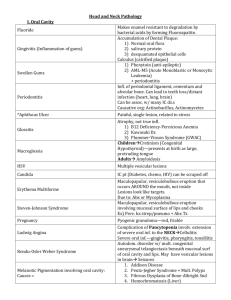
I. Oral Cavity Head and Neck Pathology Fluoride Gingivitis (Inflammation of gums) Swollen Gums Periodontitis *Aphthous Ulcer Glossitis Macroglossia Makes enamel resistant to degradation by bacterial acids by forming Fluoroapatite. Accumulation of Dental Plaque: 1) Normal oral flora 2) salivary protein 3) desquamated epithelial cells Calculus (calcified plaque) 1) Phenytoin (anti-epileptic) 2) AML-M5 (Acute Monoblastic or Monocytic Leukemia) + periodontitis Infl. of periodontal ligament, cementum and alveolar bone. Can lead to teeth loss/distant infection (heart, lung, brain) Can be assoc. w/ many IC dz.s Causative org: Actinobacillus, Actinomycetes Painful, single lesion, related to stress Atrophy, not true infl. 1) B12 Deficiency-Pernicious Anemia 2) Kawasaki Dz 3) Plummer-Vinson Syndrome (GWAC) ChildrenCretinism (Congenital Hypothyroid)—presents at birth as large, protruding tongue Adults Amyloidosis HSV Multiple vesicular lesions Candida IC pt (Diabetes, chemo, HIV) can be scraped off Erythema Multiforme Steven-Johnson Syndrome Pregnancy Ludwig Angina Rendu-Osler Weber Syndrome Melanotic Pigmentation involving oral cavity: Causes = Maculopapular, vesiculobullous eruption that occurs AROUND the mouth, not inside Lesions look like targets. Due to: Abx or Mycoplasma Maculopapular, vesiculobullous eruption involving mucosal surface of lips and cheeks Ex) Prev. hx strep/pneumo + Abx Tx Pyogenic granuloma—red, friable Complication of Pancytopenia involv. extension of severe oral inf. to the NECKCellulitis Severe oral inf.—gingivitis, pharyngitis, tonsillitis Autodom. disorder w/ mult. congenital aneurysmal telangiectasis beneath mucosal surf of oral cavity and lips. May have vesicular lesions in brain Seizures 1. Addison Disease 2. Peutz-Jegher Syndrome + Mult. Polyps 3. Fibrous Dysplasia of Bone-Albright Snd 4. Hemochromatosis (Liver) Hairy Leukoplakia Tumor-Leukoplakia Tumor-Erythroplakia Squamous Cell Carcinoma IC pt. Lateral border of tongue. Hyperkeratotic. Can NOT be scraped off. Dysplasia, Malignancy. Organism: EBV Precancerous—ventral(under) surface of tongue. Thickening of epithelium in Gingiva (white plaques)—4 diff. presentations. Can NOT be scraped off. Inflammation and Vasodilation Dysplastic lesion Tobacco and HPV 3 Stages: 1) Hyperplasia/Hyperkeratosis 2) Moderate Dysplasia (p53 mutation)—Inc. N:C, pre-malginant 3) SCC—disorderly cells entire thick, invade BM II. Nose and Sinuses Nasal Polyps Sinusitis Kartagener Syndrome Wegner’s Granulomatosis Necrotizing Lesions—Nose and URT Squamous papillomas Squamous Cell Carcinoma Hyperplastic glands w/ Infl. Due to recurrent rhinitis Organisms: Bacteria EXCEPT in Diabetics Mucormycosis Due to chronic rhinitis/tooth infection Sinusitis, situs inversus, Bronchiectasis, defective or inadequate cilia + infertile M Sinusitis, pneumocystis, glomerulitis cANCA Mucormycosis, Wegener, Extranodal NK T Cell Lymphoma Benign tumors of Nasopharynx HPV 6, 11 Malignant tumor of Nasopharynx AfricaChildren, AsiaAdults, rare in US EBV found in tumor cells Squamous cells in lymphoid background III. Larynx Laryngitis Squamous Papillomas Squamous Cell Carcinoma Serious Form: Haemophilus Influenzae in children. Can lead to Epiglossitis suffocation from airway obstruction Occur on TRUE vocal cords, no sequelae Adults—Solitary lesion