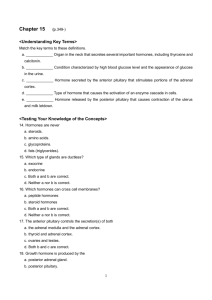
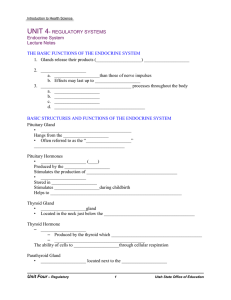
1 Endocrine Pathology Introduction to Endocrine Pathology 1. Importance of the endocrine system a. Regulation of metabolism, development, ion & water balance, reproduction b. Endocrine disorders can severely affect quality of life and can be life-threatening 2. Pathologic changes in blood hormone levels a. Diseases or syndromes are associated with either the hyper or hypo state b. The identity of the altered hormone can indicate where the problem is in the system Diabetes Insulin Effects o Autocrine effect (trophic effect) of insulin acting on Beta cells o Liver Causes glycogen synthesis Causes Lipogenesis o Skeletal Muscle Causes an increase in glucose uptake Causes glycogen synthesis Causes protein synthesis o Adipose Tissue Causes increase in glucose uptake Causes Lipogenesis Diabetes Mellitus Type I Definition - Excessive, sweet urine - diseases characterized by high blood glucose - > 126 mg/dl fasting Insulin Dependent Prevalence - Most common endocrine disorder in the US Diabetes Mellitus Type II 2 - Native Americans (15% of population) - high for black and Hispanic too - 5-10 % Signs / Symptom /- Excessive thirst, frequent urination, increased appetite, poor wound healing Complications - Acute - Dehydration - Hyperglycemia → Glucosuria → ↑Urine volume → Dehydration * Glucosuria = glucose in urine (takes H2O with it) - Early warning signs - excessive thirst and frequent urination - Ketoacidosis (mostly in type I) - ↓Glucose uptake → ↑ FFA → ↑Blood Ketones → Ketoacidosis - Warning sign – fruity smell on breath (due to acetone) - acetone eliminated through lungs - causes coma and death (fatal) - Chronic - chronic complications are part of the top 10 causes of death - contributes to heart disease - Vascular disease ** Cardiovascular disease = leading cause of death in diabetes - Macrovascular disease (arteries) - Atherosclerosis * made worse by hyperlipidemia (High Plasmids) 3 - Microvascular disease (capillaries, arterioles, venules) - Basement membrane thickening in capillaries - Microaneurysms, occlusion, leakage (edema), hemorrhage, neovascularization ** increase glucose covalent binds to protein ** decrease in exchange of nutrients ** leakage and hemorrhage due to fragile veins - Retinopathy (damage to retina) - Caused by… - Microvascular disease - Edematous area, Hemorrhagic area, Neovascularization (more leakage) - Neuropathy - leading cause of acquired blindness in adults - Nephropathy (kidney disease) - Caused by… - Microvascular disease - second leading cause of death in diabetes (behind HD) - Neuropathy -Caused by… - Microvascular disease - nerves not getting normal blood flow or nutrient exchange - decrease in sensation to a painful stimulus * ex. Cannot detect ischemia in leg -> increase in neurotoxicity - Neurotoxicity - Gangrene (req. amputation) 4 - Types of Neuropathy - Peripheral - 50 % of cases (to extremities) - Proximal - trunk - Focal - one area - Autonomic - GI disturbance (diarrhea, constipation) - Heart problem (CVD or angina not detected) 5 Pathogenesis - Weight loss * resolved with insulin (insulin dependent with injection) - during teenage years and insult occurs (virus/chemical) that triggers immune system - Immune system starts destroying Beta cells 1) Eventual decrease in Beta cells via Amyloidosis - Amylin supports action of insulin - deposition of amyloid protein in B cells - toxic -> kills Beta cells 2) Decrease in insulin receptor function (Insulin Resistance to organ tissues) - impaired trophic effect of insulin on Beta cells - Alpha cells experience - no inhibition by insulin (due to resistance) - produce more glucagon (in liver) * INCREASE PLASMA GLUCOSE - Liver experiences - glycogenolysis - gluconeogenesis 6 1) Autoimmune loss of Beta cells 2) causes decrease in insulin * body begins to mobilize energy - Liver experiences - glycogenolysis - gluconeogenesis - Ketogenesis - Ketone (Acetone = product of FFA metabolism) - Skeletal Muscle experiences - decrease in glucose uptake * INCREASE PLASMA GLUCOSE - glycogenolysis - protein catabolism (break down) - Adipose Tissue experiences - decrease in glucose uptake * INCREASE PLASMA GLUCOSE - Lipolysis - triglyceride -> FFA - - Lipolysis - increased glucose output (no A cell inhibition) * INCREASE PLASMA GLUCOSE - Skeletal Muscle experiences - decrease in glucose uptake * INCREASE PLASMA GLUCOSE - Adipose Tissue experiences - decrease in glucose uptake * INCREASE PLASMA GLUCOSE - Adipokines released * (Endocrine function) - causes inflammation - increase insulin resistance ** Aggravating not Causative ** Body cannot produce enough insulin to overcome insulin resistance 7 Treatment - Injections with Insulin (Insulin Dependent) - Long lasting insulin vs instant insulin - causes wide swings in blood glucose - Blood Glucose Levels with injections - Lose Weight - less fat = less inflammation = decreased insulin resistance - Drugs can act on Liver to decrease glucose output - blood glucose levels with Insulin Pump - basal rate of insulin set - Prosthetic pancreas (future) Mechanism of Diabetic Toxicity o Increased Plasma glucose causes… Glucose binds abnormally to proteins AGE (Advanced Glycation End Products) produce Glucose binds to proteins (denature) which can bind to inflammatory receptors – capillary basement membrane thickening Alternate Metabolic Pathways (alternative pathways for sugar) Excess Glycolysis ** 2nd Messengers produced E.g. PKC 8 Abnormal activation causes increase in inflammation and oxidation **All cause…. Capillary basement mebrane thickening Inflammatory Signals Reactive Oxygen Species (ROS) production o Decrease in Insulin and Insulin R signaling Causes… Changes in Growth Factor Signaling o E.g. VEGF (Vascular endothelial growth factor) o GF implicated in neovascularization Abnormal proliferation of blood vessels Insulin Reaction / Insulin Shock o Caused by a diabetic who plans to eat a meal and takes too much insulin o ↑ Insulin → ↑ glucose uptake in fat & muscle → ↓ blood glucose → ↓glucose to brain Brain is not dependent on insulin Decreased glucose to brain causes… Confusion and decreased judgement Leads to death or coma o Other Types of Diabetes Maturity Onset Diabetes of the Young (MODY) Definition - Monogenic - only requires one gene mutation - comes on when young - Not the same as type II Diabetes Mellitus in a young person - 100% genetic Pituitary Introduction o Pituitary has an anterior and posterior lobe Gestational Diabetes - Placental hormones - (cause) - High birth weight - in baby (requires C-section) - 19.2 lbs - Risk of type II - for the mother 9 o A stalk attaches it to the hypothalamus o o o Close to the optic chiasm Within the Sella turcica Anterior Pituitary Pathology Hyperpituitarism o Hypersecreting adenomas Cause of hyperpituitarism state Adenomas (benign) Microadenomas Macroadenomas Definition - < 1 cm - > 1 cm - Hypersecreting - Silent - Secretes excess GH - larger when diagnosed - doesn’t hypersecrete - detected when pushing on cortex and causing moter / sensory problems Prevalence - 10-20 % of older adults have these Interacts with Internal carotid 10 Mass Effects of Tumors - damages pituitary - due to tumor bulk - occupies space that it shouldn’t - Sella turcica erosion (thin bone) - Cerebral Spinal Fluid drips into Sphenoid Cavity - CSF drip out of nose (clear, high Na+, Beta transferrin protein) - Bitemporal Hemianopsia - Temporal Hemianopsia - Bilateral loss of vision due t- compression of optic - Tunnel vision (loss of peripheral vision) - Tumor presses against optic chiasm - Pituitary Apoplexy (stroke) - hemorrhage into an adenoma - rapidly expanding mass causes… - nausea, vomiting, headaches Treatment of - Drugs to shrink tumor Pituitary Tumors - Surgery - though the nostril - breaking through the sphenoid sinus and sell turcica - pull tumor out Adenocarcinomas (malignant) Rare Not hypersecreting (silent) o Hyperplasia Increased cell division o Paraneoplastic Syndromes Hormone-secreting nonpituitary tumors No feedback