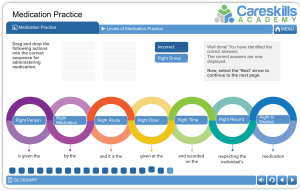
Pharmacology Final Study Guide ● What to worry about when administering medications to older adults? ○ ○ ● Adverse drug events ■ Adverse drug reactions ■ Medication errors ■ Therapeutic failures ■ Adverse drug withdrawal events ■ Overdoses Adherence ■ Patient may not fully understand drug regimen ■ Non Adherence may cause underdosing of overdosing ■ Medication education extremely important ■ Lack of prescriptions drug coverage What does the FDA do? ○ US Food and Drug Administration ■ Established Critical Path Initiative, a national strategy “to drive innovation in the scientific processes through which medical products are developed, evaluated, and manufactured.” ○ ■ improving the prevention, diagnosis, and treatment of rare and neglected disorders ■ Standardized OTC labeling Good Clinical Practice (GCP) Consolidated Guideline ■ International ethical and scientific quality standard for designing, conducting, monitoring, auditing, recording, analyzing, and reporting clinical research ● ■ Provide consumers with information ■ Described benefits and risks with OTC drug Understand how to properly give an intradermal administration of a medication. ○ Locations are chosen so an inflammatory reaction can be observed. Must be lightly pigmented, free of lesions, hairless, such as ventral mid forearm, clavicular area of the chest, or scapular area of back ○ Needle: 25 to 27 gauge, ¼ to ½ inch long, tuberculin syringe ○ Syringe: 1mL ○ Administration ■ Perform hand hygiene and gloves ■ Cleanse area with a circular motion using aseptic technique ■ Hold the skin taut. ■ Insert the needle, bevel up, at a 10- to 15-degree angle ■ Inject the medication slowly to form a bleb (or wheal). A small amount is injected so the volume will not interfere with bleb formation or cause a systemic reaction. If the bleb does not appear, the needle has been injected subcutaneously. ■ Remove the needle slowly, and do not recap it. ■ Do not massage the area, and instruct the patient not to do so. ■ Mark the area with a pen, and ask the patient not to wash it off until the response can be “read” by an HCP. ■ It is not recommended to put an adhesive bandage over the testing site because it can alter the results of the test. ■ Assess for allergic reaction in 24 to 72 hours; measure the diameter of any local reaction. For tuberculin testing, measure only the indurated area; do not include the area of erythema in the measurement ● Know your 6 rights of administration and how to best identify a patient. ○ ○ ○ Right Patient ■ Verify patient with 2 forms of identification ■ Compare patients stayed name and birthdate w/ patient's ID band and MAR ■ Scan patients barcode on their ID band ■ Check color coding on patients ID band ■ Verify patient's name with family member if present ■ Check for “name-alert” sticker when 2 patients have save name Right Drug ■ Scan medication label ■ Check that order is prescribed by licensed health care provider ■ Read drug label three time ■ Be familiar with patients health record, allergies, lab result, and vital signs ■ Know why the patients is receiving medication and if correct for patients diagnosis ■ Check dose calculations ■ Know beginning and ending date of medication Right Dose ■ Verify dosage calculation ■ Verify that drug is safe for patients ■ Unit dose method, in which drugs are individually wrapped and labeled for single-dose use for each patient ○ ○ ○ Right Time ■ Use health care agency policy ■ Use of military time reduced errors ■ Drug affected by food are given I h ac or I h pc ■ Give food with drugs that irritate the stomach ■ Check for scheduled procedures ■ Check expiration date ■ Administer antibiotics at even intervals ■ Hold antihypertensives prior to dialysis if ordered Right Route ■ Necessary for adequate absorption ■ Assess patients ability to swallow oral medication ■ Do not crush of mix medications without validation or consultation ■ Offer patients water but not juice (iron may be taken with orange juice ) ■ Use aseptic technique Right Documentation ■ Record drug administration immediately ● ■ Record drug name, dose, route, time, date, nurses signature or initials according to policy ■ Document patient's response to drug especially analgesics, sedatives, and antimetics Know you IV fluids and the different types. When to use and why. ○ Types of Intravenous Solutions: ■ ■ Crystalloids ● Used for short-term maintenance therapy ● Treat dehydration and electrolyte imbalance Major classifications: ● Isotonic: solutions have the same approximate osmolality as ECF or plasma. Because of the osmotic equilibrium, water does not enter or leave the cell; therefore there is no effect on red blood cells (RBCs). Primarily used for hydration and to expand ECF volume, because the fluid remains in the intravascular space. ● Hypotonic: solutions exert less osmotic pressure than ECF, which allows water to move into the cell. IV infusions of hypotonic solutions result in an increased solute concentration in the intravascular space, causing fluid to move into the intracellular and interstitial spaces. Excessive infusion of hypotonic solutions may cause hemolysis, decreased blood pressure, and decreased IVF volume. ● Hypertonic: solutions exert greater osmotic pressure than ECF, resulting in a higher solute