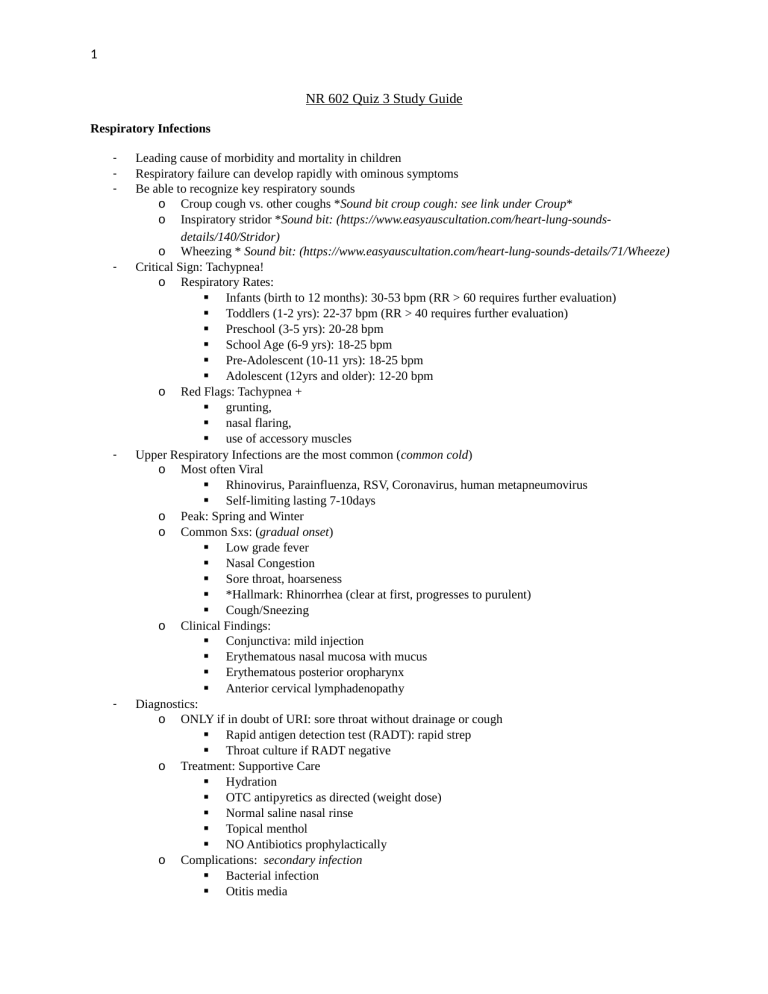
1 NR 602 Quiz 3 Study Guide Respiratory Infections - - - - Leading cause of morbidity and mortality in children Respiratory failure can develop rapidly with ominous symptoms Be able to recognize key respiratory sounds o Croup cough vs. other coughs *Sound bit croup cough: see link under Croup* o Inspiratory stridor *Sound bit: (https://www.easyauscultation.com/heart-lung-soundsdetails/140/Stridor) o Wheezing * Sound bit: (https://www.easyauscultation.com/heart-lung-sounds-details/71/Wheeze) Critical Sign: Tachypnea! o Respiratory Rates: Infants (birth to 12 months): 30-53 bpm (RR > 60 requires further evaluation) Toddlers (1-2 yrs): 22-37 bpm (RR > 40 requires further evaluation) Preschool (3-5 yrs): 20-28 bpm School Age (6-9 yrs): 18-25 bpm Pre-Adolescent (10-11 yrs): 18-25 bpm Adolescent (12yrs and older): 12-20 bpm o Red Flags: Tachypnea + grunting, nasal flaring, use of accessory muscles Upper Respiratory Infections are the most common (common cold) o Most often Viral Rhinovirus, Parainfluenza, RSV, Coronavirus, human metapneumovirus Self-limiting lasting 7-10days o Peak: Spring and Winter o Common Sxs: (gradual onset) Low grade fever Nasal Congestion Sore throat, hoarseness *Hallmark: Rhinorrhea (clear at first, progresses to purulent) Cough/Sneezing o Clinical Findings: Conjunctiva: mild injection Erythematous nasal mucosa with mucus Erythematous posterior oropharynx Anterior cervical lymphadenopathy Diagnostics: o ONLY if in doubt of URI: sore throat without drainage or cough Rapid antigen detection test (RADT): rapid strep Throat culture if RADT negative o Treatment: Supportive Care Hydration OTC antipyretics as directed (weight dose) Normal saline nasal rinse Topical menthol NO Antibiotics prophylactically o Complications: secondary infection Bacterial infection Otitis media 2 - Sinusitis Asthma exacerbation Pharyngitis, Tonsillitis, and Tonsillopharyngitis o Inflammation of mucosal lining of the throat structures o Infectious or noninfectious causes Viral or bacterial Viral (most common): adenovirus (pharyngitis primary sx), Epstein-Barr (EBV), herpes simplex (HSV), cytomegalovirus (CMV), enterovirus, parainfluenza, HIV o Upper nasal symptoms, cough and rhinorrhea, hoarseness, conjunctivitis, rash, diarrhea o Occur year round, except adenovirus which is predominantly summer (contaminated swimming pools) Bacterial: GABHS (most common in 5-13 year olds), gonococcal (15-19 year olds), Corynebacterium diphtheria (RARE), Arcanobacterium haemolyticum, Neisseria gonorrheae(adolescents), Chlamydia trachomatis (adolescents), Francisella tularensis, Mycoplasma pneumonia, Group C & G Strep o GABHS: typically late winter and early spring o Acute abrupt onset: sore throat, headache, nausea, vomiting, abdominal pain, myalgia, arthralgia, malaise Respiratory irritants (smoke) o Clinical Findings: Erythematous tonsils and pharynx EBV: exudates on tonsils, petechiae on soft palate, diffuse adenopathy Adenovirus: follicular pattern on pharynx Enterovirus: vesicles or ulcers on tonsillar pillars, coryza, vomiting, diarrhea Herpes: anterior ulcers, adenopathy Parainfluenza and RSV: lower respiratory sx, stridor, rales, and wheezing