inhibition with tumors = increased levels of hormones Nonpituitary tumor that hypersecretes a hormone o E.g. lung tumor – ACTH secreted Hypopituitarism o Ischemia, damage due to surgery, radiation, or tumors o Tumors Grows into sell turcica – crusted pituitary 11 Mass Effects of Tumors… Damage to Pituitary Sella turcica erosion (thin bone) o Cerebral Spinal Fluid drips into Sphenoid Cavity o CSF drip out of nose (clear, high Na+, Beta transferrin protein) Bitemporal Hemianopsia o Bilateral loss of vision due t- compression of optic o Tunnel vision (loss of peripheral vision) o Tumor presses against optic chiasm o Pituitary Apoplexy (stroke) o hemorrhage into an adenoma o rapidly expanding mass causes… nausea, vomiting, headaches 12 o Prolactin Disorders o Hyperprolactinemia Hyperprolactinemia Symptom - Amenorrhea – cessation of menstruation - Galactorrhea – inappropriate milk secretion - Makes the disorder easily detectable in premenopausal women - Decreased Libido (sex drive) - Only detectable symptom in men and postmenopausal women Prolactinoma - No symptoms (in men) - Increase in prolactin in plasm - looks like silent tumor in male ** most common type of hypersecreting hormone Cause - Adenomas (Prolactinoma) - Stalk interruption/compression syndrome - ↓portal blood flow → ↓dopamine to pituitary - Drugs - If they block dopamine - less dopamine = increased Prolactin 13 * control of prolactin is many negative (by dopamine (-)) (from hypothalamus) Treatment - treated with dopamine agonists Growth Hormone Disorders o Growth hormone excess Gigantism Cause - Excess Growth Hormone Clinical - increased body size Presentations - 7” foot plus Acromegaly - Thickening of bones in the hands, face, and feet - Growth of soft tissue – tongue, lips, and heart - No additional growth in body size due to epiphyseal closure - Prevalence - Children (before epiphyseal closure) - Adults (after epiphyseal closure) o Growth Hormone Deficiency Pituitary Dwarfism Cause - Deficient GH Clinical - Decreased body size Presentations - normal proportions - Adult Growth Hormone Deficiency (AGHD) - ↑Body fat - ↓muscle and bone mass - weakness - fatigue - depression * Not suspected unless there is pituitary trauma! (surgery, radiation, etc) 14 - not detected bc it looks like normal aging Treatment Prevalence - GH can be administered - children - adults Posterior Pituitary Pathology Diabetes Insipidus Diabetes Insipidus Cause - idiopathic (autoimmune) - tumors - pituitary surgery - head trauma Clinical Presentations Treatment * deficiency of ADH - Antidiuretic hormone (ADH/AVP) → ↑ urine production - increased urine production - treated with DDADP (desmopressin) - replace function of ADH Thyroid and Parathyroid Thyroid Gland Anatomy o Base of neck with two lobes on either side of trachea Thyroid Pathology Goiter o Enlarged thyroid o Cause: Excessive stimulation of TSH receptors (e.g., high TSH) o Nontoxic – low or normal thyroid hormone levels Response of gland to make more TH o Toxic – high thyroid hormone levels Hyperthyroidism o Thyrotoxicosis Hypermetabolic state due to high thyroid hormone levels o Thyroid storm 15 Abrupt-onset, severe thyrotoxicosis Life-threatening due to risk of arrhythmias Due to increased Sympathetic NS and increase in Epinephrine o Signs & symptoms Basal metabolic rate increased (↑ appetite, heat intolerance) Cardiac tachycardia, arrhythmias CNS tremor, hyperactivity, anxiety Ocular staring appearance (eyelid retraction due to ↑ sympathetic NS activity) o Graves’ Disease Graves’ Disease Definition - 85% cause of hyperthyroidism - autoimmune disorder (Graves’ antibodies) Cause 1) Graves’ Antibodies stimulate the TSH receptors on the thyroid 2) increases Thyroid Hormone (TH) synthesis - ectopic synthesis causes DECREASE in TRH and TSH - increased negative feedback to the brain (T3 and T4) - Error! Filename not specified. Diagnosis - Presence of Graves’ Antibodies - decreased TSH Morphology - Thyroid appears… - red and meaty (metabolically active) - moderate goiter Histology Symptom - Proliferation of follicular cells - trying to produce a lot of TH (metabolically active) - Involuting of colloid - moderate goiter 16 - Staring Appearance - Thyroid ophthalmopathy - proptosis or exophthalmos (eyeball protrusion) - Proliferation of preadipocyte fibroblast cells behind orbits, which have TSH receptors (antibody binds and activates) - Inflammation causes increased extracellular matrix & swelling of extraocular muscles Error! Filename not specified. Treatment - surgery relieves pressure - radiation treats inflammation for the thyroid ophthalmopathy Hypothyroidism o Myxedema o Cretinism Myxedema Cause - insufficiency of TH Signs and - Basal metabolic rate symptoms - decreased (fatigue, cold intolerance) - CNS - listlessness, mental Sluggishness - confused / disoriented - decreased performance - Facial changes - edema, broadening of features Cretinism - occurs in children - due to iodine deficiency of Hashimoto’s - Clinical features of myxedema… - Basal metabolic rate - decreased (fatigue, cold intolerance) - CNS - listlessness, mental Sluggishness - confused / disoriented - decreased performance - Facial changes - edema, broadening of Features - Severe intellectual disability * especially if mother had hypothyroidism - Short stature - thyroid hormones are needed for normal GH secretion 17 Treatment - TH with an IV Causes of Hypothyroidism o Iodine Deficiency Dietary iodine is needed for thyroid hormone synthesis A major cause of hypothyroidism in the US before 1924, and still a problem worldwide Formal greatest cause of cretinsim Goiter Belt due to iodine deficiency in water o o Hashimoto Thyroiditis Mild (subclinical) Hypothyroidism Hashimoto Thyroiditis Mild (subclinical) Hypothyroidism Definition - Most common cause of - Normal thyroid hormone levels, but high TSH hypothyroidism in the US - axis is trying to make more TH with increased TSH - Autoimmune destruction of - Subtle signs & symptoms (hyperlipidemia, low blood pressure) thyroid - May progress to Hashimoto thyroiditis - antibodies present - TSH levels increase (no negative feedback due to lack of TH) Treatment - must take Thyroid Hormones - Low blood pressure - treated with low dose of TH Morphology - Thyroid is… - shrunken - fibrotic - non-functional Error! Filename not specified. Histology - thyroid follicles gone - fibrosis and collagen present 18 Thyroid Tumors o Adenomas o Adenocarcinomas Adenomas (Follicular Adenoma) Definition - Benign thyroid tumor - hypothyroid Cause - Almost always from follicular epithelium - Almost always nonfunctional thyroid Prevalence - 10X more common than carcinomas Morphology - encapsulated Error! Filename not specified. Adenocarcinomas - Malignant Thyroid tumor - Major risk factor… - ionizing radiation - from dental x-rays - Most have an excellent prognosis, but some can be aggressive - 100% fatality with some - very invasive - non-encapsulated - invades surrounding tissue Parathyroid Pathology Hyperparathyroidism o Primary Spontaneous overproduction of PTH PTH regulates plasm calcium Hypercalcemia (Ca++) ~80% are due to Parathyroid adenomas (in parathyroid) Parathyroid adenoma causes increase in plasma calcium Bones (Weakness) o Osteoclasts very active Osteoporosis o Osteitis Fibrosa cystica 19 o o Fractures Kidney (Stones) o Nephrolithiasis o Polyuria o Nephrocalcinosis (stones) Brain (Moans) o CNS complaints Depression Lethargy Seizure GI tract (Groans) o Gallstones o Peptic Ulcers o Acute Pancreatitis o Multiple disruptions of GI Secondary PTH overproduction due to low plasma Ca2+ (e.g., kidney disease) Caused by renal failure (excess loss of Ca++ in urine) Problem somewhere else** Hypoparathyroidism o Low PTH levels and hypocalcemia Decrease in plasma Ca++ o Rare o Usually due to surgical removal or damage Thyroid surgery Signs & symptoms o Tetany – muscle spasms due to low Ca2+ (in face, hands, & feet) o Paresthesia – tingling sensations (“pins & needles”) in sensory NS o CNS effects – confusion, mood disorders, seizures Depression anxiety Ca++ makes