Diabetes Mellitus: Definition, Types, Symptoms & Treatment
advertisement

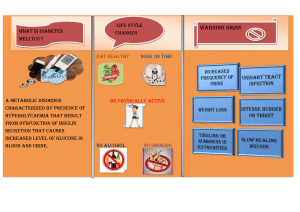
Definition Etiology & pathogenesis Methods of diagnostics Clinical pattern Diabetes mellitus is a disorder in which blood levels of glucose are abnormally high. There are 3 types of diabetes mellitus: type 1 (insulin-dependent diabetes), type 2 (non-insulin-dependent diabetes), gestational diabetes. Type 1 (insulin-dependent diabetes). Etiology isn’t known for sure. Scientists believe that a viral infection in childhood can cause the immune system to destroy the insulin -producing beta cells of the islets of Langerhans in the pancreas. As a result it leads to insulin deficiency. This type of diabetes may be caused by a genetic predisposition. Most people with this type of diabetes had developed the disease by age of 30. Type 2 (non-insulin-dependent diabetes). Type 2 diabetes is due primarily to lifestyle factors and genetics. This type of diabetes usually begins after age of 30. A number of lifestyle factors are known to be important to the development of type 2 diabetes, including obesity, lack of physical activity, poor diet and stress. Dietary factors also influence the risk of developing type 2 diabetes. Consumption of sugar-sweetened drinks in excess is associated with an increased risk. The key cells that are affected when Type 2 diabetes initially develops include the glycated red blood cells, and the muscle, fat, and liver cells, which are designed to take glucose (sugar) out of the blood, pull it into the ce lls and change it into energy. These cells require insulin to absorb glucose. When these cells fail to respond adequately to circulating insulin, these cell s lose their sensitivity to insulin (a condition known as insulin resistance) and blood glucose levels rise. The body responds to this situation by signaling the pancreas to produce more insulin, causing insulin levels in the blood to become too high. This condition is known as hyperinsulinemia. The cells in the liver also become insulin resistant and respond by making too much blood sugar. Because blood sugar is not absorbed by the cells, it stays in the blood, causing blood sugar levels to rise — a condition known as hyperglycemia. Gestational diabetes. Diabetes that's triggered by pregnancy is called gestational diabetes. It is often diagnosed in middle or late pregnancy. Because high blood sugar levels in a mother are circulated through the placenta to the baby, gestational diabetes must be controlled to protect the baby's growth and development. Gestational diabetes is generally resolved after baby is delivered. Taking anamnesis, blood sugar test, oral glucose tolerance test, test for glycated hemoglobin ( HbA1c), urine test Polyuria (excessive amount of urine which is excreted due to high level of glucose) , polydipsia (abnormal thirst), polyphagia (excessive hunger), glycosuria (presence of glucose in the urine), blurred vision, drowsiness, nausea, and decreased endurance during exercise. In type 1, diabetes symptoms can develop suddenly in previously healthy children or adolescents. In type 2, diabetes symptoms usually show up gradually. Treatment Complications There is no cure for diabetes. The main goal of diabetes treatment is to keep blood sugar levels within the normal range . Treatment for type 1 diabetes includes: Insulin replacement therapy. Insulin is available in 3 forms: rapid-acting – begins to lower blood glucose level within 20 minutes and reaches its maximum activity in 2 to 4 hours; intermediate -acting starts to work in 2 or 3 hours and lasts up to 36 hours; long-acting exerts very little effect for about 6 hours but provides coverage for 28 to 36 hours. Low carbohydrate diet Frequent blood sugar monitoring Eating healthy foods Exercising regularly and maintaining a healthy weight. Type 2 diabetes can be controlled with weight management, nutrition, and exercise. Low-carbohydrate diet This type of diabetes tends to progress and oral hypoglycemic drugs are often needed to lower blood glucose. There are several classes of hypoglycemic drugs: Sulphonylureas are the class of drugs that exerts its hypoglycemic effect by stimulating insulin secretion from the pancreatic beta cells. Biguanides (example metformin) are the class of drugs that inhibits the process of gluconeogenesis in liver; decreases intestinal absorption of glucose; reduces target cells resistance to insulin by increasing glucose uptake and utilization. Unlike sulphonylureas, biguanides do not cause hypoglycemia. Besides, metformin prevents vascular complications of DM. Alpha-glucosidase inhibitors are the class of drugs that inhibit alpha-glucosidase enzymes in the intestine, thus decreasing glucose reabsorption in the intestine. Some patients with type 2 diabetes may need to use insulin injections if their diabetes cannot be contro lled with diet, exercise and oral medication. A patient may develop diabetic coma if a level of glucose in his blood is extremely high or low. The damage to small blood vessels leads to a microangiopathy, which can cause one or more of the following: Diabetic cardiomyopathy, damage to the heart muscle. Diabetic nephropathy, damage