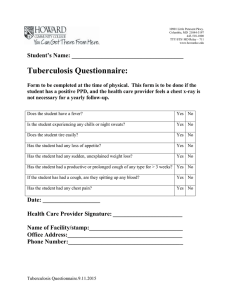
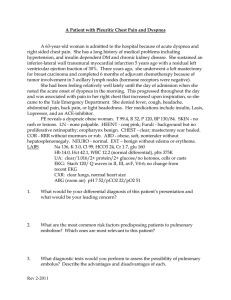
Clinical OSCE of internal medicine 1. History taking 2. General examination 3. Abdominal examination - GI bleeding - Diarrhea - Pancreatitis - Cholangitis - Gastritis - Hepatitis - GERD - Dysphagia 4. Cardiovascular examination - Heart failure - Ischemic heart disease - Pericarditis - Endocarditis - Valvular heart disease - Palpitations - Aortic dissection 5. Respiratory examination - Pneumonia - Bronchiectasis - Asthma & COPD - Dyspnea & cough & hemoptysis* - Pulmonary embolism - Tuberculosis 6. Rheumatology examination - Acute arthritis - Chroinc rheumatoid arthritis - Spondylo arthopathy - Connective tissue diseases Done by: Randa Altuwaijri Please note that I am not responsible for the accuracy of the information in this summary. It’s up to you to study it. Abdominal examination GI bleeding Hemoptysis vs. Hematemesis? Presentation Hematemesis – bright red/coffee-ground Melena – distinctive smell, tar-like Dyspepsia, Dizziness, Chest pain Prolonged vomiting/retching Past Hx Previous bleeding Known peptic ulcer, varices, liver, cardiovascular, respiratory disease Malignancy Medical: NSAIDs, Steroids, Anticoagulants Social: Alcohol consumption Diarrhea Acute vs. Chronic? Small vs. Large? Presentation Enterotoxic (Extracellular volume depletion) Recent use of antibiotics – C.diff Medium cooked hamburger – ETEC Contaminated water – V. Cholera Carbs food – S. Auras Reheated rice – B. Ceruses Camping/fresh water – Giarrdia Invasive (Fever & peritoneal signs) Raw eggs – Salmonella Hemolytic-urimic/meat – shigella/EHEC HIV – A. Haemorrhagic Compylobacter Examination Signs of chronic liver disease: jaundice/pallor, legs/ankles oedema, Itchy skin, Dark urine, Pale stool, spider nevi, gynecomastia, caput medusae, clubbing. DRE for melena R/O orthostatic hypotension (20-10 rule) Signs of shock & Encephalopathy History Passage of 6 or more per 24 hours Low/High Stool volume & frequency Stool characteristics (appearance, blood, mucus, oil droplets, color, food) Associated symptoms (pain, fever, W loss) Relationship to foods, fasting, & stress hospitalizations, antibiotics, radiation Emergency Management Variceal ABC – intubation: vomiting/ loss conscious IV fluid resuscitation – Kg x 20 Chest/Abdominal X-Ray – gases in cavities Foley’s catheter – accurate fluid balance Transfusion – haemodynamically↓ / Hb 7-8 Proton-pump inhibitors – PPIs, H2-RA Prokinetic – Metoclopramide Broad-spectrum antibiotics – IV Tazocin Vasoconstriction – IV Terlipressin Endoscopy – with in 12h Band ligation – oesophageal varices N-butyl-2-cyanoacrylate – gastric varices Surgery – stent, balloon, TIPSS Drug: PPI, BB, Statins, NSAID, SSRI Allergy: Drugs, IBD, Food Social: travel, camping, Alcohol, coffee NonVariceal Same as above plus: Prokinetic – erythromycin Endoscopy – within 24h Clips +/- adrenaline Fibrin/thrombin Thermal coagulation Scoring system - Forrest – Bleeding character - AIMS65 – mortality prediction Examination Dehydration Orthostatic changes Fever Bowel sounds Hepatomegaly DRE & FOBT Skin, joints, thyroid Evaluation CBC (Hct, MCV, WBC count) electrolytes, BUN, glucose, Ca, albumin TSH, B12, folate, INR/PTT, Vit D, iron IBD panel; calprotectin, CRP, ESR, LFTs Stool studies (Culture, leukocytes, occult blood, pH, fat & Laxative screen) Management Oral rehydration solutions/ IV fluid Empiric antibiotic - fluoroquinolone Antimotility - loperamide/Diphenoxylate Adequate nutrition - Boiled starches Pancreatitis I GET SMASHED Gastritis histological diagnosis, endoscopy Presentation Severe epigastric pain, radiating to the back worse lying down/relieved sitting forward Presentation Acute Erosive and hemorrhagic Neutrophils Use of aspirin or NSAID