nerves destabilize with ion channels Adrenals Adrenal Cortex Pathology 20 Addison Disease Cushing Syndrome Addison Disease Definition - chronic adrenal cortical insufficiency - Autoimmune destruction of adrenal cortex (usually) - also TB destroys the cortex Cushing Syndrome - Excessive plasma glucocorticoids - Cushing Disease – hypersecreting corticotroph adenoma - Corticotroph = in pituitary that produces ACTH Signs / - Hyponatremia (low plasma Na+) Symptoms - due to changes in aldosterone - Fatigue & weakness - Stress intolerance - glucocorticoids withstand stress (not enough) - important during surgery - Hyperpigmentation - ACTH molecule similar to Melanocyte Stimulating Hormone (MSH) - initial part of ACTH acts like MSH and stimulates melanocytes in the face - Central obesity (“buffalo hump”, “moon face”) - back of neck and shoulder - Muscle wasting (thin arms and legs) - loss of fat - Abdominal striae – “stretch marks” - from weakened blood vessels - Weakness & fatigue - Osteoporosis - CNS effects (mood disorders, psychosis) - depression, anxiety - Adrenal atrophy or hyperplasia depending on the cause Cause Pituitary Cushing Syndrome 1) Corticotrophs Disease - Tumor in anterior pituitary 2) Tumor releases ACTH (trophic hormone) 3) causes Adrenal hyperplasia 4) Adrenal Cortex releases Cortisol Adrenal Cushing Syndrome 1) Tumor in Adrenal Cortex - releases cortisol - atrophy with tumor 21 - decrease in ACTH 2) Nodular Hyperplasia in adrenal cortex - releases - hypersecretes - decrease in ACTH - not dependent on ACTH Paraneoplastic Cushing Syndrome 1) Nonendocrine cancer produces ACTH - Lung Cancer (or other nonendocrine cancer) - Ectopic Hyperplasia 2) ACTH stimulates Adrenal Hyperplasia in adrenal Cortex 3) Cortisol release * Not involved at pituitary or CNS axis Iatrogenic Cushing Syndrome - Iatrogenic = doctor induced - 95 % 1) Oral glucocorticoids (steroids) 2) Cushing Syndrome occurs - decrease in ACTH 3) causes Adrenal Atrophy Morphology Adrenal Cortex Adenoma Adrenal Cortex Adenoma Definition Benign Adrenal Cortex - Adrenal Atrophy and Adrenal Hyperplasia 22 Morphology - Adenoma - Atrophy to the rest of the gland Symptoms - Weight gain Treatment - remove tumor on Adrenal Cortex Congenital Adrenal Hyperplasia Congenital Adrenal Hyperplasia Pathogenesis 1) ACTH produced from anterior pituitary 2) increase in ACTH = hyperplasia of the adrenal cortex 3) Mutation in enzymes in the steroid synthesis pathway 4) blocks synthesis of aldosterone and cortisol 5) causes increase in ACTH (no feedback inhibition bc of decreased aldosterone and cortisol) 6) Adrenal cortex produces - Progesterone - > aldosterone, cortisol - block decreases Aldosterone (mineralocorticoids) and Cortisol (glucocorticoids) - mediators (progesterone) builds up and is shunted into sex steroid pathway - increase in sex steroids * masculinization of females (young) Symptoms - Masculinization of females - caused by increase in sex steroids due to hyperplasia of adrenal cortex that produces progesterone - Male Pattern Hair grown (Hirsutism) – facial hair (high level of androgens Error! Filename not specified. - decrease in gonadal axis pathway - decrease in FSH and LH levels - Oligomenorrhea (stopped menstrual cycle) - infertility in men (high steroid) Pheochromocytoma 23 Pheochromocytoma Definition - Chromaffin cell tumor that hypersecretes epinephrine & norepinephrine - tumor located in Adrenal Medulla Prevalence - 90 % are benign - rare Signs / - Hypertension & tachycardia Symptoms - due to high plasma epinephrine - Increases HR and BP - Headache - Anxiety (jittery) Treatment - Surgical Removal ** must include antagonists Prevent release of epinephrine during surgery Tumor secretes epinephrine when squeezed Morphology - Tumor on adrenal Medulla _____________________________________________________________________________________ CNS Pathology Anatomy, Cell Types, Edema, Herniations CNS Meninges o Dura Mater Outermost layer Strong Can damage Parenchyma o Arachnoid membrane Spiderweb o Pia Mater Delicate