Influenza: cough, fever, systemic sxs M. pneumo & Chlamydophila pneumo: cough, pharyngitis GABHS: exudative Erythematous pharyngitis with follicular pattern without presence of cough or nasal symptoms, swollen beefy red uvula, enlarged tonsillopharyngeal tissue, anterior cervical lymphadenopathy, bad breath, scarlatiniform rash, strawberry tongue A. haemolyticum: exudative pharyngitis, marked erythema and pruritic, fine scarlatiniform rash o Diagnostics: RADT and/or throat culture if >3 years old with pharyngitis or if someone in household is + Strep Culture if RADT negative, or suspect A. haemolyticum, N. gonorrhea or C. diphtheria If suspect Mononucleosis: CBC o Treatment: Supportive care: ibuprofen, acetaminophen Hydration GABHS with + RADT or + culture: antibiotics PCN V potassium – 1st choice Amoxicillin suspension Benzathine pcn G IM Allergy to PCN: o Cephalexin o Cefadroxil o Clindamycin (1st choice if chronic symptomatic carriage of GABHS) 3 o Azithromycin o clarithromycin If CMV or EBV: beta-lactam antibiotic causes diffuse morbilliform skin eruption Discard/Clean: bathroom cups, toothbrush, orthodontic devices Return to school when afebrile or on antibiotic for 24 hours Tonsillectomy/adenoidectomy: if > 7 throat infections in past year, >5 throat infections in past 2 years, >3 throat infections per year x 3 years sleep apnea adenoid hypertrophy unresponsive rhinosinusitis chronic otitis media (post tympanostomy tube placement) Sinusitis/Rhinosinusitis - - - URI lasting 10 to 14 days with no symptoms improvement or worsening symptoms o Acute (ARS): lasting as long as 4 weeks o Chronic (CRS): persist 12 weeks or more Inflammation and edema of mucous membranes lining the sinuses Bacterial: Strep pneumo., H. influenza, Moraxella catarrhalis, Staph. Aureus (less often) Risk factors: o Preceding infection o Environmental irritants/allergies o Anatomic problems (septal deviation, nasal polyps, facial trauma) o GERD o CF, ciliary dyskinesia o Immunodeficiency Clinical Findings: o Thick, yellow discharge o Worsening symptoms after initial improvement from URI o Sx: headache, fatigue, decreased appetite o Bad breath (halitosis) o Facial pain* o Facial/nasal congestion and fullness* o Purulent postnasal drainage and nasal discharge o Cough o Ear pain/fullness/pressure Treatment: o Watchful waiting: do not over use antibiotics Symptom management: ibuprofen, acetaminophen Rest Reassess after 72 hours o Chronic: referral to ENT o Antibiotics Criteria per AAP Guidelines: URI with persistent nasal discharge, daytime cough, lasting >10 days without improvement URI with worsening symptoms, new onset of fever, nasal discharge, or daytime cough after initial improvement Fever > 102.2 F (39 C) with purulent nasal discharge for at least 3 days and sinusitis Amoxicillin – 1st line x10-28 days or 7 days past symptom resolution 45 mg/kg divided into 2 doses/day S. pneumo: 80-90 mg/kg/day (max: 1000 mg/dose) 4 Child < 2 yrs, daycare attendee, recent antibiotic use, or severe illness: Augmentin 80-90 mg/kg/day of amoxicillin part (max: 2 grams/dose) Vomiting: ceftriaxone 50 mg/kg IV or IM PCN allergy type I: 3rd generation cephalosporin (cefdinir, cefpodoxime, cefuroxime) Bronchitis/ Bronchiolitis/ Respiratory Syncytial Virus (RSV) - - - - - - inflammatory process of the bronchus, or bronchioles (small airways) most commonly caused by a Virus o MOST Common: Respiratory Syncytial Virus (RSV) o Others: influenza, parainfluenza, adenovirus, enterovirus, bocavirus, and rhinovirus o Rarely: can have rare bacterial cause: Mycoplasma pneumonia Highly CONTAGIOUS Direct Contact and Droplet Transmission o Incubation period before symptoms start High Risk: children with o Prematurity o Chronic lung disease o Immunocompromised o Participating in Day Care Symptoms: o Starts as URI o Worsening cough o Rhinorrhea o *HALLMARK: Wheezing Exam Findings: o Increased work of breathing o Prolonged expiration o Intercostals retraction o Grunting o Nasal flaring o Wheezes and crackles *Sound bit: polyphonic wheeze found in RSV: (https://www.easyauscultation.com/heart-lung-sounds-details/144/Wheeze-Polyphonic), crackles (https://www.easyauscultation.com/heart-lung-sounds-details/72/Crackles-Fine-(Rales)) o Abdominal distention, palpable liver and spleen o Chest X-ray (not typically done): hyperinflation, atelectasis, flattening diaphragm Complications: may progress to o Pneumonia o Respiratory distress and hypoxia o Respiratory acidosis Treatment: o Supportive Care Monitory pulse oximetry and respiratory status Supplemental Oxygen Hydration (oral, NG, IV) Nutrition Suction o Hospitalization Age < 2 months Respiratory distress Progressive stridor or stridor at rest Apnea 5 RR > 50-60 bpm (sleeping) Cyanosis, hypoxia Inability to tolerate oral feeding Depressed sensorium Presence of chronic cardiovascular or immunodeficiency disease Pertussis “Whooping Cough” - - - - Gram-negative bacillus: Bordetella pertussis Hallmark: high-pitched inspiratory whoop follows by spasms of coughing *Sound bit: (https://www.youtube.com/watch?v=zuK4honWVsE) Aerosol droplet transmission 7-10 day incubation, most contagious during first 2 weeks Cough lasts 6-10 weeks (possibly longer in adolescents) Vaccination: DTaP or Tdap Symptoms: o Most severe in infants < 6 months Apnea Seizures induced by hypoxemia Cough without inspiratory whoop Tachypnea Poor feeding Leukocytosis nad lymphocytosis Diagnostics: o Gold standard: culture with Dacron or Calcium alginate swab of nasopharynx (only 12%-60% specific) o PCR (improved sensitivity) Treatment: o Macrolide (not in infants < 1 month due to pyloric stenosis) Azithromycin – 1st line Clarithromycin Erythromycin o Macrolide allergy: Bactrim o Chemoprophylaxis in household and close contact exposure: monitor x 21 days Prevention o “Cocooning”: vaccination of all adults and relatives close to infant and protection from environmental hazards o Vaccinate Pneumonia - Bacterial or Viral o Bacterial: less common in childhood S. pneumo. Most common cause Lobar pneumonia Methicillin resistant Staph aureus(MRSA) Community acquired Empyema Necrosis o Viral: 6 - - - - - - More common in children < 2 yrs Gradual onset Typical or Atypical o Typical: lobar, infection of alveolar space resulting in consolidation o Atypical: non-localized consolidation Walking pneumonia Risk factors: neonates o Prolonged rupture of membranes o Maternal amnionitis o Premature delivery