the second trimester, and this hypertrophy is usually concentric. In addition, data from a number of studies demonstrate that during pregnancy complicated by hypertension, left ventricular myocardial mass and relative wall thickness increase more than during normotensive pregnancy [9]. Peripartum cardiomyopathy A disease that occurs exclusively during pregnancy or in the postpartum period (between the last months of pregnancy and up to 5 months after childbirth). Data on its frequency are contradictory: from 1 case per 3000-4000 pregnancies to 1 case per 15,000 births [10], which may indicate the difficulties of diagnosis. This pathology is suspected in all cases when a pregnant woman has signs of heart failure, heart rhythm disturbances, and also if the condition after childbirth slowly returns to normal. The risk of peripartum cardiomyopathy is increased in women over 30 years of age with multiple pregnancies, preeclampsia, in patients with bronchial asthma, and anemia. Echocardiography is of priority in the detection of peripartum cardiomyopathy. The diagnosis is established on the basis of a set of clinical and echocardiographic criteria [10, 11]: 1. Heart failure: • last month of pregnancy; • 5 months postpartum. 2. No previous heart disease. 3. The absence of a specific cause of the disease, other than pregnancy. 4. Obvious echocardiographic signs of LV dysfunction: • ejection fraction less than 45% and/or fractional shortening less than 30%; • end-diastolic LV diameter greater than 2 2.7 cm/m . With a reduced ejection fraction (<35%), thrombi form in the LV cavity, which is the cause of thromboembolism. Recovery and return to normal is achieved in most, but not all women, and in some cases, heart function has a positive trend, but only up to certain values o f the ejection fraction. With incomplete recovery (“recovery with a defect”), peripartum cardiomyopathy may reappear in subsequent pregnancies [10]. Thus, the diagnosis of peripartum cardiomyopathy is made by exclusion in the absence of evidence of all other possible causes of systolic insufficiency. That is why, in each case, a very careful EchoCG assessment of the structure and function of the heart is necessary, a comparison of the obtained data with the previous ones (the best is with the EchoCG protocol before pregnancy) in order to differentiate the existing picture with changes occurring in severe preeclampsia, other forms of cardiomyopathies, congenital and acquired pathology of the heart, as well as with pulmonary embolism, myocardial infarction, intracardiac formations, sepsis. Pregnant women with heart defects In the structure of all CVD in pregnant women, according to various sources, 30-50% are CHD, about 15% - PPS [12, 13]. Establishing a diagnosis, assessing the anatomy of the valve, hemodynamics, the severity of the defect, including in terms of indications for cardiac surgical correction during pregnancy (for example, balloon commissurotomy), monitoring pregnant women in the postoperative period - these are the tasks that face echocardiography [2]. ]. ADVERTISING In recent decades, the number of pregnant women with congenital heart disease has increased significantly due to the widespread introduction of cardiosurgical methods of correction. Girls operated on in early childhood reach childbearing age. Their clinical condition, quality of life are often quite satisfactory in order to plan a pregnancy. Initially, pregnant women with previously confirmed congenital heart diseases should be examined by echocardiography up to 10-12 weeks of gestation to determine the prognosis of the possibility of carrying a pregnancy [2]. Based on the results of the examination, together with a cardiologist, an obstetrician- gynecologist and, if necessary, a cardiac surgeon, a conclusion is made on the presence or absence of contraindications to pregnancy, the need for cardiac surgical treatment. Further, in the normal course of pregnancy, no risk or low risk, echocardiography is performed at 18-22 and 27-32 weeks, as well as before childbirth. A large frequency of echocardiography is determined by the clinical condition, the type of heart disease. Often, it is the EchoCG conclusion that is decisive in matters of further tactics of pregnancy management and early delivery for medical reasons. Caesarean section is reasonable in patients with acute refractory heart failure, severe aortic stenosis, severe pulmonary hypertension (including Eisenmenger's syndrome), or acute heart failure. ADVERTISING mitral stenosis In the structure of PPS in pregnant women, mitral