NSG 352; Wk 2 Chain of Infection & Vital Signs
advertisement
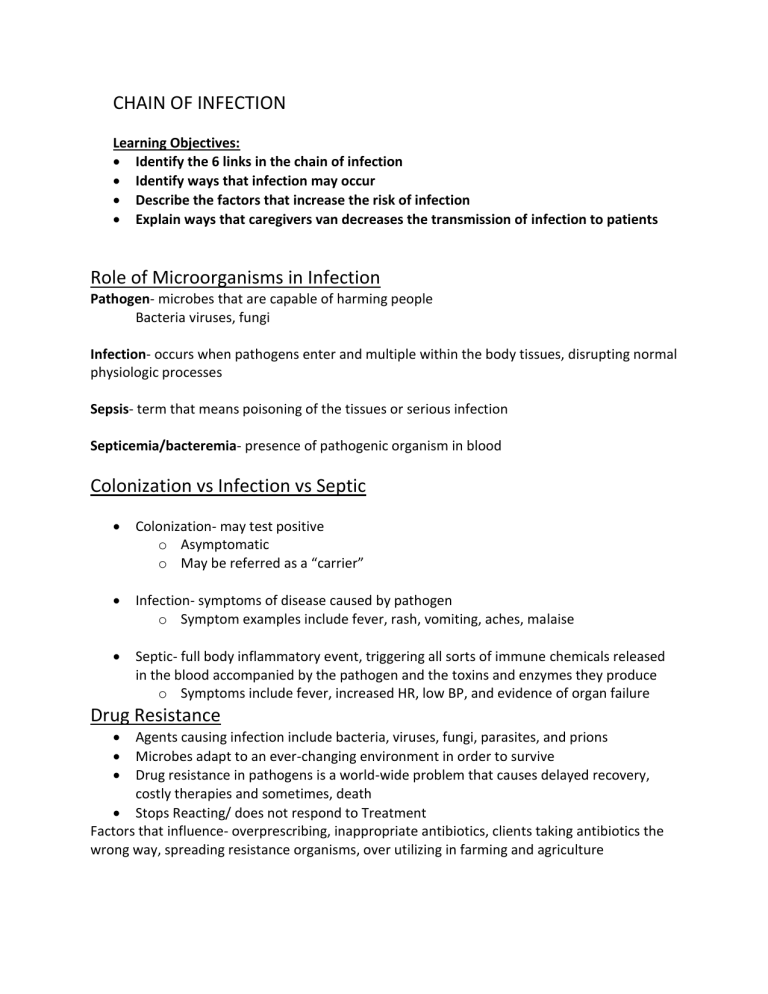
CHAIN OF INFECTION Learning Objectives: Identify the 6 links in the chain of infection Identify ways that infection may occur Describe the factors that increase the risk of infection Explain ways that caregivers van decreases the transmission of infection to patients Role of Microorganisms in Infection Pathogen- microbes that are capable of harming people Bacteria viruses, fungi Infection- occurs when pathogens enter and multiple within the body tissues, disrupting normal physiologic processes Sepsis- term that means poisoning of the tissues or serious infection Septicemia/bacteremia- presence of pathogenic organism in blood Colonization vs Infection vs Septic Colonization- may test positive o Asymptomatic o May be referred as a “carrier” Infection- symptoms of disease caused by pathogen o Symptom examples include fever, rash, vomiting, aches, malaise Septic- full body inflammatory event, triggering all sorts of immune chemicals released in the blood accompanied by the pathogen and the toxins and enzymes they produce o Symptoms include fever, increased HR, low BP, and evidence of organ failure Drug Resistance Agents causing infection include bacteria, viruses, fungi, parasites, and prions Microbes adapt to an ever-changing environment in order to survive Drug resistance in pathogens is a world-wide problem that causes delayed recovery, costly therapies and sometimes, death Stops Reacting/ does not respond to Treatment Factors that influence- overprescribing, inappropriate antibiotics, clients taking antibiotics the wrong way, spreading resistance organisms, over utilizing in farming and agriculture Links in the Chain of Infection Infectious agent: bacteria, fungi, virus, parasite, prions Source: human, animal, inanimate object Portal of Exit: sputum, emesis, stool, blood Made of transmission: contact, vehicle, droplet, airborne, vector Portal of entry: mucous membrane, non-intact skin, GI tract, GU tract, Respiratory tract Susceptible Host: immunosuppressed, elderly, chronically ill, trauma, surgery BREAK THE CHAIN CDC and Hospital Monitoring for HAI CAUTI (Catheter-Associated Urinary Tract Infections) CLABSI (Center Line-Associated Bloodstream Infections) SSI (Surgical Site Infections) C Diff (clostridium difficile) o Dehydrates and malnourished quickly HAP (Hospital acquired pneumonia) MRSA (Methicillin-Resistant Staphylococcus Aureus bacteremia) One in 31 hospital clients has at least one healthcare-associated infection Standard Precautions Measures to protect you, other employees, patients, and their families ALL THE TIME Hand Hygiene before and after client care/contact, before and after gloving Wear gloves for blood/body fluid Wear masks, eye protections and gowns during potential of splashing Following respiratory hygiene/cough etiquette Cleaning and disinfecting the environment appropriately Handling linens and laundry carefully Following safe injection practices and proper handling of needles and other sharps Protect Everyone: Monitoring of personnel/employee o TB screen annually o Monitoring for high risk Decreasing the risk of needle sticks or unintentional exposure Preventing transmittable diseases Proper use of isolation procedures for patients requiring isolation Airborne Precautions - small particle droplets that can remain suspended and widely dispersed by air movement and flow -Wear a mask when transported out of room -Negative pressure room with door closed; air isn’t circulating in others -N95 masks worn by everyone in room -EX: TB, measles, chickenpox Droplet Precautions -microbes transmitted by larger particle droplets which disperse into air currents by client coughs, sneezing, or talking -Private room or cohered with a person with same microbe -Regular mask and eye protection -Client where mask outside room -EX: pneumonia, influenza, whooping cough, bacterial meningitis Contact