Children—Multiple, recur, linked w/ HPV 6,11 KEY RF: Tobacco, gen. appear on vocal cord Persistent Hoarseness for months Late sx: Dysphagia, pain, hemoptysis (necrosis) IV. Neck Branchial Cyst Thyroglossal duct cyst Paraganglioma Lateral, second branchial arch remnant Midline, remnant of thyroid descent tract Benign tumor w/ Neurosecretory Carotid body, SNS and PSNS V. Salivary Gland Sial Adenitis Chronic Sialadentiis Anti-Ro in pregnancy Pleomorphic Adenoma Warthin Tumor Oncocytic Cells Mucoepidermoid Carcinoma Mumps (RNA virus) Children—No Sequelae Adults Pancreatitis, Orchitis Sjogren Syndrome Risk of Lymphoma in salivary galnds Anti-La (SSA) and Anti-RO (SSB) High risk intrauterine heart block of fetus Myoepithelial cells embedded in myxoid stroma First Presentation Facial Nerve Palsy Benign, most common (90%) tumor of salivary gland, recurs; commonly in Parotid Benign, Parotid; low recurrence (diff. from PA) M>F, 40-60 yo, Smokers Gross: encapsulated mass w/ cystic spaces Micro: Benign Glands lined by double layer of oncocytic cells surr. a lymphoid stroma Cells w/ large number of mitochondria on EM Malignant (most common malig.)-maj. Parotid Gross: Large, poor circumscribed, mucinous Miro: Squamous islets, mucous glandular struct. Prognosis dep. on GRADE (90 v 50% survival) Esophagus Pathology Plummer-Vinson Syndrome Achalasia Chagas Disease Food sticking in throat Sliding Hiatal Hernia Paraesophageal/Rolling Hiatal Hernia Zenker Diverticulum (Pharyngoesophageal) Epiphrenic Diverticulum Mallory-Weiss Syndrome Boerhaave Syndrome Esophageal Varices Pathogenesis Reflux Esophagitis (GERD) Upper webs, Iron Deficiency Anemia (Microcytic), Glossitis and Cheilosis Risk of post-cricoid Carcinoma Partial or incomplete relax. of LES on swallowing w/ increased resting tone Biopsy: diminished myenteric ganglia in body of esophagus/around LES S/Sx: Progressive dysphagia Sequelae: 5%-->Squamous Cell Carcinoma Secondary Chagas Disease Due to: Trypanosoma Cruzi S/Sx: Achalasia, toxic megacolon, dilated cardiomyopathy Achalasia or Carcinoma 95% of All, Cardia herniates upward (straight up—one line w/ esophagus) Gen. Greater curvature herniates alongside esophagus Associated w/ previous surgery (operation for sliding HH) Sequelae: Strangulation or obstruction Above the UES Etiology: cricopharyngeal motor dysfx w/ or w/o GERD and decreased lumen of UES Accumulates food Regurgitation, dysphagia, NECK MASS, aspiration pneumo Above LES—due to discord. peristalsis/LES relaxation *Nocturnal regurgitation of lots of fluid LONGITUDINAL tears of mucosa at EG jx Bleeding that resolves Alcoholics or with severe vomiting Can penetrate mucosa Complete perforation of the esophagus assoc. w/ M-W syndrome S/Sx: Pain radiating to back Severe/prolonged portal HTDilated veins beneath mucosa at Gastro-Esophageal Anastomoses: Coronary V.s in stomach and Plexi in distal esophagus IF >5mm RuptureLife-Threat Hemorr. (Hematemesis) (50% of deaths in pt w/ adv. cirrhosis) 40-50% pt die in 1st bleeding episode Most common cause, Adults >40yo Etiology: sliding HH, Dec. LES tone Inadequate or slowed esophageal clearance of refluxed material Achalasia Reflux Esophagitis Micro Reflux Esophagitis Clinical S/Sx Relfux Esophagitis Clinical Outcomes Barrett Esophagus Barrett Esophagus Clinical Features Herpes Esophagitis Candida Esophagitis Squamous Cell