stenosis occupies the first place (about 60%) and is the most dangerous, with serious, sometimes fatal complications associated with it [14]. Often this defect is first diagnosed during pregnancy. This is due to the fact that he remains asymptomatic for a long time. When the area of t he mitral orifice is more than 1.5 cm2, the course of pregnancy is close to normal. However, moderate and severe stenosis (valvular orifice area less than 1.5 cm2) is associated with clinical manifestations (primarily shortness of breath) and a high risk of complications such as pulmonary edema, cardiac arrhythmias, and progressive heart failure. Echocardiography - assessment of valve morphology in pregnant women with mitral stenosis is of particular importance. The need for balloon mitral commissurotomy depends on the changes in the valve, whether there is calcification of the leaflets. Currently, this operation is performed successfully at any stage of pregnancy, while the overall maternal mortality does not exceed 1% (slightly higher, up to 2%, with calcification of the valves), fetal death is about 2%, and the level of postoperative complications is low. At the same time, with open commissurotomy and valve replacement, fetal death occurs in 10-30% of cases. In addition, when installing valve prostheses, anticoagulants will be required in the future [15]. ADVERTISING The frequency of echocardiography depends on the severity of mitral stenosis, the state of hemodynamics. With mild mitral stenosis, a stable condition of the pregnant woman, examinations are performed in each trimester and before childbirth. In moderate and severe at least once every two months or monthly [2, 14]. Mitral insufficiency Mitral valve insufficiency in pregnant women is usually of rheumatic origin, as well as due to mitral valve prolapse, including due to myxomatous degeneration. There is also functional regurgitation in congenital heart defects, including those operated on in childhood. Unlike mitral stenosis, complications in pregnant women with this defect are infrequent, which is explained by good adaptation to volume load as a result of a decrease in total peripheral vascular resistance during pregnancy and, accordingly, a decrease in the volume of regurgitation. Echocardiography determines the severity of regurgitation, the size of the cavities of the heart. When planning pregnancy, patients with moderate to severe regurgitation are advised to perform an exercise test. During pregnancy, in almost all cases, there is an increase in the degree of regurgitation, the size of the left cavities of the heart. The risk of complications depends on the severity of regurgitation and LV function. Note that mitral regurgitation prevents the formation of blood clots in the left heart. With mild and moderate regurgitation, echocardiography is repeated every month, with severe - at least once every 2 months [2, 14]. Aortic valve stenosis When planning pregnancy, it is recommended to determine the degree of aortic stenosis, as well as to clarify the adaptive reserve of the cardiovascular system by conducting a test with physical activity. Thus, mild aortic stenosis is characterized by good adaptation to volume load, the absence of symptoms, and a favorable course of pregnancy. On the contrary, in severe aortic stenosis, the adaptation of the heart to the load is much worse, but despite this, a favorable course of pregnancy is also possible. With echocardiography in patients planning pregnancy with aortic stenosis, attention is paid to LV function. In case of impaired systolic function, according to the recommendations, valvuloplasty or aortic valve replacement is reasonable in all patients with severe aortic stenosis with clinical symptoms, as well as with asymptomatic disease, but impaired LV function or decreased exercise tolerance. Otherwise, pregnancy is not recommended. ADVERTISING Echocardiography in cases of aortic stenosis shows an increase in the size of the left ventricle and atrium, as well as an increase in the average and maximum pressure gradient from trimester to trimester [16]. The area of t he aortic orifice, ejection fraction, as a rule, do not change. Echocardiography is performed monthly in severe aortic stenosis, in other cases once a trimester [2, 14]. ADVERTISING Aortic insufficiency In severe aortic regurgitation with LV dysfunction and acute aortic regurgitation, pregnancy is poorly tolerated. Therefore, such patients need to be examined before pregnancy. Focus on determining the severity of regurgitation, measuring the size and function of the left