Coronary Artery Disease & Acute Coronary Syndrome Overview
advertisement

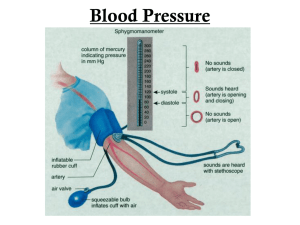
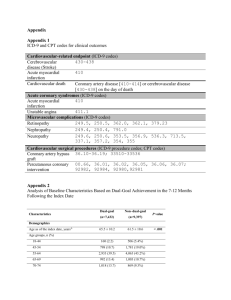
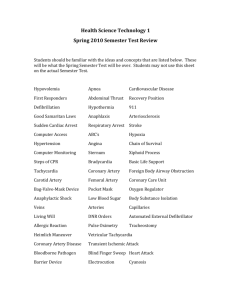
Coronary Artery Disease & Acute Coronary Syndrome ST Segment depression= Ischemia T wave inversion = Ischemia Coronary Artery Disease • • An abnormal condition that may affect the heart’s arteries and produce various pathological effects, especially reduction in flow of oxygen and nutrients to the myocardium Atherosclerosis is a major cause of CAD o Begins as soft deposits of fat that harden with age o Referred to as “hardening of arteries” o Can occur in any artery in the body o Atheromas (fatty deposits): Preference for the coronary arteries A, Damaged endothelium. B, Diagram of fatty streak and lipid core formation. C, Diagram of fibrous plaque. Raised plaques are visible: Some are yellow, others are white. D, Diagram of complicated lesion: Thrombus is red, collagen is blue. Plaque is complicated by red thrombus deposition. Vessel Occlusion with Collateral Circulation A, Open, functioning coronary artery. B, Partial coronary artery closure with collateral circulation being established. C, Total coronary artery occlusion with collateral circulation bypassing the occlusion to supply blood to the myocardium. Risk Factors for CAD Nonmodifiable Risk Factors Modifiable Risk Factors - Serum lipids (Cholesterol greater - Increasing age - Gender: Men greater than than 5.0 mmol/L or a fasting women until 65 years of triglyceride level greater than 3.7 age mmol/L) - *Hypertension (a BP > 140/90 mm Hg - Ethnicity: whites’ greater risk than blacks or >130/80 mm Hg if the patient has - Family history of heart diabetes or chronic kidney disease) - Diabetes disease - Tobacco use (2-6x higher) - Genetic predisposition - Physical inactivity - Obesity [(BMI) of >30 kg/m2 and a waist circumference ≥102 cm (40 inches) for men and ≥88 cm (35 inches) for women] Serum Lipids • Healthy serum lipid panel includes: o ↓ Total cholesterol o ↓ LDL o ↑ HDL o ↓ Triglycerides Improving Serum Lipids • Total cholesterol and LDL o ↓ Total fat intake and saturated fats • HDL o ↑ Physical activity and exercise • Triglycerides o ↓ or eliminate alcohol and simple sugars Management of CAD: Lipid-lowering drug therapy • Include drug classes that: • o Restrict lipoprotein production: Ex. Statins, niacin o Increase lipoprotein removal: Ex. Bile acid sequestrants o Decrease Cholesterol absorption: Ex. Ezetimibe (Ezetrol) Antiplatelet therapy o Low dose Aspirin or Clopidogrel (Plavix) Chronic Stable Angina • Pain o o o usually lasts 3-5 mins Subsides when the precipitating factor is relieved Pain at rest is unusual ECG reveals ST-segment depression and/or T-wave inversion Location of Pain During Angina & MI • • Although most of the pain experienced by people with angina appears substernally, the sensation may occur in the neck or may radiate to various locations, including the jaw and shoulders, and down the arms. Often people will complain of pain between the shoulder blades and will dismiss it as not being heart related. Chronic Stable Angina Management (ONAM: Oxygen, Nitrates, Aspirin, Morphine) • Acute interventions for anginal attack o Have client rest or sit immediately o Administer Oxygen • • o Assess vitals, pulse oximetry o 12-lead ECG o Prompt pain relief with a nitrate first followed by an opioid analgesic, if needed o Auscultation of heart sounds Ask the patient to describe the pain and to rate it on a scale of 0 to 10 before and after treatment to evaluate the effectiveness of the interventions. Diagnostic Studies o Health history/physical examination o Laboratory studies o 12-lead ECH o Chest x-ray o Echocardiogram o Exercise stress test o Cardia catheterization/coronary angiography (Diagnostic) o Coronary revascularization: percutaneous coronary intervention (PCI) Balloon angioplasty Stent Acute Coronary Syndrome (ACS) • When ischemia is prolonged and is not immediately reversible, acute coronary syndrome (ACS) develops. Clinical Manifestations of ACS • Unstable angina o Changes in usual pattern o New in onset o Occurs at rest o Has a worsening pattern • UA is unpredictable and