Carcinoma SCC Pathogenesis SCC Morphology (same for Esophagus and Gastric Carcinoma) SCC Micro Adenocarcinoma Adenocarcinoma Appearance Adenocarcinoma Clinical Sx Infl. cells in epithelial layer (neutrophils/Lymphocytes), basal zone hyperplasia Severity of sx does NOT correlate to degree of histo changes Heartburn, regurg. of sour brash, dysphagia Severe: Hematemesis, Melena Healing or Bleeding Complications: Ulceration, stricture, Barrett Esophagus ( Adenocarcinoma) Metaplastic Change: SquamousColumnar in LOWER esophagus Complication of chronic GERD Gross: Red, velvety appearance Dx requires: 1) Endoscopy—columnar epi above GE jx 2) Biopsy—Intestinal Metaplasia MOST Imp. RF for Adenocarcinoma 40-60 yo, White, M>F 30-40x Risk of Adenocarcinoma w >3cm BE Multiple punched-out ulcers that occur along ENTIRE length of esophagus Occur in immunosuppressed pt Dirty/gray pseudomemb. appearance Immunosupp. or diabetics Most common site: Middle 1/3 Adults > 50yo, M>F Blacks, Asians, and US increased risk—diet , Alcohol, tobacco, nitrosamines Poor prognosis due to insidious onset can recur local and distally Chronic EsophagitisDysplasiaCancer Can metastasize to regional nodes or spread by lymphatics locally 1) Exophytic/Protruded—60% 2) Flat (infiltrative)—15% 3) Excavated (necrotic ulceration)—25% can fistulate into trachea or aorta Pleomorphic, hypochromatic, large nuclei w/ prominent nucleoli. Pink collagen in cytoplasm. (signs of malignancy) >40 yo, median of 60 yo, M>F, White>Black p53 over-expression in Barrett Esophagus or p53 functional inactivation Lower 1/3 of esophagus Start as flat/raised patchesLarge nodules or infiltrate and ulcerate Most prod. mucin—Intestinal-type Epi Dysphagia, wt loss, hemorrhage, CP, vomit Poor prog. in general, > if superfic./resected Stomach Pathology Structure Cells Heterotopic Rests (Congenital) Diaphragmatic Hernia Pyloric Stenosis Acute Gastritis Pathogenesis Acute Gastritis Assoc. Chronic Gastritis Chronic Antral Gastritis Atrophic/Autoimmune Gastritis Granulomatous Gastritis GVHD Gastritis Fx of PG Synthesis by Mucosal Cells Peptic Ulcer Cardia—Mucous Cells Fundus-Parietal Cells and Chief Cells Antrum—Muscous Cells and G Cells G Cells-Endocrine-Gastrin EcL-Produce Histamine D Cells-produce Somatostatin Mucous Cells-prod. Mucus and Pesinogen II Parietal Cells—IF and HCl secretion Many mitochondria, eosinophilic Chief Cells: Pepsinogen I and II Tissue that doesn’t belong there Pancreatic—pylorusinflObstruction Gastric—DuodenumulcerBleeding Gastric—Upper EsophagusInfl., discomf. Defective closure, gen. on left. Asx or Respiratory problems in newborn Congenital hypertrophy of musc. propria Projectile vomiting at 2-3 weeks of age Assoc. w/ Turner Syndrome, atresia; M>F PE: palpable mass—feels like olive and visible peristalsis Together or individually: ↑Acid secr&Back diffusion + ↓ Bicarb buffer + ↓ blood flow Disruption of mucus layer or direct mucosal inj Acute gastritis 1) AlcoholicsMassive Hemorrhage 2) Aspirin for RA, may bleed Atrophy and metaplasia (w/o erosions) Dysplasia Neoplasia = complication Due to H. Pylori (G- curved rods) Hypochlorhydria NOT Anemia/Achlor. ↑Risk Gastric Carcinoma and Lymphoma Diffuse damage of Body and Fundus mucosa Autoimmune: Ab to Parietal Cells, Gastrin R, IF, and H+/K+ ATPase Anti-ParietalPernicious Anemia + Achlorhydria ↑Risk Gastric