Dyspepsia, anorexia, N/V hematemesis, melaena History Recent excess alcohol intake Previous gallstone disease or ERCP Family history of gallstones, Pancreatitis Examination Tachycardia, Fever, Jaundice Epigastric tenderness, Rigidity Reduced or absent bowel sounds Cullen’s & Grey-Turner’s sign Evaluation Typical abdominal pain Amylase or Lipase 3 or more Radiologic findings Management Null Per Oral Intravenous fluids 20ml per Kg then 3ml Oxygen supplementation +94% Analgesia: acetaminophen, morphine Thromboprophylaxis - heparin Antibiotics - if infection only CT abdomen - after 6-10 days ERCP - within 72h Alcohol avoidance Cholangitis Presentation Charcot’s triad (Jaundice, Fever, RUQ pain) History Obstruction gallstones Infection post-ERCP Autoimmune PSC, PBC Tumour/HIV/Roundworm Evaluation Blood tests (CBC, Urea, Clotting) Blood cultures (E.coli, Klebsiella) Imagining (AXR, USS, CT) Management IV fluid resuscitation & Foley’s catheter IV antibiotics (Tazocin) & ICU management ERCP within 24h (Dx and Tx) Chronic lymphocytes & plasma cells dyspepsia, H. pylori Management antacids, PPIs, prokinetics, antiemetics + H. pylori eradication Peptic Ulcer HP, NSAID, stress Presentation Abdominal pain (burning, vague discomfort, fullness, cramping) Awaken patients from sleep 12- 3 AM Nausea, vomiting, and anorexia Relieved by food = DU Evaluation upper endoscopy, mucosal biopsy serologic antibody detection urea breath test (UBT) stool antigen test Management Nonpharmacological Reduce stress Stop smoking and NSAIDs Avoid spicy foods, caffeine, alcohol Pharmacological Triple (Omeprazole, Amoxicillin, Clarithromycin) 7 days Quadruple (Omeprazole, Bismuth, metronidazole, tetracycline) 14 days Hepatitis SECES Ddx Alcoholic liver disease/ Cirrhosis Autoimmune Wilson, HH Hepatocellular Carcinoma Presentation Hepatomegaly, jaundice Vein dilation, acites, JVP spider nevi + easily bruising Gynecomastia + testicular hypertrophy Palmmar erythema, flubbing tremor Evaluation LFTs, FBC, U&Es, CRP autoantibodies & Ascitic tap Imaging US abdomen/portal vein doppler Management Conservative (Alcohol abstinence, optimise nutrition, low salt diet, fluid restriction) Medical Vitamin B + chlordiazepoxide Diuretics, Paracentesis Antibiotics, Steroids + albumin Lactulose Vaccination against HAV and HBV Surgical TIPSS/ transplantation Scoring system Child Pugh Score: bilirubin, PT, albumin, ascites, hepatic encephalopathy GERD NERD70%, Erosive30%, Barrett10% Presentation Heartburn, regurgitation chronic cough, chest pain hoarseness, pharyngitis Cardiovascular examination Heart failure Presentation Exertional dyspnea/Orthopnea Paroxysmal nocturnal dyspnea Fatigue, N/V, congested liver Cynosis, JVP, S3 & S4 Crackles and wheeze, RT. plural effusion periorbital purpura, Ankle edema Evaluation ECG, CXR, Echo, MRI, Biomarkers BNP Management Stage A control the risk factors Stage B ACE + BB, ICD Stage C ARN + BB + SGLT + MRA, CRT Emergency management ABC - O2, vitals, rhythm Loop Diuretic - IV furosemide Folly’s catheter Search for the cause Systolic HF (stop BB give IV inotrope and mechanical support) Diastolic HF (BB, IV fluid, vasopressin) Unknown HF (IV inotrope and IV vasopressin, ECHO) Ischemic heart disease Evaluation Clinical symptoms upper endoscopy 24 hour PH mentioning Angina chest pain, ST depression, -ve cardiac marker NSTEMI chest pain, ST depression, +ve cardiac marker STEMI chest pain, ST elevation, +ve cardiac marker Management Proton pump inhibitor H2 receptor blocker Antireflux surgery Presentation very severe pain type pressure, diffuse Radiate to the arm, neck jaw Sweat, nausea, vomiting, breathlessness, Dysphagia After swallowing? Regurgitation? esophageal dysphasia Stricture, Esophagitis, Dysmotility Evaluation ECG & Cardiac biomarkers (Troponin, CK-MB) Initiation of swallowing? Choking? Oropharyngeal dysphasia Neuromuscular disease Management Nitrates, BB, Oxygen, ACEI/ARB Life-style modification PCI Pericarditis Presentation Chest pain can be retrosternal, positional, fever, friction rub, Distant heart sounds Evaluation ECG - PR depression, T wave inversion ECHO - efusion and tamponade CXR - water-bottle Management High dose NSAID fuid removal - pericardiocentesis Endocarditis Presentation fever, tiredness, night sweats, weight loss purpura, petechial, splinter haemorrhages Osler, Janeway lesion & Roth's spots Evaluation Blood culture, CBC ESR, CRP, Urinalysis ECG, ECHO, CXR The Duke criteria Major x2 vegetations, Positive blood culture Minor x1 Intravenous, Pyrexia Management Remove the source of infection Empirical treatment subacute: amoxicillin, gentamicin acute: vancomycin, gentamicin prosthetic: vancomycin, gentamicin, rifampicin surgery: HF, Large vegetations, Abscess Valvular heart disease MS rheumatic & congenital dyspnoea, haemoptysis, Fatigue, AF loud S1 + low mid-diastolic murmur Tx digoxin + BB + Diuretic + Anticoagulation MR rheumatic & post valvotomy Dyspnoea, oedema, ascites, palpitation apical S3 + Apical pansystolic murmur/ radiates into the axilla + thrill Tx digoxin + Vasodilators + Diuretic + Anticoagulation + replacement AS AGE asymptomatic, syncope, angina Ejection systolic murmur Tx surgery if severe AR infection, trauma, root dilatation collapsing pulse, Head nodding, Femoral bruit Early diastolic murmur, heaving apex beat Tx replacement, Marfan = root replacement Palpitations History frequency, rhythm, method of termination, associated symptoms (N/V, presyncope) Evaluation EKG or Holter ECHO- size and function TEE- thrombi Exercise stress TSH & T4 levels AF Irregular RR intervals + no distinct P waves. Rate controller: BB + CCB Rhythm controller: Digoxin Unstable: synchronized cardioversion + anticoagulation Stable: rate control + anticoagulation SVT Narrow QRS, pain, fever, hypovolemia, anemia, hypoxia, PE, anxiety Unstable: cardioversion Stable: Vagal massage, IV adenosine Polymorphic VT torsade's de pointes: IV magnesium sulfate Aortic dissection Presentation Abrupt, severe, sharp chest/back pain Bilateral BP and pulses for asymmetry Diagnosis CXR, CT 1st, D-dimer, EKG/Troponin Management IV BB or verapamil/diltiazem Type A: surgery! Uncomplicated B: medical, surgery if needed Complicated B: surgery 1st then must use medical treatment after Respiratory examination Pneumonia Atypical: Legionella, Mycoplasma, Chlamydia Evaluation CURB65: confusion, Urea+19, RR+30, BP+90 CXR: lobar consolidation, interstitial infiltrates & cavitation Labs: CBC, ABG, LFT, COV19, Blood culture Ddx: CHF, PE, ILD, bronchiectasis Management: Antibiotics (Amoxicillin), O2, Antipyretics, IV fluid, Vaccines Bronchiectasis Presentation Productive Chronic cough, foul-smelling Wheezing & Crackles Dyspnea & Hemoptysis Recurrent lung infections Clubbing & Weight loss Evaluation CBC, gram stain & culture, AFB Quantitative immunoglobulin testing CF genotyping, CXR, PFT, Bronchoscopy Management Treat underlying cause Airway (Nebulized, Bronchodilators) Antibiotics & Vaccines physiotherapy & Surgery Bronchial Asthma Presentation Wheezing, Dyspnea, Cough Allergic rhinitis, Nasal polyps, dermatitis Evaluation Spirometry: ↓ FEV1/FVC <70% +ve bronchodilator response PEFR: Normal: ≥ 500 L/min CBC: eosinophilia 4% Sputum & IgE level & CXR Management Patient dedication & Vaccinations Quick-relief (rescue): SABA & LABA + ICSformoterol + Oral/ IV corticosteroids Long-term (control): Inhaled ICS, ICS & LABA, LAMA, Montelukast, Theophylline, Biologic tx COPD Emphysema Presentation Excessive smoking, dyspnea, productive cough, prolonged expiration, Pursed