concentration than the serum. When administered, hypertonic IVF fluids pull water from the interstitial space to the ECF via osmosis and cause cell shrinkage. Patients receiving hypertonic solutions must be monitored carefully for signs of circulatory overload (because of the increase in ECF volume). ○ Examples: Dextrose 5 in water (D5W), Normal saline solution (0.9% NSS), Lactated Ringers ■ Colloids ● Plasma expanders ● Contain protein ● Because of their size, the particles are unable to pass through the semipermeable membranes of the capillary walls and stay within the intravascular compartment; thus colloids are also known as plasma expanders. ● They act by increasing the colloid oncotic pressure and pulling fluids from the interstitial space into the plasma, increasing blood volume. ● ■ ● Examples: Dextran 75, Albumin 5% Blood and Blood products ● Whole blood ● Packed RBC ● Plasma ● Platelets ● Cryoprecipitate ● Max rate of infusion is 4 hours per unit Know how to give eye drops, suppositories, and enteral meds ○ Administering Eye Drops ■ Gently pull down on the skin below the eye to expose the conjunctival sac ■ Apply drops to the middle third of the sac, and apply gentle pressure over the lacrimal duct after administration ○ Suppositories Rectal ■ A suppository is a useful route in babies, in uncooperative patients and in cases of vomiting or certain digestive disorders ■ The numerous small capillaries in the rectal area promote medication absorption ■ During insertion, place the suppository past the internal anal sphincter; otherwise, the suppository will be expelled before it can dissolve and absorb into the mucosa. ■ ○ Some suppositories tend to soften at room temperature Suppositories Vaginal ■ Available as suppositories, foams, jellies, or creams ■ They are not individually packaged in foil wrappers and are sometimes stored in refrigerator to prevent the solid, oval shaped suppositories from melting ■ Foams, jellies, creams and suppositories are generally inserted into the vagina with an applicator supplied with the medication ■ Gloves should be worn and patients should be in lithotomy position ■ Advise patients to remain lying for a time sufficient to allow medication absorption; time vary depending on the medication ■ After insertion, provide the patient with a sanitary pad. If the patient is able, they may want to personally insert the vaginal drug. ○ Enteral Medication ■ Oral medications absorbed by the gastrointestinal tract, mainly from the small intestine ■ When administering nonliquid drugs through an enteral tube, the nurse should always ensure that the drug is crushable ● ■ dissolve in water and that it can be absorbed through the enteral route. ■ Never mix medications with feeding formulas Know the definitions of Pharmacodynamics and Pharmacogenetics. ○ Pharmacodynamics ■ is the study of the effects of drugs on the body. Drugs act within the body to mimic the actions of the body’s own chemical messengers. ○ Pharmacogenetics ■ Pharmacogenetics is the study of how a patient’s genome affects his or her response to medications ● Know the Z-Track injection technique and why and when it is used. ○ Recommended when administering IM injections to help minimize local skin irritation by sealing the medication in the muscle tissue ○ Ventrogluteal site preferred using aseptic technique, draw up medication, Holding the skin taut, inject the needle at a 90-degree angle deep into the muscle, and if there is no blood return on aspiration, slowly inject the medication. Allow the needle to remain inserted for 10 seconds for the medication to disperse evenly. ○ ● Medication administration safety/ tip ● Understand topical medication administration. ○ Frequently applied to the skin by painting or spreading the medication over an area and applying a moist dressing or leaving the area exposed to air. ○ ● Can be applied with a glove, tongue blade, cotton-tipped applicator, never without gloves. Advantages to IV administration. ○ Direct ○ Immediate action/ Therapeutic effect ○ Patients cannot tolerate drugs/ fluids orally ○ Some drugs cannot be absorbed by any other route ○ Pain and irritation is avoided compared to some substances given SC/IM ○ Drug is delivered immediately upon the completion of a response requirement and since delivery is into a vein, there is a rapid onset of drug effects. ■ ○ Such immediate results in rapid acquisition and strong maintenance of behavior Administering medication intravenously eliminated the princess of drug absorption and breakdown by directly depositing it into the blood. ● Know what hyponatremia is and how to treat it with IV fluids. ○ Hyponatremia: caused by a loss of sodium-containing fluids, deficient intake, or water gain. ■ ○ Less than 135 mEq/L Signs and Symptoms ■ Muscle weakness ■ Coma ■ Decreased deep tendon ■ Abdominal cramps reflexes ■ Nausea ■ Headaches ■ Vomiting ■ Lethargy ■ Pale skin ■ Confusion ■ Dry mucous membranes. ■ Seizures ■ For a serum sodium level between 125 and 135 mEq/L, IV normal saline (0.9% sodium chloride) may increase sodium content in vascular fluid. For a serum sodium level below 120 mEq/L, a hypertonic 3% or 5% saline solution may be necessary. ● Hypokalemia- symptoms, causes and treatment ○ Hypokalemia, or potassium deficit, is generally defined as a serum potassium