to the kidney which can lead to chronic renal failure. Diabetic neuropathy, abnormal and decreased sensation starting with the feet but potentially in other nerves, later often fingers and hands. When combined with damaged blood vessels this can lead to diabetic foot (see below). Diabetic retinopathy, growth of friable and poor-quality new blood vessels in the retina which can lead to severe vision loss or blindness. Diabetic encephalopathy is the increased cognitive decline and risk of dementia- including the Alzheimer's typeobserved in diabetes. Macrovascular disease leads to cardiovascular disease, to which accelerated atherosclerosis is a contributor: Coronary artery disease, leading to angina or myocardial infarction Peripheral vascular disease, which contributes to intermittent claudication as well as diabetic foot. Prevention Definition Aetiology& pathogenesis • • • • Clinical pattern Diabetic foot, often due to a combination of sensory neuropathy (numbness or insensitivity) and vascular damage, increases rates of skin ulcers (diabetic foot ulcers) and infection and, in serious cases, necrosis and gangrene . Stroke (mainly the ischemic type) There is no known preventive measure for type 1 diabetes. Type 2 diabetes can often be prevented by a person being a normal body weight, physical exercise, and following a healthful diet. Diabetic coma is a life-threatening diabetes complication that causes unconsciousness. Dangerously high level of glucose in blood is known as hyperglycemia. Hypoglycemia is dangerously low level of glucose in blood. Both conditions can lead to death. There are three main causes of diabetic coma. Two causes are most often associated with type 1 diabetes, and one is most often associated with type 2 diabetes. Type 1 diabetes A diabetic coma can happen when one of the following is present: very low blood glucose levels, also known as hypoglycemia high blood ketone levels, also known as diabetic ketoacidosis Type 2 diabetes A diabetic coma can result from one of the following: very low blood sugar very high blood glucose levels, also known as hyperglycemic hyperosmolar syndrome Hypoglycemia. Coma from hypoglycemia is more likely to occur from low blood glucose levels if a large insulin overdose is taken or alcohol is in the body during hypoglycemia. The brain is more vulnerable to hypoglycaemia and the consequences of hypoglycemia than any other organ. As the brain levels of glucose fall, the levels of amino acids such as glutamate and aspartate that act as excitatory amino acids are raised. This leads to sodium and water influx causing cellular edema in the brain. Calcium then flows into the cells and causes further dysfunction leading to apoptosis or death of neurons. Diabetic ketoacidosis is a serious complication of type 1 diabetes that arises when levels of ketones in the blood become too high and the acid lev el of the blood increases. It can also result in a diabetic coma.The levels of ketones in the blood can become too high if an individual is using fat rather than sugar as an energy source. People with diabetic ketoacidosis will also have high levels of glucose in their blood since the sugar cannot go from the blood and into the cells. The body tries to reduce the high glucose levels by allowing glucose to leave the body in the urine. However, this also causes the body to lose more water. Hyperglycemic hyperosmolar syndrome (HHS) is a potentially life-threatening condition involving extremely high blood sugar, or glucose, levels. It’s most commonly a result of uncontrolled or undiagnosed diabetes. When glucose level in blood gets too high, the kidneys try to compensate by removing some of the excess glucose through urination. If a patient does not drink enough fluids to replace the fluid he is losing, his blood sugar levels spike. Blood also becomes more concentrated. This condition is called hyperosmolarity. Blood that’s too concentrated begins to draw water out of other organs, including the brain. Before developing a diabetic coma, patients usually experience signs and symptoms of high or low glucose level in blood. Methods of diagnostics Treatment Complications Prevention Hyperglycemia. If level of glucose is too high, patients may experience a very dry mouth, increased thirst, polyuria, fatigue, nausea and vomiting, shortness of breath, pain in the stomach, fruity breath odor, a rapid heartbeat. Hypoglycemia. If level of glucose is too low, patients may experience tremor or nervousness, anxiety, fatigue, weakness, sweating, hunger, nausea, dizziness or lightheadedness, difficulty speaking, confusion. Glucose test Urine test Hypoglycemia requires eating or drinking a source of glucose which can bring blood glucose levels back into the healthy range, and the patient will feel better almost immediately. Treatment for diabetic ketoacidosis includes insulin and fluid. Treatment for HHS involves reversing or preventing dehydration and getting blood glucose levels under control. Prompt treatment can relieve symptoms within a few hours. Left untreated, a diabetic coma can lead to permanent brain damage and death Good day-to-day control of diabetes can help prevent a diabetic coma.