Precautions - organisms that can be transmitted by hand-skin or skin0skin contact during client activities or when touching the clients’ environmental surfaces or care items -Limit transport of client whenever possible, if necessary, cover or contain colonized areas of body -Use disposable of educated care equipment. Disinfect before use on another client -Private room or cohered with client with same organism -Gloves when the room and change when exposed to potentially infected material -Gowns and other protective barriers -EX: MRSA, VRE, open wounds, RSV Contact Precautions (Enteric) -C Diff- No use of alcohol hand hygiene products -Area COVID-19 Precautions -N95 masks -Gown, gloves, eye protection, -Gloves -Single room with door closed -For aerosol-generating procedures, place in airborne isolation -Limit transport out of room Protective isolation - used in high-risk situations to prevent infection for people whose body defenses are known to be compromised -No fresh fruits and veggies -No flowers in water or soil -Private room with visitor restrictions -EX: oncology patients with neutropenia (low white blood cell count) as a result Personal Protective Equipment ON: gown, mask, goggles, gloves OFF: gloves, goggles, gown, mask, good hand hygiene Medical Asepsis - measures aimed at reducing number and spread of microbes for all clients >Hand hygiene >Disinfecting equipment >Use of PPE >Handling of soiled equipment and linen >Proper management of trash >Private rooms or cohering clients Surgical Asepsis -asepsis or sterile technique- to prevent the introduction of microbes from the environment to client >Surgical procedures >Procedures that invade the bloodstream >Sterile gloves >Selected dressing changes and wound care Cleaning Disinfection Sterilization C- refers to remove of foreign material from object An object that becomes soiled by bloody or body fluids and stays in the same patient’s room D- refers to the chemical or physical process used to reduce the number of pathogens on an object’s surface A piece of equipment being moved from one patient room to another (walker) S- refers to the complete destruction of all microbes including spore A piece of equipment that is being used for an aseptic of sterile procedure VITAL SIGNS Learning Objectives: Describe the procedures used to assess vital signs Describe factors that influence each vital sign Identify rationale for variations in techniques used Recognize normal vital sign values among age groups Temperature Measurement of body’s core temp using a thermometer Normal: 96.6F-100.6F or 35.8-38.1C Too high> 100.6F or 38.8C, hyperthermia Too low< 96.6F or 35.8C Routes Axillary o Armpit o inaccurate used on newborns as screening tool Tympanico Ear o impacted by user variability and ear wax for adults pull pinna of ear up and out infants and children less than 3, pull pinna down and back Oralo tongue o affected by hot and cold liquids and oxygenation delivered via facemask. Not ideal for children or those unable to keep mouth open Temporalo scan forehead Less invasive Good for all age groups Rectalo Rectum o invasive and risk of insertion too far Avoid with rectal bleeding Factors That Affect Temperature: Time of day o low in morning o high at night Age o young and old have issues holding onto heat Hormones o progesterone (secreted during ovulation in women) increases body temperature Environment/Ambient Temperature o client exposure to extreme hot/cold Exercise o physical activity increases body temperature Stress o emotional or physical stress can increase body temp How to Choose: Consider policy of organization/unit What equipment is available How reliable does it need to ne Age/condition of patient Consider how invasive the route is Pulse Measurement of the patient’s circulation as the aorta expands and then contracts creating a pulsation or throb in the artery measured per minute Normal varies by age typically from 60-100 for adults Too high> 100 