Carcinoma & Carcinoid Crohn’s Disease or Idiopathic Erosion of gastric mucosa 1) ↑ mucus and Bicarb. prod. 2) Vasodil., improved mucosal blood flow 3) Inhibit acid secr. by Parietal Cells Breach in mucosa that extends into submucosa or deeper H. Pylori Duodenum and Stomach Chronic, relapsing, Solitary EXCEPT in Zollinger-Ellison Syndrome H. Pylori Characteristics H. Pylori Diseases Pangastritis Acute Gastric Ulceration (NOT peptic ulcers) Hypertrophic Gastropathy – 4 Types 1. Menetrier’s Disease (Protein-losing gastropathy) 2. Parietal Cell Hypertrophy Hyperplastic Polyp—Benign Adenoma (Adenomatous Polyp) Gastric Carcinoma (50-60% in Pylorus and Antrum) Risk Factors for Gastric Carcinoma Zollinger-Ellison Syndrome Complications: Bleeding, Perforation, Obstruction from edema and scarring Multiple ulcers of stomach and duodenum + Diarrhea Tumors of pancreas produce gastrin (Gastrinoma) + Parietal Cells to secrete HCl and Peristalsis UreaseAmmonia and CO2 (Buffers gastric acid) and Toxic compounds (NH4Cl) PhospholipaseDamages surf. epith. ProteinsImmunogenic Adhesins Mobility Chronic gastritis, peptic ulcer, gastric carcinoma, MALT lymphoma High IL18 , PangastritisAtrophyCancer Multiple lesions = erosions and ulcers 1. Curling Ulcers – assoc. w/ severe burns or trauma, located in proximal Duodenum 2. Cushing Ulcers – assoc. w/ intracranial injury, occur in stomach, duod., esoph. & high incidence of perforation Mucosal epithelial hyperplasiaelargement /hyptertrophy of gastric rugae Can MIMIC: infiltrative carcinoma/ lymphoma on physical exam Excess acid secr. assoc↑risk peptic ulcer Males 40-60 yo Hyperplasia mucous cells, atrophy of glands Excess mucous and little acid in gastric secretionsProtein loss = Hypoproteinemia Assoc. w/ chronic use of acid secretion inhibitors (Proton Pump Inhibitors) Get: Parietal cell hypertrophy w/o excess acid! Common in chronic gastritis, NO malignant potential—Req. Biopsy to diff. from Adeno Proliferative dysplasia of epi w/ Malignant potential. Gen. Single and in Antrum Assoc w/ chronic gastritis w/ intestinal metaplasia 90-95% malignant tumors of stomach Japan, SA inc. risk due to salt in diet Very Poor Prognosis Linitis Plastica—leather bottle Environmental—Nitrites (food) Host—Chronic atrophic gastritis Genetic: Blood Group A, FMHx CDH1 and BRCA2Diffuse gastric cancer Morphology of Gastric Carcinoma Early Gastric Carcinoma Advanced Gastric Carcinoma Intestinal Type Carcinoma Gastric Type Carcinoma Gastric Carcinoma Clinical Krukenberg Tumors Virchow’s Nodes MALT Lymphoma Gastrointestinal Stromal Tumor Carcinoid Tumors Exophytic, Flat/depressed, Excavated/Ulcerative—heaped up, beaded margins and necrotic base (diff. from chronic peptic ulcer which is well demarcated, punched out lesion) Confined to: Mucosa and Submucosa regardless of LN met Extending below submucosa into muscle, regardless of LN met Glandular, expansile growth Mutations in β Catenin and APC Infiltrating pattern of poorly diff. cells + Signet ring conformation , Gastric-type mucus cells that don’t form glands but permeate the wall as indiv. cells or clusters Insidious, Asx until late-wt loss, abd p, anorexia, vomiting, altered bowel habits Hemorrhage may occur due to necrosis Metastasis to ovaries (In GC) Metastasis to L Supraclavicular Node often First clinical manifestation of GC t11;18 Stomach is most