Associated with the surface of the brain o Subdural space Between dura mater and arachnoid mater o Subarachnoid space 24 Between arachnoid and piamater Full of CSF o CNS Vasculature o Circle of Willis Basilar artery and carotids flow in Communicating arteries form a circle Safety mechanism Can compensate when atherosclerosis develops slowly *not when there is an immediate blockage CNS Cell Types o Neuron o Highly susceptible to hypoxia that lasts more than 10 minutes Highly aerobic Glial cells 50 % of cells in brain by volume (outnumber neurons by 50:1) Glia susceptibility to hypoxia is low (can be hypoxic for a while) Oligodendrocyte Responsible for wrapping axons with myelin in CNS Astrocyte End feet on capillaries Project to neurons Participate in synapse Supply nutrients to neurons Buffer environment around neurons to protect Provide electrical insulation Responsible for repair of damage o Gliosis Benign hyperplasia y and hypertrophy of astrocytes Scars in CNS Doesn’t restore function of neuron 25 Microglia For defense macrophage system of CNS Ependymal cells Line the ventricles Cytotoxic and Vasogenic Edema o Cytotoxic Edema Hypoxia or ischemia causes decrease in ATP Can’t run Na+/K+ ATPase Intracellular [Na+] increases Water follows and cells swell Astrocytes, capillary endothelia, and neurons can swell RAPID Response (mins – hrs) Can be reversible o Vasogenic Edema Caused by vasculature Vessels became permeable and filtrate goes into extracellular space Usually blood brain barrier is tight DELAYED Response (Hrs – days) Irreversible damage occurs o Can be fatal (when you drink too much water) Causes Hyponatremia (low plasma glucose) – cell swells Low blood pressure Cerebral Edema Edematous brain Gyri and Sulci are flattened Brain is expanded and pulses against skull 26 o High Altitude Cerebral Edema Progressively worsening headache Caused by low Oxygen in the air Brain Herniations o What kills you with brain edema o Displacement of brain tissue past a rigid partition (fold of Dura Mater) Caused by high intracranial pressure Due to edema hemorrhage or tumor (rapid growth) o Subfalcine Herniation Displacement of cingulate cortex under the falx cerebri (dura) Compresses branch of anterior cerebral artery Interruption of blood flow (infarct) Not as fatal o Transtentorial Herniation Displacement of temporal lobe under Tentorium (dura mater) Compresses an artery or nerve Hemorrhage can occur in pons or midbrain (Duret Hemorrhage) Very fatal or disabled Duret Hemorrhage o Occurs in medulla or pons (artery or vein) o fatal o Tonsilar Herniation Displacement of Cerebellar tonsils through the foramen magnum Medulla is compressed Hemorrhage can occur in pons or midbrain Very fatal or disabled Can be treated with a craniotomy (relieve pressure higher up) 27 Parenchymal and Vascular Trauma CNS Traumatic Parenchymal Injuries o Concussion Concussion Definition - A trauma-induced alteration in mental status - Multiple concussions = accumulating damge Cause - Brain accelerates rapidly around midbrain and brainstem - stretch receptors cause ion channels to open - Results in changes in neural firing Symptom - May or may not cause unconsciousness - confusion, disorientation, nausea, headache o Definition Cause Contusions Laceration - Bruising on impact - Coup – under the site of impact - occurs when head is stationary and is hit by a moving object - Contrecoup – opposite to the site of impact - occurs when object is stationary and is the head hits it (car crash) Morphology - Contusion and bleeding o Laceration Laceration Definition - A penetrating injury causing tearing of tissue - There are sensory nerve endings in the meninges, but not in the brain parenchyma - No pain in parenchyma * Parenchymal injury = no pain (nail in head) 28 o Diffuse Axonal Injury Diffuse Axonal Injury Definition - Swelling and degeneration of axons in white matter tracks \Cause - Caused by traumatic deceleration (car accident) - Axons become stretched - Axons become more permeable to ions - Axons degenera