lip exhalation, Yellow nails, barrel chest Evaluation CXR: Hyperinflation, Flat diaphragm, Bullae PFT, ABG, a1 antitrypsin, Sputum culture Management Stop smoking, vaccine, bronchodilators, O2, rehabilitation, Bullectomy Tuberculosis Presentation Pleural effusion, dry cough, Hemoptysis, fever, night sweats, weight loss, and malaise, caseating granulomatous, Meningitis, coma, seizure, paresis, organomegaly, Spine and Hip osteomyelitis. Evaluation Protect yourself! AFB, NAAT, Mycobacterial culture, CXR Latent TB Tuberculin skin test Interferon gamma release assay Management Isoniazid*, rifampin*, pyrazinamide, ethambutol (6months) *latent Pleural Effusion Transudative (CHF, Cirrhosis, Hypoalbuminemia) Exudative (TB, Viral, PE, Malignancy) presentation Peripheral edema + Dyspnea Absent tactile fremitus & breath sounds Dullness over the chest Decreased mobility, bulging Evaluation CXR: costophrenic angle blunting Thoracentesis & fluid analysis Management Serial therapeutic thoracenteses Indwelling Pleural Catheter Pleurodesis. Pneumothorax Primary (simple): tall, thin young men. spontaneous. Secondary (complicated): underlying lung disease, life threatening Presentation cyanosis, Cough, Dyspnea, Ipsilateral pleuritic chest pain, Hyperresonance, absent tactile fremitus. Evaluation: CXR, ultrasonography, CT-Chest. Management chest-tube placement, O2 +2 cm aspirate cannula +4 cm chest drainage Dyspnea acute: hours to days chronic: + 4 to 8 weeks Presentation cough - asthma or chest infection change of the sputum - COPD Chest pain - cardiac conditions Sudden shortness of breath - PE History character, onset, duration, associations, severity, relation to exertion and any exacerbating/relieving factors. Systematic review HF, Asthma, kyphoscoliosis, anemia, anxiety Family history coronary artery disease, dilated cardiomyopathy, and sudden cardiac death Social history smoking, alcohol use and illicit drug use Evaluation CXR, D-dimer, ECG, TSH, BNP, Spirometry Clinical examination General appearance and vital sign Extremities & Neck & Abdomen Cardiac and pulmonary disease Management Supplemental oxygen Pulmonary rehabilitation Cough History Onset & Duration Dry or productive Characteristic Exacerbating & relieving Associated symptoms viral URI - Rhinorrhea & obstruction acute lung infection - Fever, malaise, purulent sputum upper airway cough syndrome - fluid dripping into throat, clear throat Red flag symptoms Hemoptysis Weight loss Night sweating Hoarseness Review of systems MSK: Rheumatoid, Scleroderma GERD Family history Atopy: asthma, eczema Lung: cancer, TB, fibrosis Drug history ACE, ARB, NSAID, BB, Methotrexate, Amiodarone Social history Smoking, drugs, asbestos, Pets Physical examination Vitals: RR, Temp, Pulse, O2 Head: nostrils, mouth, tonsils, pharynx, ears (secretions, redness, polyp) Lung: wheezes, crepitation Extremities: clubbing, staining, LL edema. Evaluation spirometry, CXR, CT, PFT BNP, ECG, ECHO Endoscopy, 24H pH, barium swallow Hemoptysis History Onset & Duration, severity, color, Character, amount, fever, chills, sputum, weight loss, anticoagulants, smoking, other sites bleeding, congenital diseases, Cough, dyspnea Physical examination Respiratory (tachypnea, cynosis, clubbing) CV (conjunctival/ splinter hemorrhage) Hematology (DIC, telangiectasia, bruising) Rheumatology examination Evaluation Confirmation of hemoptysis Electrocardiogram Sputum microbiology CXR & Bronchoscopy CBC, PTT, D dimer Presentation Mono arthritis (knee), abrupt pain, warmth, swelling, fever, sweating Management Oxygen supplementation IV fluid resuscitation Fresh frozen plasma Plt transfusions -50 Desmopressin & vasoconstrictor Surgery - trauma, AV fistula Empirical antibioticse Bedrest on the same side of bleeding control