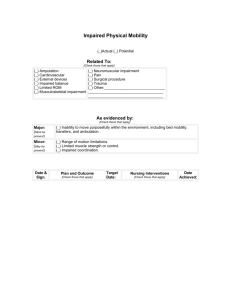
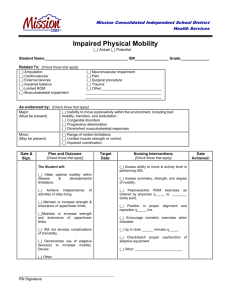
This Photo by Unknown Author is licensed under CC BYNC This Photo by Unknown Author is licensed under CC BY Range of Motion and Joint Mobility PTH5416 Therapeutic Exercise January 27, 2023 Objectives • Understand application of ROM activities as a PT intervention for mobility impairments • Demonstrate PROM, AAROM, AROM to UE • Demonstrate PROM, AAROM, AROM to LE • Demonstrate progression of PROM AAROM AROM • Understand and demonstrate self-ROM activities • Communicate appropriate instructions for activity - Mobility Activities Who: Physical Therapist What: Manual techniques, teach self-mobility, pt education -movement requires different levels of mobility When: May be initiated early and done throughout the rehabilitation program May be prescribed as HEP Where: Joint (capsule, muscle, tendon, ligament), neural, integument, viscera May be prescribed specifically by area of limitation, extremity, total body Why: Bridge the gap from impairment Function (activities and participation) How: Know indications, precautions, contraindications. Choice of mobility activity depends on the stage of healing, length of immobilization, number and kind of tissues affected, and the specific injury or surgery Continuum of Mobility Degree of mobility occurs along a continuum Hypomobility---------------------Hypermobility Hypomobility Decreased mobility At the hypomobility end of the continuum Contracture = a condition of fixed high resistance to passive stretch of a tissue because of fibrosis or shortening of the soft tissues or muscle around a joint Adaptive shortening = shortening of the tissue relative to its normal resting length Can be accompanied by stiffness = resistance to passive movement Hypermobility Excessive mobility-Should not be confused with instability Instability = an excessive range of osteokinematic or arthrokinematic movement for which there is no protective muscular control Flexibility The ability to move a joint or a series of joints through AROM Relative flexibility-Considers the comparative mobility at adjacent joints Relative Flexibility Comparative mobility at adjacent joints If hypomobile Adjacent segments/joints are hypermobile Copyright © 2018 Wolters Kluwer • All Rights Joint Mobility Arthrokinematics • Movements of the joint surfaces • Descriptive terms—roll, spin, glide • Necessary component of osteokinematic motion Osteokinematics • Movements of the bones • Described in terms of planes or relative movements Morphology and Physiology of Normal Mobility Normal mobility includes Osteokinematic motion Arthrokinematic motion Adequate tissue length to allow full range of motion Neuromuscular coordination and skill to accomplish purposeful movement Loss of Mobility Reasons Trauma to soft tissue, bone, or other joint structures Surgery Joint disease Prolonged immobilization Neuromuscular disease Pain come addfore 1 Self-Perpetuating Cycle of Immobility • Examination of movement impairments therapeutic interventions • Necessary for functional movement • Involves muscles, jt surfaces, capsules, ligaments, fasciae, vessels, nerves • As a treatment intervention, administered to maintain joint and soft tissue mobility to minimize loss of tissue flexibility and contracture formation • Principles of ROM-don’t encompass stretching to increase ROM & ROM > ROM is than different stretching Range of Motion (ROM) • Dosage • Volume should be sufficient to achieve the physical therapy goal without overloading the tissues • Depends on the purpose of the activity • Slow rhythmical motion • 5-10 repetitions depends on • Objectives of the program • Patients condition • Response to the treatment • Progression • Passive ROM (PROM) • Active assisted ROM (AAROM) -active ROM (AROM) • Active ROM (AROM) Passive Range of Motion (PROM) • Performed by external force • Performed without any muscular activation • Performed within the available ROM • Any overpressure at the end of the range = stretching • PROM is NOT the same as passive stretching • PROM and stretching can be combined PROM: Indications • PROM is used when • Active movement may disrupt the healing process • Surgical repair of contractile tissue that would compromise repaired muscle • Patient is physically unable or not supposed to move actively • Teaching active or resistive exercises • Relaxation is the goal PROM: Goals • Maintain joint and connective tissue mobility, mechanical elasticity of muscle • Minimize negative effects of immobilization/disuse • Prevention of joint contractures and soft-tissue stiffness or adaptive shortening • Decrease/inhibit pain • Assist circulation, vascular dynamics and synovial diffusion Passive Range of Motion: Types/Modes • Manual • PT • Family members • Self Assisted ROM • Pulleys • Various household objects • Mechanical • ie Continuous passive motion devices (CPM) Continuous Passive Motion (CPM) • Mechanical device that moves a joint slowly and continuously through controlled ROM • Benefits • • • • • • • Prevents adhesions and contractures, joint stiffness Stimulating effect on healing of tendons and ligaments Enhances healing of incisions over moving joints Synovial fluid lubrication intra-articular cartilage healing/regeneration Prevents negative effects of immobilization Quicker return of ROM Decrease post op pain after commonlyused > knee post surgery CPM Research support for short term benefits Long term functional gains reported to be no different than using other forms of mobility Considerations Detrimental effects Cost