concentration of less than 3.5 mEq/L ○ ○ ● Signs and Symptoms ■ Quadricep weakness ■ Anoreixa ■ Fatigue ■ Nausea ■ Muscle weakness ■ Vomiting Severe Signs ■ Paresthesia ■ Rhabdomyloysis ■ Leg cramps ■ Myoglobinuria ■ Decreased bowel motility ■ Atrial and Ventricular ■ Paralytic ileus ■ Confusion Dysrhythmias ■ Cardiac arrest Know nurses’ rights in medication administration. ○ Bill of Rights for nurses containing seven premises concerning workplace expectations and environments that nurses from across the United States recognize as necessary for safe nursing practice. ○ The Bill of Rights supports nurses in workplace situations and includes issues such as unsafe staffing, mandatory overtime, and health and safety issues in the workplace. These issues are essential to meet the responsibilities of patient care, including safe drug administration and the responsibility nurses have to themselves ● Know what enteric coated, extended release, or sustained release capsules are. ○ Enteric coated: drugs resist disintegration in the gastric acid of the stomach, so disintegration does not occur until the drug reaches the alkaline environment of the small intestine ○ Extended release: Medications that last longer in the body ○ Sustained release capsules: Drugs that release small medication into a person’s system over a long period of time ● Transdermal medications considerations ○ Transdermal medication is stored in a patch placed on the skin and is absorbed through the skin to produce a systemic effect. ○ A patch may be left in place for as little as 12 hours or as long as 7 days depending on the drug. ○ Transdermal drugs provide more consistent blood levels than oral and injectable forms, and they avoid GI absorption problems associated with oral products. ○ To prevent skin breakdown, transdermal patches should be rotated to different sites and should not be reapplied over the exact same area every time. Additionally, the area should be thoroughly cleansed before administration of a new transdermal patch. ○ ● Never cut patch in half and don’t apply tape too tightly Know what a gastrostomy tube is and how to properly use one to administer meds. ○ Gastrostomy tube: ■ AKA the percutaneous endoscopic gastrostomy (PEG) tube, and the jejunostomy (J) tube ■ Placed surgically, endoscopically, or radiologically. ● With the PEG tube, the patient must have an intact GI system. ■ Usually, the doctor orders intravenous (IV) antibiotics to decrease the risk of infection. ■ Always check for proper placement and gastric residual before administering drugs ■ Place the patient in high fowler position or elevate the head of the bed at least 30 degrees ■ Make sure drug is crushable- add H2) to dilute ■ Remove the plunger from the syringe and attach it to the feeding tube, pour liquid medication into the syringe, release the clamp and allow the medication to flow in properly by gravity. A gastrostomy tube is introduced through a temporary or permanent opening on the abdominal wall (stoma) into the stomach. ● Understand what the assessment, planning, implementation, and evaluation stages are of the nursing process and how they pertain to drug administration. ○ Assessment ■ Determine patient’s level of consciousess, risk for aspiration, and abaiity to take medications ○ Planning ■ ○ Implementation ■ ○ ● Identify strategies to promote adherence to drug regimen Execute drugs Evaluation Know how to properly teach your patient about self-administering a medication i.e. inhalers, sublingual, etc. ○ Metered Inhaler ■ Patient education insert med into plastic holder ■ If space used-attach inhaler to end -Shake ■ Sitting position, then practice breath ■ Instruct the patient to take slow, deep breath through the mouth and during inspiration, to push the top of the medication canister once ■ Have patient hold the breath for 10 seconds and then exhale slowly through pursed lips ■ If a second dose is required, wait 1-2 minutes and repeat the procedure by the first shaking the canister in the plastic holder with the cap on (5 for steroid) ● ● ● ● Know all the essential components that must be present on a physician’s order for a medication. ○ Patient’s Full name, Date, Time ○ Drug Name ○ Dosage ○ Route of Administration ○ Time and Frequency of Administration ○ Signature and licensure of physician Know the difference between enteral and parenteral route of administration. ○ Enteral Feeding tube ○ Parenteral ■ 1. Intradermal ■ 2. Subcutaneous (subcut or SQ) ■ 3. Intramuscular (IM) ■ 4. Intravenous What is a sublingual medication? How do you administer or educate your patient? ○ Sublingual Medication is given under the tongue or between the cheek and gum (buccal) ○ Administer by remaining in place until fully absorbed with no food or fluids Nursing considerations regarding diversity, culture and religious preferences regarding medication administration ○ ● Patient’s choice should be honored whenever possible General herbal preparations precautions and patient education ○ ○ Dietary Health and Education Act (DSHEA) 1. Name of the supplement 2. Amount of the supplement (net quantity) 3. Nutrition labeling 4. Ingredient list 5. Name and place of the manufacturer, packer, or distributor ● Opioid withdrawal symptoms ○ Nausea ○ Hyperthermia ○ Vomiting ○ Hypertension ○ Abdominal Cramps ○ Restlessness