represents a medical emergency Unstable Angina & MI Diagnostic Studies • Detailed health history and physical • 12-lead ECG: changes in QRS complex, ST segment elevation • Serum cardiac markers • Coronary angiography • Others: exercise stress testing, echocardiogram Elevated ST segment during an MI is referred to as an ST-segment elevation MI (STEMI). Serum Cardiac Markers After MI • • • CK-MB begins to rise about 6 hours after symptoms onset, peaks in about 18 hours, and returns to baseline within 24-36 hours after MI Troponin is detectable within hours (average 4-6hours), peaks at 1024 hours, and can be detected for up to 10-14 days Myoglobin begins to rise within 2 hours and peaks in 3-15 hours Serum Cardiac Marker After MI • Troponin- cardiac-specific o Detectable within one hour of myocardial injury, high specificity at 3 to 6 hours, peak at 24 to 48 hours and return to baseline over 5 to 14 days • CK-MB- cardiac-specific o Levels rise 4 to 6 hours after symptoms onset, peak in 18 to 24 hours, and return to baseline within 3 days after MI • Myoglobin- cardiac and skeletal muscle specific o Rise within 30 to 60 min after cardiac injury but return to baseline within 24 hours of an MI Acute Coronary Syndrome • Result: o Partial occlusion of coronary artery: UA or NSTEMI o Total occlusion of coronary artery: STEMI Myocardial Infarction (MI) • • • Result of sustained ischemia (>20mins), causing irreversible myocardial cell death (necrosis) Necrosis of entire thickness of myocardium takes 4-6 hours Infarctions are usually describing according to the location of damage (ex. Anterior, inferior, lateral, posterior wall infarction) Myocardial Infarction from Occlusion • Occlusion of the left anterior descending coronary artery, resulting in a myocardial infarction. • Termed the ‘widow maker’ MI because it affects the left ventricle which is responsible for pumping the blood into the systemic circulation. Acute myocardial infarction in the posterolateral wall of the left ventricle. This is demonstrated by the absence of staining in the areas of necrosis (white arrow). Note the scarring from a previous anterior wall myocardial infarction (black arrow). Full-Thickness MI • Myocardial infarction involving the full thickness of the left ventricular wall. Myocardial Infarction • The degree of altered function depends on the area of the heart involved and the size of the infarct • Contractile function of the heart is disrupted in areas of myocardial necrosis • Most Mis involve the left ventricle (LV) • The severity of an MI is determined by the location, if it is a partial or total occlusion (NSTEMI or STEMI) and how many layers of the myocardium is damaged. • Pain o Total occlusion anerobic metabolism and lactic acid accumulation severe, immobilizing chest pain not relieved by rest, position change, or nitrate administration o Described as heaviness, constriction, tightness, burning, pressure, or crushing o Common locations: substernal, retrosternal, or epigastric areas; pain may radiate to neck, jaw, arms • Stimulation of Sympathetic NS results in o Release of glycogen o Diaphoresis o Vasocontraction of peripheral blood vessels o Skin: ashen, clammy, and/or cool to touch • Cardiovascular o Initially, ↑ HR and BP, then ↓ BP (secondary to ↓ in CO) o Crackles o Jugular venous distension • • o Abnormal heart sounds: S3 or S4 or New murmur Nausea and vomiting o Can result from reflex stimulation of the vomiting center by severe pain Fever o Systemic manifestation of the inflammatory process caused by cell death Acute Coronary Syndrome Collaborative Care • Emergency management o Initial interventions (ONAM) Establish an IV, oxygen, sublingual NTG, Aspirin, Morphine sulphate o Ongoing monitoring of VS, lung and heart sounds • Emergency PCI (ideally within 90 mins) o PCI= percutaneous coronary intervention o Treatment of choice for confirmed MI o Balloon angioplasty + drug-eluting stents • Fibrinolytic therapy (within 6 hours) o IV Alteplase/Activas recombinant or tissue plasminogen activator (t-PA) o Best marker of reperfusion: return of ST segment to baseline o Rescue PCI if thrombolysis fails o Major Complication: BLEEDING • Coronary surgical revascularization