for adults “Tachycardia” Too low< 60 for adults “Bradycardia” Routes o apical (for all ages) o Radial (primarily for older children/ adults) Other pulse sites used to determine peripheral circulation and not for measurement of pulse Factors: -pulse quality by palpation -Pulse rate -Pulse rhythm Factors that affect pulse: Ageo newborns have rapid pulses of 140-160bpm which slows as they grow and mature o By school age. Pulse slows to 60-110 bpm o Older adults have slower pulse to the weakening of the heart with age and disease Medications o beta blockers slow the pulse o beta adrenergic increase pulse Autonomic nervous system o - stimulation of the vagus nerve slows the pulse (bearing down to have a bowel movement, simulation of the carotid artery) o Sympathetic nervous system stimulation raises the pulse (pain, anxiety, fever, caffeine ingestion) Choose the “right” route for pulse movement: Auscultating an apical pulse using stethoscope o Place the stethoscope at the 5th intercostal space, midclavicular Used for infants less than 1 yr For those with fast, irregular heart rhythms For those with slow rhythms, especially receiving beta blockers Count for 60 sec Palpating a radical pulse o Use one or two fingers of your hand parallel to the course of the artery on the wrist just below thumb o Press lightly so as to not occlude the artery o Count for 15 seconds and multiple by 4 for regular rhythms o Count for 60 seconds for irregular rhythms or abnormally slow or fast rhythms Respirations measurement of the process of the respiratory cycle Count inspiration and expiration as one respiration over one minute Normal varies based on age from 12-20 breaths per minute for adults Too high> 20 breaths/min for adults’ “tachypnea” Too low< 12 breaths/min for adults “bradypnea” Absent for more than 10 secs is “apnea” Methods: observation: watching rise and fall of chest Palpation: placing hand on the chest to feel the rise and fall Auscultation: listening to inhale and exhale with a stethoscope Factors that Impact: client activity Depth of respirations Factors affect respirations Age o newborns and infants’ breath faster Slowing as lung capacity increases older adults can have increased respirations as the lung tissue becomes less elastic Gender o men have a slower respiration due to increased lung capacity as compared to women Altitude o increases reparations due to the lower percentage of oxygen in air Medicationo sympathomimetic drugs or inhaled corticosteroids can increase the patient’s ability to move air and slow respirations Opioids decrease respirations Exercise o increases respiration as the body’s need for oxygen increases Stress o pain, anxiety, infections, and fever can increase respirations Blood Pressure The measurement of the force that blood exerts against the walls of the blood vessels and measured in mm Hg Systolic (Top Number) measures ventricular contraction (cardiac systole) Diastolic (Bottom Number) measures ventricular relaxation (cardiac diastole) Normal varies based upon age o but considered SBP less than 120 and DBP less than 80 Too high> 140/90 Too low < 100/60 for adults is “hypotension” Methods manual BP sphygmomanometer automated BP Factors that impact Cuff size o Width of bladder should be at least 40% of the circumference of midpoint of limb Too small or loose can lead to falsely high readings Too large can lead to falsely low readings Proper positioning o Measure BP at the heart level o When sitting or standing, the arm should be horizontally at the level of heart Elevating arm above heart level can result in falsely low reading while below the heart can result in a falsely high reading Proper inflation and deflation o Slow, prolonged, or frequent cuff inflation promotes venous congestion o At least 1-2 minutes should elapse between sequential cuff inflation on the same limb Auscultation o As you deflate the cuff and blood returns, Korotkoff sounds can be heard with the stethoscope o