coughing Pulmonary embolism Wells criteria Presentation Dyspnea, pleuritic pain, Cough, Syncope, Hemoptysis,DVT, Tachypnea & hypoxemia, crackels, ronchi, decrease breathing sounds, Rt HF Evaluation Stable: d-dimer then CTPA Unstable: TTE the CTPA ECG: Sinus tachycardia, S1Q3T3 Wells Point Score (+4) DVT, Other Dx = 3 Heart rate +100, immobilization = 1.5 Past DVT, Hemoptysis, cancer = 1 CXR: pleural effusion, Hampton hump, Westermark V-Q scan for pregnants Management Oxygen supplementation Thrombolysis & embolectomy Anticoagulation UFH (3 months) LMWH for Pregnancy IVC filter- recurrence Stable: SC Antico. LMWH & Fondaparinux. Unstable: O2, systemic Anticoagulation TPA, embolectomy Acute arthritis Bacteria/inflammation Evaluation Arthrocentesis +50k ESR and CRP Blood culture Conventional radiograph Management Empirical antibiotic Joint drainage abscess IV antibiotic (S. aurse vancomycin/ N. Gono Ceftriaxone) GOUT 1st MTP of great toe - podagra Acute Management: NSAID, Colchicine, Corticosteroid, Anakinra Chronic management decrease meat and seafood, Allopurinol, Febuxostat, IV pegloticase Pseudogout calcium pyrophosphate (3H’s): Hemochromatosis, Hyperparathyroidism, Hypomagnesemia Chondrocalcinosis/2nd and 3rd MC Chroinc rheumatoid arthritis Presentation Insidious/gradual in onset, Multi symmetrical joint involvement, pain, stiffness, swelling, wormth +30 minutes, relieved by movement Examination 1. Joints — MCP, PIP, MIP 2. Deformities – Swan neck, ulnar deviation, boutonnière, muscle wasting 3. Synovial proliferation – carpal tunnel syndrome, pouplotial burst, neck subluxation 4. Systemic — fever, fatigue, weight loss 5. Extra articular – subcutaneous nodules, vasculitis, endocarditis, valve diseases, Sicca, Scaleralitis Evaluation 1. Joint involvement (no. + size) 2. Serology (RF/ACPA) 3. Inflammatory markers (CRP/ESR) 4. Duration (+6 months) 5. Radiology & aspiration Management Referral to rheumatologist & physiotherapy Symptoms — NSAID Slow progression — steroids Treatment — DMARD (Methotrexate, Sulfasalazine, Leflunomide) & Hydroxychloroquine Ankylosing spondylitis Presentation +40 old man, Sacroiliitis, dactylics, Low back pain in night, morning stiffness, Heel pain, IBD Evaluation Xray: bamboo spine Management NSAID, Steroids, Anti TF Stop smoking + Education Psoriatic arthrtis Presentation Psoriasis, arthritis, nail biting Evaluation CASPER 1. current episodes +2 2. Family / previous Hx 3. Dactylitis 4. -ev RF 5. New bone formation 6. Nail biting Management NSAID, Methotrexate, Leflunamide Reactive arthritis Presentation Post infection, urethritis, conjunctivitis, dysuria and diarrhea, ketoderma blennorrhagica Management NSAID, steroids + time Connective tissue diseases SLE Presentation Fever, alopecia, oral ulcers, Mala rash, delirium, psychosis, pleural effusion, leukopenia, thrombocytopenia, arthritis Evaluation ANA, ds-DNA, Anti-Smith Low C3, C4 lupus anticoagulan, anti-cardiolipin, β-2glycoprotein I Management Organ involvement: cyclophosphamide, Mycophenolate mofetil, Rituximab No organ involvement: hydroxychloroquine, low-dose steroids, azathioprine, methotrexate Sjögren’s syndrome Presentation Sicca (dry eyes and mouth) fatigue, fever Evaluation Serology: +ve SSA/Ro or SSB/La Biopsy: lymphocytic Keratoconjunctivitis Management Eye: artificial tears, steroid cyclosporine drops Oral: sugar free gum, salvia substitute, hydration, cevimeline or pilocarpine Scleroderma Presentation Raynaud, Synovitis, Myositis, Pulmonary HTN, tight and thickened skin, hand edema Evaluation Anti-U1-RNP - overlap anti-Scl-70 - diffuse/fibrosis anticentromere - limited/HTN BUN/Cr, PFTs, CT, TTE, BP Management Symptomatic Pulmonary fibrosis - cyclophosphamide PAH - vasodilator Renal - ACE Skin - steroids, methotrexate