o Failed medical management o Presence of left main coronary artery or three-vessel disease o Not a candidate for PCI (Ex. Lesions are long or difficult to acess) o Failed PCI with. Ongoing chest pain o History of diabetes o Coronary revascularization with CABG surgery is recommended for these patients o Coronary artery bypass graft (CABG) surgery Requires sternotomy and cardiopulmonary bypass (CPB) Uses arteries and veins for grafts CABG Surgery The distal end of the left internal mammary artery is grafted below the area of blockage in the left anterior descending artery. The proximal end of the saphenous vein is grafted to the aorta, and the distal end is grafted below the area of blockage in the right coronary artery. Myocardial Infarction Healing Process • Within 24 hours, leukocytes infiltrate the area of cell death • Enzymes are released from the dead cardiac cells (important indictors of MI) • Proteolytic enzymes of neutrophils and macrophages remove all necrotic tissue by second or third day • Development of collateral circulation improves areas of poor perfusion • Necrotic zone identifiable by ECG changes an nuclear scanning • 10-14 days after MI, scar tissue is still weak and vulnerable to stress • By 6 weeks after MI, scar tissue has replaced necrotic tissue o Area is said to be healed, but less compliant • Ventricular remodelling o Normal myocardium will hypertrophy and dilate in an attempt to compensate for the infracted muscle Complications of MI • Dysrhythmias o Most common complication o Present in 80% of MI patients o Most common cause of death in the prehospital period o Life-threatening dysrhythmias seen most often with anterior MI, HF, or shock • Heart Failure o A complication that occurs when the pumping power of the heart has diminished • Cardiogenic Shock o Occurs when inadequate oxygen and nutrients are supplied to the tissues because of severe LV failure o Requires aggressive management ACS Collaborative Care • Nutritional therapy o Initially NPO o Progress to: Low salt, Low saturated fat, Low cholesterol • Rest and comfort o Balance rest and activity o Begin cardiac rehabilitation • Drug Therapy o Drug therapy o IV nitroglycerin o Morphine sulphate o β-Adrenergic blockers o Angiotensin-converting enzyme inhibitors o Antidysrhythmia drugs o Cholesterol-lowering drugs o Stool softeners ACS Nursing Management • Anxiety • Emotional and behavioural reaction • • • • • • • Maximize patient’s social support systems. Consider open visitation. Ambulatory and home care Patient and caregiver teaching Physical exercise Resumption of sexual activity Evaluation o Relief of pain o Preservation of myocardium o Immediate and appropriate treatment o Effective coping with illness-associated anxiety o Participation in a rehabilitation plan o Reduction of risk factors Questions • Which type of MI causes more damage to the myocardium? o STEMI • How many minutes of sustained ischemia does it take to cause irreversible myocardial cell death (necrosis)? o Approx. 20 mins o “Time is muscle” for MI’s o “Time is brain” for strokes • How many hours does it take for necrosis of the entire thickness of the myocardium? o 4-6 hours • After an MI, how many weeks does it take for scar tissue to replace the necrotic tissue? o 6 weeks • The patient receives IV morphine for chest pain. Which of the following results are the intended effects of morphine? Select all that apply. o A. Reduce myocardial oxygen consumption o B. Promotes reduction in respiratory rate o C. Reduces blood pressure and heart rate o D. Reduces anxiety and fear • A patient presents to the emergency department with an MI that damages the full thickness of the myocardium. What would the ECG changes reflect for this patient? • 2nd one • After a coronary angiogram through the right femoral artery, the nurse is not able to palpate the right pedal pulse. What is the nurse’s first action? o A. Elevate the legs o B. Change the IV rate o C. Use a doppler to assess the pulse o D. Call the doctor • Which of the following medications would a patient have to take for at least a year following an angioplasty to the RCA? o A. Warfarin and ASA o B. Heparin and ASA o C. Clopidogrel and ASA o D. ASA only