common site for extranodal lymphoma—EBV assoc. too Mutation of gene encoding tyrosine kinase cKIT Most commonly in SI (Small bowel) Gen. older adults-50-65 yo Triad: Diarrhea, Flushing, Asthma May hear tricuspid murmur via thickening Dx Test: 5-HIAA (Breakdown of Serotonin) Small Intestine Pathology Blood Supply to SI Special Glands of Duodenum Heterotopia Atresia -congenital Stenosis-congenital Meckel Diverticulum -congenital Secretory diarrhea Osmotic Diarrhea Exudative Diarrhea Rotavirus Norwalk Virus GVHD esp. bone marrow transplant Radiation Malabs. snd most common in US Key Sx of Malabs: Celiac Disease –Gluten-sensitivity Required for Dx of Celiac Disease Dermatitis Herpetiformis Whipple Disease Malabs. 1. Duodenum – Gastroduodenal and SMA 2. Rest of SI Superior Mesenteric A. Brunner’s Glands—Submucosal Congenital Anomaly—gen. Pancreaticinfl. maybe gastriculcers Duodenal atresia most common May be acquired via intussusception Failure of vitelline duct (gut to yolk sac) to involute. True Diverticulum. Heterotopic rests in 50%. May see bleeding if ulcer. Isotonic, >500mL/day. Rotavirus, E. Coli, Cholera, villus adenomas, laxatives, VIPoma >500mL/d, osmolality >plasma by 50mosm Lactase deficiency, antacids Purulent, bloody stool=Shigella, Salmonella Outbreaks in infants Outbreaks in school children and adults Focal crypt cell necrosis Severe, watery diarrhea Endothelial cell inj.-->Ischemic fibrosis and stricture. Acute: Anorexia, cramping, malabs. Chronic: Inflammatory enteritis Pancreatic insuff., Celiac Sprue, Crohn’s Anemia—B12, folate Petechiae—Vitamin C Skin Problems—Vitamin E (dermatitis) Bone Pain/tetany--Calcium Chronic, mucosal lesion of SI = malabs. Caucasians, improves w/ remove wheat HLA-DQ2 and DQ8 Anti-Gliadin or Anti-Endomysial AbIgA T-Cell mediated HS (CD8, CD4+Gliadin) Gross: flat mucosa LM: marked atrophy of villi *HIGH RISK OF LYMPHOMA Malabs sx, SI biopsy, sx improve w/o gluten *Dermatitis Herpetiformis *Granular IgA deposit in dermal papillae Vesicular lesions on extensor surfaces only Systemic Disease-CNS, joints, GI Trophyrema Whippeli (G+ actinomycete) White, middle-aged Males *Lamina propria laden w/ distended MΦs PAS+ Rods Lymphadenopathy + Hyperpigmentation of skin, joint problems 1st sign Abetalipoproteinemia Infants: failure to thrive, steatorrhea Inborn error of metab. (AR) Ischemic bowel disease Incarceration in hernia Strangulation in hernia Intussusception Adenoma Def. of β-Lipoprotein req. for transport of intestinal chylomicrons. ↑TG Enterocyte Vacuolation ↓ LDL, VLDL, CM Acanthocytes (Burr cells) Histo: Coagulative necrosis Transmural = Poor prognosis – perforation quickly, sudden severe abd. P!, N/V/D/M Edema from impaired Venous drainage Compromised Arterial & Venous—infarct Infants/ Young kids: Currant-Jelly Stool Adults: neoplasms Benign, Ampulla of Vater (obstructive jaundice) 40-70 yo, maj. in Duodenum Major RF: Infl. from Celiac Disease ↑ in familial polyposis Clinical: Occult blood FOR Small Intestine—UWORLD LM Finding of intestinal Mucosa 1. marked atrophy of intestinal villi Celiac Disease 2. Distended MΦs in intestinal lamina propriaWhipple Disease 3. collections of neutrophils in crypt lumina Ulcerative Colitis 4. Intestinal infl. w/ scattered non-caseating granulomas Crohn Disease 5. massive infiltration of intestinal lamina propria w/ atypical lymphocytes