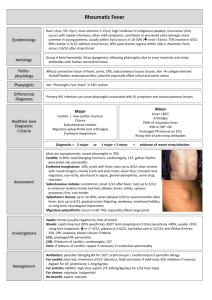
Pedi Acquired Cardiovascular Study Guide Rheumatic Fever *delayed sequela of group A streptococcal pharyngeal infection. occurs more often in school-age children between 5 and 15 years of age in areas where streptococcal pharyngitis is more prevalent, especially during the colder months. It usually develops 2 to 4 weeks after the initial streptococcal infection. child develops an antibody response to surface proteins of the bacteria. The antibodies then cross-react with antigens in cardiac muscle and neuronal and synovial tissues, causing carditis, arthritis, and chorea (involuntary random, jerking movements). ARF affects the joints, central nervous system, skin, and subcutaneous tissue and causes chronic, progressive damage to the heart and valves. Rheumatic Heart Disease (RHD) is the most common complication of RF, that damages the heart valves. Assessment *Jones Criteria: Diagnosis of acute rheumatic fever requires the presence of either two major criteria or one major plus two minor criteria. Major Criteria Carditis Migratory polyarthritis Subcutaneous nodules (occur in crops over bony prominences) Erythema marginatum (rash on trunk and proximal extremities) Sydenham chorea – St. Vitus Dance (5th manifestation) o CNS involvement o Sudden, aimless movements of the extremities o Involuntary facial grimaces o Speech disturbances o Emotional lability o Muscle weakness Minor Criteria Polyarthralgia Elevated erythrocyte sedimentation rate or C-reactive protein Prolonged PR interval (unless carditis is a major criterion) recent medical history for risk factors, such as documented streptococcal infection or sore throat within the past 2 to 3 weeks, or for history of ARF. Auscultate the heart, noting a murmur. Throat culture will provide definitive diagnosis of current streptococcal infection, while streptococcal antibody tests may yield evidence of recent infection. Echocardiogram is required to determine if carditis is present. Management managing inflammation and fever, eradicating the bacteria, preventing permanent heart damage, and preventing recurrences. *A full 10-day course of penicillin therapy (or equivalent) is used along with corticosteroids and nonsteroidal anti-inflammatory drugs. Children without valvular disease will receive continued prophylaxis with monthly intramuscular injections of penicillin G benzathine or daily oral doses of penicillin or erythromycin (if allergic to penicillin’s) following the initial illness to prevent a new streptococcal infection and recurrent ARF. Prophylaxis is continued until adulthood Some children may require a neuroleptic agent such as haloperidol (Haldol) for management of chorea. Administer corticosteroids or nonsteroidal anti-inflammatory agents for control of joint pain and swelling. Kawasaki Disease *acute systemic vasculitis occurring mostly in children 6 months to *5 years of age. It is the leading cause of acquired heart disease among children and occurs more often in the winter and summer It is a self-limited syndrome but can cause cardiovascular complications such as coronary artery aneurysm and cardiomyopathy Pathophysiology etiology is still unknown appears to be an autoimmune response mediated by cytokine-induced endothelial cell surface antigens that leads to vasculitis in the medium size arteries, including the coronary arteries Generalized systemic vasculitis occurs in the blood vessels throughout the body due to the inflammation and edema and can lead to coronary dilation or aneurysm *Assessment Three Phases: Acute - sudden high fever, unresponsive to antipyretics and antibiotics Subacute - end of fever through end of all KD clinical signs Convalescent - clinical signs resolved, but laboratory values not returned to normal; completed with normal values (6-8 weeks) Lab and Diagnostic Testing CBC count may reveal mild to moderate anemia, an elevated white blood cell count during the acute phase, and significant thrombocytosis in the later phase The erythrocyte sedimentation rate (ESR) and the C-reactive protein (CRP) level are elevated. Echocardiogram is performed as soon as possible after the diagnosis is confirmed to provide a baseline of a healthy heart or to evaluate for coronary artery involvement Management reducing inflammation in the walls of the coronary arteries and preventing coronary thrombosis. Chronic management of children developing aneurysms during the initial phase is directed toward preventing myocardial ischemia. *In the acute phase, high-dose aspirin (80-100 mg/kg/day) in four divided doses daily for fever *single infusion of intravenous immunoglobulin (IVIG) Administer intravenous and oral fluids as ordered, evaluating intake and output carefully. *Assess frequently for signs of developing heart failure such as tachycardia, gallop, decreased urine output, or respiratory distress Provide acetaminophen for fever management and apply cool cloths as tolerated. Keep the environment quiet and cluster nursing care activities to decrease stimulation Apply petrolatum jelly or another lubricating ointment to the lips. Encourage the older child to suck on ice chips; the younger child may suck on a cool, moist washcloth. Popsicles are also soothing. Provide comfortable positioning, particularly if the child has joint pain or arthritis. Teach parents to continue to monitor the child’s temperature after discharge until the child has been afebrile for several days. Children with prolonged or recurrent fever may require a second dose of IVIG. Inform parents that irritability may last for up to 2 months after initial diagnosis It is important to avoid nonsteroidal anti-inflammatory agents while aspirin therapy is ongoing *Avoid measles and varicella vaccination for 11 months after high-dose IVIG administration