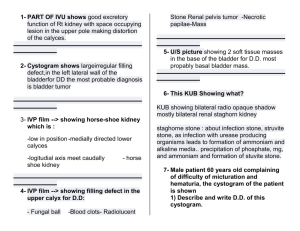
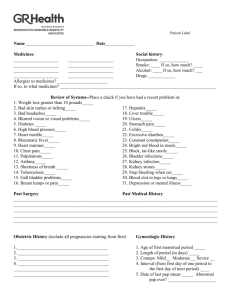
Bladder cancer more common in men. White men Exposure to dyes and industrial chemicals Long term foley. Previous radiation Bladder has transitional cells and most are papilliomatous Bladder cancer most common symptoms painless hematuria Stage 1 is in the lining. Stage 2 is muscle. Stage 3 is adjacent tissue Stage 4 is lymph nodes Cystoscopy is how bladder cancer is diagnosed with a biopsy Treatments 1. Surgery 2. Radiation 3. Immunotherapy. 4. TURBT -transuretheral resecetion of bladder tumor. 5. Partial cystectomy- partial bladder removal. 1056 and 1054 learn about urine diversion devices Ilieal conduit- bypasses the bladder through the ileum and into the ureters. Is a stoma Indiana pouch -is where you catheterize. Neobladder? Complications of bladder surgery 1. bleeding 2. pain opiods 3. constipation Surgery Radiation and chemo(nivolumab and Pimbrolizumab And intravesicular chemo BCG bacilli Calmette-guerin. Empty their bladder reposition q15 Increase fluids to manage dysuria Stop smoking, no public bathrooms for 6 hours, sit when peeeing Add 2 cups of bleach to urine let sit for 15 minutes Pd1 blockers are cancer immunosuppressive. KIDNEY CANCER More likely in men Greater than 64 years old Hypertension Obesity Smoking 1st degree relative which is a risk factor only in kidney. EXPOSURE TO GASOLINE ASBESTOS AND CADMIUM PRESENTATION FLANK PAIN HEMATURIA ABDOMINAL PAIN. DIAGNOSED BY CT SCAN, RENAL ULTRASOUND. PARTIAL NEPHRECTOMY CAN BE DONE LAPRASCOPICALLY OR OPEN INCISION Simple nephrectomy (kidney) Total radical nephrectomy (kidney ureters) If there is severe increase in pain there is concern for retroperitneal bleed.) Can also use ablation with a laser or cryotherapy Also treated with bevacizumab (avastin) Angiogenesis inhibitor. Staging kidney tumors Stage 1 kidney Stage 2 kidney >7 cm Stage 3 invades tissue adjacent Stage 4 Lymph nodes End Stage Renal Disease Less than GFR 15 Less than 400 ml per day= oliguria Less than 100 is anuria. Uremia becomes azotemia Azotemia is build up of waste Signs and symptoms Confusion, lethargy, weakness, headache n/v, muscle cramps and spasm. Pruritis and uremic frost anorexia. Hyperglycemia Hyperkalemia Hypermagnesemia Dysrhythmias Edema Hypertension Active vitamin D is in the gut leads to low calcium leads to increased parathyroid hormone and increased phosphorus. Higher risk for fractures. Anemia leads to hypoxia Can cause tetany Decreased platelets. Hyperkalemia can be treated by kayexalate Patiromer- cant be taken with food 6 hours before or after Sodium polystyrene sulfate For high phosphorus give phosphate binding Inhibitor SEVELAMAR CARBONATE - RENAGEL Sensipar – CALCIUMMIETIC. A normal peritoneal dialysis exchange 2 Liters over 15-20 min. Dwell 4-6 hours. Drain up to 30 minutes. Dextrose helps draw fluid off. Strict aseptic technique. Automated 4 exchanges usually at night leave fluid in all day Continuous is 4-5 exchanges instill dc dwell reconnect drain. Peritonitis can be caused from not using a septic technique. Staph is usual cause. These patients usually have pain nausea vomiting gas abd distention and hyperactive bowel sounds. Effluence is what you drain. Ask patient if they are having their period because that could be a cause of blood in the effluent. 10- 20 grams of protein loss is normal. Anything less is worrisome. Hemodialysis red is for removing. Blue returns the blood, Arteriovenous graft higher infection rates than fistulas often have clots or graft rejection. Steal syndrome- the fistula shunts blood away from the distal part of extremity such as fingers and hands and STEALS the blood from this area. Continuous renal replacement therapy prolonged dialysis to not mess with blood pressure. Procrit helps with erythropoietin. Hyperacute rejection is within 24 hours they must remove the kidney,. Acute is after 24 hours to 6months they can give steroids and other medications Chronic rejection they can remove it and go on dialysis.