ventricle, the size of the aorta. If severe regurgitation is detected in combination with dysfunction or dilatation of the left ventricle, the defect needs to be corrected before pregnancy [16] due to the high risk of developing heart failure. Echocardiography in patients with mild and moderate regurgitation is performed every 3 months, but in severe regurgitation, the frequency is set individually, based on the woman's condition and the course of pregnancy [2, 14]. Tricuspid insufficiency Tricuspid regurgitation in pregnant women in the vast majority of cases is functional due to pressure and / or volume overload of the right ventricle. However, with severe dilatation of the valve ring (≥ 40 mm), moderate and severe tricuspid regurgitation, the patient should be consulted with cardiac surgeons to decide on surgical intervention. When planning a pregnancy in patients with severe regurgitation, surgery before pregnancy is recommended. ADVERTISING Dilatation of the ascending aorta Dilatation of the ascending aorta is detected in approximately 50% of pregnant women with a bicuspid aortic valve. In these cases, the size of the aorta is especially closely monitored during each EchoCG examination [17]. If a woman planning pregnancy has a diameter of the 2 ascending aorta ≥ 50 mm (27.5 mm/m ), then, regardless of the presence of symptoms, it is necessary to discuss the possibility of surgery before pregnancy, since the degree of dilatation may increase and there is a risk of its dissection. The risk of aortic dissection is higher in Marfan-Ehlers-Danlos syndrome. Women with aortic root dilatation over 40 mm, dilatation of the ascending aorta are recommended to undergo echocardiography every 4-8 weeks and 6 months after delivery [17]. Increase in size during pregnancy is considered a risk factor for aortic dissection. For patients with an aortic diameter of more than 45 mm, with Marfan's syndrome, in which the aortic diameter is 40-45 mm, acute or chronic dissecting aortic aneurysm, operative delivery is advisable. Conclusion Thus, echocardiography is necessary to assess the structural and functional state of the heart during pregnancy, especially in women with a history of cardiovascular pathology. The frequency of examination and the algorithm are individual and depend on the severity of comorbidity [18]. The correct interpretation of the obtained EchoCG changes allows the doctor to conclude that the changes in the woman's body have a normal or pathological effect on the heart. An echocardiogram is mandatory to assess maternal risk, determine indications / contraindications for pregnancy, as well as the method of delivery. ADVERTISING CONFLICT OF INTEREST. The authors of the article confirmed the absence of a conflict of interest, which must be reported. CONFLICT OF INTERESTS. not declared. Literature/References 1. 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy // European Heart Journal. 2018; 39 (34): 3165-3241. DOI: 10.1093/eurheartj/ehy340ESC. 2. Diagnostics and treatment of cardiovascular diseases during pregnancy 2018. National recommendations. Developed by the Committee of Experts of the Russian Society of Cardiology (RCS). Section of diseases of the cardiovascular system in pregnant women // Russian Journal of Cardiology. 2018; 3 (155) 91-134. [Diagnostika i lechenie serdechno-sosudistykh zabolevanii pri beremennosti 2018. Natsional'nye rekomendatsii. Razrabotany Komitetom ekspertov Rossiiskogo kardiologicheskogo obshchestva (RKO). Sektsiia zabolevaniia serdechno-sudistoi sistemy u beremennykh [Diagnosis and treatment of cardiovascular diseases during pregnancy 2018. National guidelines. Developed by the Committee of experts of the Russian society of cardiology (RSC). Section of cardiovascular diseases in pregnant women] // Rossiiskii kardiologicheskii zhurnal. 2018; 3 (155): 91-134. 3. Tsiaras S., Poppas A. Cardiac disease in pregnancy: value of echocardiography // Curr Cardiol Rep. 2010; 12(3): 250-256. DOI: 10.1007/s11886-010-0106-9. 4. Narayanan M., Elkayam U., Naqvi TZ Echocardiography in Pregnancy: Part 2 // Curr Cardiol Rep. 2016; 18 (9): 90. DOI: 10.1111/echo.13242. 5. Savu O., Jurcu? R., Giu?c? S., van Mieghem T. et al. Morphological and functional adaptation of the maternal heart during pregnancy // Circ Cardiovasc Imaging. 2012; 5(3):289-297. DOI: 10.1161/CIRCIMAGING.111.970012. 6. Li J., Umar S., Amjedi M., Iorga A., Sharma S., Nadadur RD, Regitz-Zagrosek V., Eghbali M. New frontiers in heart hypertrophy during pregnancy // Am J Cardiovasc Dis. 2012; 2(3): 192-207. 