o Fetal tachycardia o Maternal intrapartum fever o Airway anomaly Symptoms (vary by age group): o Neonates: *Fever, irritability, lethargy o Older Children: *Cough *Fever Tachypnea, tachycardia, air-hunger Downward displacement of liver and spleen Obvious illness (lethargy, decreased appetite, look unwell) o C. trachomatis: repetitive staccato cough with tachypnea, cervical adenopathy, and crackles Treatment: o If sxs not improving after 72 hours: Chest x-ray o Neonates: admit to hospital o Supportive care: Antipyretics Hydration Rest o Antibiotics: by age and causative organism Chlamydia: azithromycin or amoxicillin, erythromycin, ethyl succinate C.pneumo, M. pneumo: azithromycin, macrolide+ beta-lactam S. pneumo: 3rd generation cephalosporin S. aureus: vancomycin, clindamycin + beta-lactam Complications: o Respiratory Distress, pneumothorax o Meningitis o CNS abscess o Endocarditis, pericarditis o Osteomyelitis, septic arthritis Vaccination: Prevnar 13 Rotavirus Croup 7 - - - - Viral infection of the middle respiratory track (Larynx and bronchial tree Laryngotraceitis / Laryngotracheobronchitis (LTB) o Viral: parainfluenza type 1 & 2 (HPIV) o LTB more severe, occurs 5 – 7 days in to the disease Usually children < 6 yrs Season: fall and winter Incubation period: 2-4 days with viral shedding up to 1 week, lasts approx. 5 days HALLMARK: Barking Cough *Sound bit: 1, 2, 3 (https://mommyhood101.com/croup-audio-clips Diagnosis: made by symptoms/clinical presentation Symptoms: o Low grade fever o URI symptoms- gradual onset (rhinorrhea, congestion) o Barking Cough o Hoarseness o Dyspnea o Respiratory Distress (Intercostal retraction, tachypnea, cyanosis, accessory muscles, nasal flaring) Clinical Findings: o Tachypnea o Prolonged inspiration o Inspiratory stridor (as airway obstruction worsens) *Sound bit: 4, 5 (https://mommyhood101.com/croup-audio-clips) o Wheezing (if lower airway involved) o Chest X-Ray (not typically done): subglottic narrowing – Steeple Sign Treatment: o Supportive Care: Symptom Management Cold air Hydration o Glucocorticoids: reduce airway swelling Dexamethasone 0.6 mg/kg to1 mg/kg IM PO o Aerosolized racemic epinephrine: reduce swelling of larynx and subglottis o Bronchodilator o Hospitalization: RR > 70 bpm Stridor at rest Temperature > 102.2 F (39C) Complications: o Pneumonia o Respiratory distress Epiglottitis - Inflammation of epiglottis, aryepiglottic folds, and ventricular bands at the base of the epiglottis Cause: H. influenza type B (HiB) Prevention: HiB vaccine Typically age 1-5 yrs (most under 2 yrs) Symptoms: o Abrupt onset fever o Severe sore throat o Dyspnea o Inspiratory distress without stridor o *drooling o Toxic look 8 - - - Clinical Findings: Emergent- Death within hours o * If epiglottitis is suspected: do NOT examine throat, do NOT place in supine position, Immediately transfer to ER o Expiratory stridor o Drooling o Aphonia (muffled, ‘hot potatoe’ voice) o Rapid progression of respiratory obstruction o High fever o Flaring ala nasi and retraction of supraclavicular, intercostals, and subcostal spaces o Hyperextension of the neck Diagnostic: o Blood culture o Lateral neck radiograph: absence of ‘thumb’ sign rules out condition