effectiveness Pt compliance Supervision of equipment Length of hospital stay (LOS) Appropriate populations (Can • PROM • UE • LE • AAROM • UE • LE • AROM • UE • LE • Cervical • Spine Let’s Practice use worksheet to make notes and document practice) ROM: Pt. Preparation • Set Up • Free from restrictive clothing, linen, splints, dressing. Drape appropriately • Position patient for comfort and safety, alignment and stabilization for room to move body part through ROM • Clear environment to be able to move body segment through ROM • Communicate with patient-plan and method of intervention Range of Motion: Techniques Techniques: • Support any areas at risk of injury • Use firm and supportive grip at joints (avoid excessively tight grip) • Perform slowly and rhythmically • Move through full pain-free range to the point of tissue resistance • Ensure clinician safety by use of body mechanics • Use • cardinal plane motions • combined motions • functional movement patterns Passive Range of Motion (PROM) • Considerations • Ensure patient is passive • No assistance provided by muscles that cross joint • Perform slowly and rhythmically through available pain free range • To the point of slight tissue resistance • Provide appropriate support at surrounding joints Active Assisted Range of Motion (AAROM) • Considerations • Mobility activities in which some muscle activation takes place • Has little impact on true strength gains in most patients –teaches the patient how to actively fire the muscle • Involves the patient in the rehabilitation process Active Assisted Range of Motion: Indications AAROM is used when • the patient is unable or not allowed to fully activate the muscle • some muscle activation through the ROM is allowed or desired, but the patient requires some assistance to complete the ROM • initiating gentle muscle activity after musculotendinous surgical procedures Active Assisted Range of Motion: Goals • Prevention of the negative effects of immobilization • Prevention of joint contractures and soft tissue tightness • Decreased pain • Enhanced vascular dynamics and synovial diffusion • A stimulus for bone activity from the pull of the muscle on the bony attachment • Muscle activity • Enhanced proprioception and kinesthesia Active Assisted Range of Motion: Techniques Techniques • Hand placement and cueing • The amount of assistance throughout the ROM may vary • May be based on amount of participation prescribed • May be based on how much pt is able to do Active Range of Motion (AROM) : Indications When is AROM used? • When active muscle contraction is desired (see goals) • To ensure proper exercise performance before the addition of resistance Active Range of Motion: Goals • Prevention of the negative effects of immobilization • Prevention of joint contractures and soft-tissue stiffness or adaptive shortening • Decrease pain • Increased blood flow and synovial diffusion • A stimulus for bone activity from the pull of the muscle on the bony attachment • Enhance proprioception and kinesthesia • Progression to build in neuromuscular component of movementrequires more muscle coordination only those we fair (315) strength or legs can be ... Active Range of Motion: Techniques Techniques • Ensure that muscle activation is warranted & determine precautions • Physical therapist to demonstrate the exercise to be performed • Or passively take the patient through the ROM • Can be performed against gravity or in a gravity-minimized position • Speed, ROM, posture and quality of movement should be monitored Self-Assisted ROM (S-AROM): Indications/Goals • Promote self-care • Protects healing tissue when more intensive muscle contraction contraindicated • HEP Self- Assisted ROM Activities: Techniques Self-Assisted Range of Motion Educate pt on value of motion Teach correct body alignment/stabilization Observe and correct substitute or unsafe motions Can use normal extremity or equipment-Assure hazards are eliminated Provide drawings and guidelines for dosing This Photo by Unknown Author is licensed under CC BY Self- Assisted ROM Activities (cont’d) • Considerations • Pt’s strength, control, balance and coordination, desired working range, joint biomechanics • Pt ability to assume position for activity-can use variety of positions • Use horizontal and vertical surfaces • Horizontal-tabletops, desktops, floor, bed • Vertical-wall, doorway, door • Add towel, pillowcase, mitten, etc to decrease friction • Dose as though physical therapist is doing activity • Examples Horizontal & Vertical Surfaces Self-Range of Motion Supine Shoulder Flexion Allows the final range of shoulder flexion to be assisted by gravity Self-Range of Motion Sitting/Standing Shoulder Flexion The resistance (because of gravity) increases as the upper extremity approaches 90º flexion and continues to be resisted by gravity Independent ROM Activities • Wand (T-bar) activities • Wall climbing • Overhead pulleys • Skateboard/Powder board • Towels, sheets, belt • Reciprocal exercise unit • Aquatic Environment • The water’s buoyancy makes upward movement easier than on dry land • Functional patterns Questions?????? • COMING UP • Next Week • Tuesday Mobility • Stretching, Mobilization, Stabilization • Neural Mobility (practice neural mobility positions as described on neural tension handout on canvas) • Friday-Mobility Lab • Manual stretching, Self-stretching • Quiz # 1 Due 2/5 • Prep for Skill check • Lab topics listed except self-stretching (will cover more in second half of semester-expect on final practical), includes progression/regression