7. Schannwell C. M., Zimmermann T., Schneppenheim M., Plehn G., Marx R., Strauer B. E. Left Ventricular Hypertrophy and Diastolic Dysfunction in Healthy Pregnant Women // Cardiology. 2002; 97: 73-78. DOI: 10.1159/000057675. 8. Cong J., Fan T., Yang X., Squires J. W., et al. Structural and functional changes in maternal left ventricle during pregnancy: a three-dimensional speckle-tracking echocardiography study // Cardiovasc Ultrasound. 2015; 13: 6. DOI:10.1186/1476-7120-13-6. 9. De Haas S., Ghossein-Doha C., Geerts L., van Kuijk S. M. J., van Drongelen J., Spaanderman M. E. A. Cardiac remodeling in normotensive pregnancy and in pregnancy complicated by hypertension: systematic review and meta-analysis // Ultrasound Obstet Gynecol. 2017; 50 (6): 683-696. DOI: 10.1002/uog.17410. 10. Arany Z. Understanding Peripartum Cardiomyopathy // Annu Rev Med. 2018; 69: 165-176. DOI: 10.1146/annurev-med041316-090545. 11. Bauersachs J., Arrigo M., Hilfiker-Kleiner D., Veltmann C., et al. Current management of patients with severe acute peripartum cardiomyopathy: practical guidance from the Heart Failure Association of the European Society of Cardiology Study Group on peripartum cardiomyopathy // Eur J Heart Fail. 2016; 18 (9): 1096-105. DOI: 10.1002/ejhf.586. 12. Nanna M., Stergiopoulos K. Pregnancy Complicated by Valvular Heart Disease: An Update // Journal of the American Heart Association. June 2014, Wolters Kluwer Health. DOI: 10.1161/jaha.113.000712. 13. Pessel C., Bonanno C. Valve disease in pregnancy // Semin Perinatol. 2014; 38 (5): 273-284. S0146-0005(14)000342.10.1053/j.semperi.2014.04.016. 14. Le?niak-Sobelga A., Tracz W., Kostkiewicz M., Podolec P., Pasowicz M. Clinical and echocardiographic assessment of pregnant women with valvular heart diseases- maternal and fetal outcome // Int J Cardiol. 2004; 94 (1): 1523. OpenUrl CrossRef PubMed. 15. Roeder H. A., Kuller J. A., Barker P. C., James A. H. Maternal valvular heart disease in pregnancy // Obstet Gynecol Surv. 2011; 66 (9): 561-571. DOI:10.1097/OGX.0b013e318238605d. 16. Windram J. D., Colman J. M., Wald R. M., Udell J. A., Siu S. C., Silversides C. K. Valvular heart disease in pregnancy // Best Pract Res Clin Obstet Gynaecol. 2014; 28 (4): 507-518. DOI: 10.1016/j.bpobgyn.2014.03.009. 17. Shim W. J. Role of echocardiography in the management of cardiac disease in women // J Cardiovasc Ultrasound. 2014; 22 (4): 173-179. DOI: 10.4250/jcu.2014.22.4.173. 18. Горохова С. Г., Морозова Т. Е., Аракелянц А. А., Барабанова Е. А., Дьяконова Е. Г. Алгоритм эхокардиографического исследования у беременных // Российский кардиологический журнал. 2018; 23 (12): 75-82. [Gorokhova S. G., Morozova T. E., Arakeliants A. A., Barabanova E. A., D'iakonova E. G. Algoritm ekhokardiograficheskogo issledovaniia u beremennykh/Algorithm of echocardiography in pregnant women // Russian Journal of Cardiology. 2018; (12): 75-83. (In Russian.)] А. А. Аракелянц 1 , кандидат медицинских наук Т. Е. Морозова, доктор медицинских наук, профессор Е. А. Барабанова, кандидат медицинских наук Е. О. Самохина, кандидат медицинских наук РЕКЛАМА ФГАОУ ВО Первый МГМУ им. И. М. Сеченова Минздрава России, Москва, Россия 1 Контактная информация: nxrrimma@mail.ru Структурно-функциональные изменения сердца при беременности у женщин с сердечно-сосудистыми заболеваниями/ А. А. Аракелянц, Т. Е. Морозова, Е. А. Барабанова, Е. О. Самохина Для цитирования: Аракелянц А. А., Морозова Т. Е., Барабанова Е. А., Самохина Е. О. Структурно-функциональные изменения сердца при беременности у женщин с сердечно-сосудистыми заболеваниями // Лечащий Врач. 2021; 7 (24): 18-23. DOI: 10.51793/OS.2021.24.7.004 Теги: женщины, беременные, сердечнососудистые заболевания Купить номер с этой статьей в pdf Наше сообщество Вконтакте Наш канал в Telegram Еженедельный дайджест "Лечащего врача": главные новости медицины в одной рассылке Подписывайтесь на нашу email рассылку и оставайтесь в курсе самых важных медицинских событий Cпасибо, ваши данные приняты. Не забудьте подтвердить подписку, в письме, которое вы получите на почту. поле обязательно для заполнения поле обязательно для заполнения поле обязательно для заполнения Специализация Акушер-гинеколог Аллерголог Гастроэнтеролог Гематолог Гепатолог Дермато-венеролог Кардиолог Невролог Нейрохирург Инфекционист Онколог Отоларинголог Офтальмолог Педиатр Психиатр Пульмонолог Проктолог Ревматолог Рентгенолог и радиолог Терапевт и врач общей практики Уролог Фтизиатр Хирург Эндокринолог Другое поле обязательно для заполнения Подписаться на новости Нажимая на кнопку Подписаться, вы даете согласие на обработку персональных данных Перейти на оригинал