o Confirmed in OR Treatment: o Establish airway (possible intubation or tracheostomy) o Start antimicrobials IV broad spectrum Rifampin prophylaxis to all household members (20 mg/kg, max: 600 mg, x 4 days) o O2/ respiratory support Foreign Body Occlusion/ Aspiration Nasal Occlusion - - Symptoms: o Recurrent, unilateral purulent nasal discharge o Foul odor o Epistaxis o Nasal obstruction/ mouth breathing Detection of FB in nasal passageway Removal: o Alligator forceps o Suction with narrow tips o Cotton tipped applicators w/ or w/o topical vasoconstrictor o Hook or curette o 5-Fr catheter balloon inflation behind FB o Refer to ENT Laryngeal FB Aspiration - Symptoms: o Rapid onset hoarseness o Croupy cough o Aphonia Tracheal FB Aspiration - Symptoms: o Brassy cough o Hoarseness o dyspnea Bronchial FB Aspiration 9 - - - - Symptoms: o Unilateral wheeze, usually aspirated into *Right lung o Recurrent pneumonia o HX of Choking episode Clinical Findings: o Cyanosis o Hemoptysis, blood streaked sputum o Decreased vocal fremitus o Limited chest expansion o Diminished breath sounds o Unilateral wheezes Tracheal: homophonic wheeze: wheeze with audible ‘slap’ and palpable ‘thud’ on expiration Diagnostic: o Inspiratory and forced expiratory chest radiographs o Chest fluoroscopy Treatment: Referral to Pulmonary Specialist Complications: o If vegetable matter: severe condition Fever, sepsis-like sxs, dyspnea, cough o Lobar pneumonia o Status asthmaticus o Emphysema, atelectasis Prevention: Education on high risk foods/objects: o Carrots, nuts, popcorn, hot dog chunks o Small toys, coins, buttons, etc Restrictive Airway Diseases - Less common in pediatrics Decreased lung compliance with relatively normal flow rates HALLMARK: tachypnea and decreased tidal volume/capacity Causes: o Neuromuscular weakness o Lobar pneumonia o Pleural effusion or mass o Severe pectus excavatum o Abdominal distention Asthma *Know Levels of severity* Cystic Fibrosis (CF) - Genetic disorder, autosomal recessive, mutation of CFTR protein on chromosome 7 Multisystem, progressive disease: COPD, GI disturbances, *exocrine dysfunction Life expectancy: 41 yrs Symptoms: o Respiratory: chronic airway inflammation and lung infections, viscous mucus, *mucociliary transport dysfunction, chronic cough, and *excess sputum production, respiratory failure 10 GI: meconium ileus, pancreatic insufficiency, rectal prolapsed, GI obstruction, failure to thrive, edema, hypoproteinemia, steatorrhea, poor muscle mass, GERD, *vitamin deficiencies (A, K, E, D) o Hepatic: biliary cirrhosis, jaundice, ascites, hematemesis, esophageal varices, cholelithiasis o Endocrine: recurrent acute pancreatitis, CF related diabetes (CFRD) o Musculoskeletal: osteoporosis o Reproductive: delayed sexual development, nonfunctional vas deferens (male sterility), undescended testes, hydrocele, demale decreased fertility, cervicitis o Sweat: *“taste salty”, hypochloremic alkalosis, dehydration Diagnostic: o Newborn screening performed o Gold Standard: pilocarpine iontophoresis sweat test Only ordered if child has more than one clinical feature of CF Sweat chloride concentration > 60 mmol/L (age > 6 months), > 30 mmol/L (in infants) o PFTs o Glycosylated