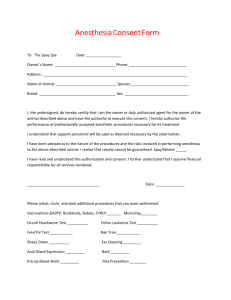
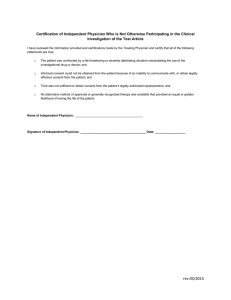
Patient Bill of Rights ◦ Section B #9- A patient shall receive information necessary to give informed consent prior to the start of any nonemergency procedure or treatment or both the reasons for it, the reasonably foreseeable risks and benefits involved and the alternative for care or treatment if any as a reasonable practitioner under similar circumstance would disclose. Documented evidence of such informed consent shall be included in the patients medical record. It is the policy of Strong Memorial Hospital that each patient or the patient’s authorized representative will be provided with the information they need to enable them to make informed treatment decisions. Informed consent may be verbal or in writing, but it must be documented in writing prior to performance of all invasive medical and surgical procedures, transfusion of blood or cellular elements of blood, and/or use of tissue in a procedure, except in cases of emergency when informed consent cannot be reasonably obtained. The discussion with the patient or the patient’s authorized representative, and their consent to the treatment or procedure, must be documented in the patient’s medical record. Was first referenced in World War II medical experimentation Introduced into American law in the 1950’s ◦ Case: Salgo V Leland Stanford Jr. Univ. Bd. of Trustees, 317 P.2d 170, 181(Cal. Dist. Ct App 1957) Emerged from the legal idea that physicians were from now on obligated to share decision making authority with their patient, which was contrary to pre-existing medical practices. Webster Dictionary- ◦ Consent to surgery by a patient or to participation in a medical experiment by a subject after achieving an understanding of what is involved (No where does it mention the practice of anesthesia or any other non-surgical interventions) American Medical Association: ◦ It is a process of communication between a patient and physician that results in the patient's authorization or agreement to undergo a specific medical intervention Allow for a patient to participate in his/her own health care decisions Involves ethical obligations Implies legal ramifications Having or showing knowledge of a particular subject or situation. A decision or judgment based on an understanding of the facts of the situation. Open communication between patient and physician ◦ Specifically relating to medical diagnosis, interventions, alternatives to intervention, and risks of intervention Explanation of risks and benefits ◦ Of both undergoing and not undergoing the procedure Opportunity for questions Judgment regarding comprehension Anxious adult female, presents for lumpectomy after recently being diagnosed with breast cancer. As you begin your discussion of the anesthetic plan she begins to cry and says, “ Doc, You telling me the risks is going to make me feel worse. Please can we skip this conversation and go to the OR. I will be fine.” Is this patient informed and does it matter? Reasonable physician standard: ◦ What would a typical physician say about this intervention? Reasonable patient standard: ◦ What would the average patient need to know in order to be an informed participant in the decision? Subjective standard: ◦ What would this patient need to know and understand in order to make an informed decision? To give assent or approval Permission for something to happen or agreement to do something Competency to make decision for ones self Voluntariness, free of coercion Freedom to decline ? Documentation Can be signed theoretically by any physician, who partakes in that patient care. ◦ Resident or Attending from other consulting services can sign it In terms of anesthesia, there are only a couple of sentences, informing the patient about there anesthesia risk ◦ “I consent to the administration of local, regional or general anesthesia and/or sedation as deemed most appropriate for the procedure to be performed.( The list of possible anesthesia providers all of whom are credentialed to provide anesthesia at this hospital)” The UMRC Anesthesiology Informed Consent includes: ◦ Section for Risks from Anesthesia (You should check only the ones you actually talk about) ◦ Section for who the Anesthetic Plan and Risk discussion was with (ex: patient, spouse, father, mother, etc.) ◦ Section for who the Blood Products discussed was with ◦ Section for what medical provider your plan was discussed with( ex CRNA, Fellow, Surgeon, Anesthesiology Attending etc.) It does not require a patient signature. Practice a script ◦ Try to have a frame work of what you want to say to the patient prior to your conversation Don’t make it to scripted ◦ Try to not let the patient become a “drop down menu”, if you can document something specific to that patient in your consent form: (Ex I spoke to Mrs. X and her sister who is visiting from Y) Document Document Document!! Please refer back the Salgo V Leland Stanford Jr. Univ. Bd. of Trustees, 317 P.2d 170, 181(Cal. Dist. Ct App 1957) Would you consider the patient informed? Do believe he gave proper consent?