Phase 1 is the systolic blood pressure, while Phase 5 is the diastolic Factors that Affect Age o Increases gradually from birth throughout childhood into adulthood with growth and age o Older adults have increase due to narrowing of arteries, decrease in vessel elasticity and increased systemic vascular resistance Circulating Volume o Fluid volume deficit from hemorrhage or dehydration with decrease BP o Excess fluid from renal failure or congestive heart failure will increase BP Normal Fluctuations o Ambient temperature with vasoconstriction and vasodilation can increase and decrease BP o Circadian rhythm with BP being highest in the morning Autonomic Nervous System o Increased sympathetic response result in BP increase (pain, anxiety, fear, smoking, exercise) Medications o Diuretics create fluid loss and decreases BP o Cardiac drugs that decrease heart rate decrease BP o Antihypertensive drugs will decrease BP o Opioid analgesics can decrease BP How to Choose the “Right” Method Check for limb alerts to determine a “do not use” limb or side o Presence of venous access device o s/p mastectomy with lymph node removal o recent procedure to a limb upper extremity vs lower extremity o limb size vs cuff size o lower extremity often used for infants/toddlers o loss of limb or non-intact skin due to surgery/injury/burns o ensure that the cuff and stethoscope are appropriate for the artery being used Manual versus automated o Location/setting, availability of equipment o Patient movement, ability for patient to stay still o Very irregular heart rate o Frequency of BP readings Orthostatic Hypotension Drop in SBP of at least 20mm HG or drop in DBP of at least 10 mmHg AND increase in HR of at least 10bpm WITH movement from lying to siting or standing o Start with client flat for 10 minutes, wait 2 minutes between position changes to take BP and HR Results from inadequate reflex compensation upon position change o Can be problem for clients with hypovolemia (low systemic volume) autonomic nervous system dysfunction Parkinson’s disease Diabetes Education for clients o Change positions slowly o Increased fall precautions Causes symptoms associated with decreased cerebral prefusion Dizziness weakness blurred vision syncope marked change in BP and heart rate with position changes from lying to siting Pulse Oximetry The measurement of the percentage of hemoglobin that combines with oxygen in the blood o Reported as SpO2 (arterial oxygen saturation) Noninvasive and indirect means for approximating oxygenation Sensor is attached to the patient’s finger and infrared light passes through from one side of the finger to the other o Can also use earlobe, forehead, toe using special probes Normal varies based on age but typically SpO2 93-95% are normal o Too low <93% usually is an indication for further assessment and possibly supplemental O2 Methods used for measurement Pulse Oximeter Factors that Impact: Nail polish Core body temperature Peripheral perfusion Factors Affect carbon monoxide poisoning false high readings Edema at the sensor site false low reading Anemia o Cause high readings bc most of the hemoglobin has oxygen attached to it, however, there are fewer hemoglobin molecules. Anemia can cause hypoxemia because there isn’t enough hemoglobin molecules in the blood Pain Personal and subjective “what the client says it is” Can be acute or chronic or both Affects many of the other vital signs and is important to assess at the time of taking vital signs OLDCART O-nset L- ocation D-uration C-haracteristics A-ggravating factors R-elieving factors T-reatment Factors Affect: Age o Older people had more sensitivity to pain and willingness to report History with pain Gender o Women were more sensitive to pain and more willing to report pain but more able to endure pain Culture o Disparity in pain management for non-native population Language o Ability to understand terms o Challenges with using English and Pain reading tools