hemoglobin (elevated) Treatment: complicated, require multidisciplinary team o Pulmonary: promote airway clearance Inhaled dornase alfa :reduce mucus viscosity Hypertonic saline: thins mucus Postural drainage (cycle: active breathing, autogenic drainage, percussion, positive expiratory pressure, exercise, high frequency chest wall oscillation) BID High dose Ibuprofen: reduce airway inflammation Azithromycin 3x/week (ibuprofen decreases neutrophil mitigation) Lung transplant o GI: Pancreatic enzyme supplementation Vitamin replacement and serum monitoring (A, D, E, K) Osmotic laxatives, Gastrografin enemas o Endocrine Glucose tolerance test Diabetes management o - - Salmonella Clostridium difficile Cryptosporidium Pyloric Stenosis Pinworms 11 Gastric Esophageal Reflux (GERD) - Common in young infants: anatomical reasons o Spitting up after meals Foreign Body Ingestion - Common in children exploring their environment with mouths and hands Common locations: o Thoracic inlet, pyloris, ileocecal junction Common Culprits: Coins o Most pass without problem; 10-20% need surgery Symptoms: o Dysphagia o odynophagia, o drooling, o regurgitation, o abdominal pain, o difficulty breathing Urinary Tract Infection - - - More common in females > uncircumcised male > circumcised males o Girls who have > 2 UTIs, urology consult is recommended o Boys who have >1 UTIs, urology consult is recommended Lower UTI: uncomplicated, bladder and urethra Upper UTI: complicated, urethra, bladder, ureters, kidneys o May require hospitalization Fluid stabilization Treatment Monitoring for sepsis Risk Factors: o Perineal irritation (soaps, bubble baths, fragrances, wipes) o Not wiping front to back o uncircumcised Symptoms: o Infants: Fever/hypothermia Jaundice Poor feeding Irritability Vomiting Strong smelling urine Failure to thrive Sepsis o Children: Abdominal/ flank pain Urinary frequency Dysuria Urgency Enuresis 12 - - Vomiting Fever Diagnostics: o Urinalysis o Urine culture and sensitivity o Gram stain o Hydration status and electrolyte values Most common cause: E. coli (85%) o Others: Klebsiella, Proteus, Enterococcus, Staphylococcus, and Streptococcus Treatment: dependent on culture, child’s age, and clinical guidelines Primary Enuresis Glomerulonephritis - Result of renal insult caused by immunoglobulin damage to the kidney Red Flag: hematuria Types: o Post-infection: most common Post-streptococcal infection: occurs 10 to 14 days post-primary infection Sx: edema, renal insufficiency Dark, tea-colored urine o Membranoproliferative o IgA nephropathy o Henoch – Schonlein purpura (HSP): Most common cause of small vessel vasculitis in children 2-7 yrs old Sx: itching, urticaria, maculopapular rash with purpura on legs, buttocks, and elbows Joint pain 50% chance of renal involvement o Systemic lupus o Alport syndrome Osgood-Schlatter Juvenile Rheumatoid Arthirits Osteomyelitis Transcient Synovitis of the Hip Legg-Calve’ – Perthes Disease 13 Idiopathic Scoliosis 1. 2. How should the APRN teach the parents to manage the child’s symptoms? Fevers in children under 36 months of age can have potentially serious consequences. For a 2 month old infant, which tests should the APRN considering ordering?