Gastrointestinal Lymphoma Large Intestine Pathology Blood Supply (Know for vignettes assoc w/ thrombosis) Hirschprung Disease Pseudomembranous Colitis Crohn’s Disease (IBD) Ulcerative Colitis (IBD) Crohn’s Disease Ulcerative Colitis IBD (Both) Crohn’s Key Sx: UC Key Sx: Key Complications of Crohn’s Key Complications of UC Extra-Intestinal Manifestations of Crohn’s Ascending/Proximal Transverse – Superior Mesenteric A. Rest of Colon to rectum – Inf. MA Upper Rectum – Superior Hemorrhoidal A. (off IMA) Lower Rectum – Hemorrhoidal br.s off Internal Pudendal A. Absence of ganglion cells (Auerbach’s and Meissner’s) in part of GI Neural crest cell migration defect Dilation proximal to aganglionic segment Meconium Ileus—failure to pass meconium in infants C. Diff, can be w/o abx after surgery or debilitating illness, + Exotoxins A,B,C Plaque-like adhesions w/ fibrinopurulentnecrotic debris and mucus, adherent to damaged mucosa. Granulomatous infl. that can be found ANY part of GI, esp. Ileum. Transmural Infl.. Skip Lesions. Ulcers, fissures. *Non-Caseating Granuloma ↓ Th cells in periphery = ↑risk viral and fungal inf. String Sign on X-Ray(narrowed lumen) Nongranulomatous, confined to Colon/rectum. Superficial continuous Infl(mucosa). Ulcers, Pseudopolyps. *Crypt Abscesses Cobblestones HLA-DR1/DQw5 pANCA HLA-DR2 HLA-B27 Ankylosing Spondylitis AND inflammation is FINAL common pathway Diarrhea/fever/P! separated in time, may be precipitated by stress Bloody, mucoid, diarrhea-relapsing after mo. to decade and persists days to months Strictures Fistulas Malabsorption + Protein-Losing enteropathy ↑Risk cancer w/ pancolitis Toxic Megacolon Erythema Nodosum Migratory Polyarthritis Sacroilitis Extra-Intestinal Manifestations of UC Angiodysplasia Peutz Jeghers Syndrome Villous Adenoma Familial Adenomatous Polyposis (FAP) Gardner Snd Turcot Snd Multiple Hit for Adenoma-Carcinoma Lynch Syndrome (HNPCC) Adenocarcinoma =98% colon cancer Carcinoid Tumor Carcinoid Snd Sx: Acute Appendicitis Mucinous Cystadenocarcinoma in Appendix Ankylosing Spondylitis Primary Sclerosing Cholangitis (pANCA) Clubbing of fingers Uveitis, arthritis, DVT, pyoderma gangrenosum, ankylosing spondylitis Tortuous dil. of sumuc/muc BV Sx: Hematochezia Melanotic change incl. mouth + Polyps Increased risk carcinoma of pancreas and ovary NOT colon. Increased risk of cancer Hypokalemia—due to inc. SA for fluid secr. APC gene on Chromosome 5 (Adenomatous polyposis coli) Adenomatous polyps that carpet mucosa Clinical: Presents in teens-20s ALL have Adenocarcinoma in 10-15y FAP + Osteoma (Mandible/skull/long bone) Polyposis of colon + Gliomas 1st Hit—Abnormal APC 2nd Hit: Loss of normal APC 3rd hit: KRAS mutation 4th Hit: Inactivationg of p53 =Adenoma DNA Mismatch Repair defect 60-79 yo If in young: must suspect Hx of UC or Polyposis snd. 55% Rectosigmoid Proximal colon more dangerous, larger lumen, meaning no obstruction until late. Any pt >50yo w/ microcytic anemia (Iron def. anemia)—GI cancer until proven otherwise Liver is primary site of met Appendix MC site (w/ obstruction) then SI RARELY met, but if so it’s extensive, to liver = carcinoid Snd Gross: Solid yellow/tan Carcinoid Snd: 5-HIAA in urine and blood (breakdown of serotonin) Good prognosis if not spread Flushing, hypermotile GI, Bronchoconstr., hepatomegaly, systemic fibrosis, tricuspid murmur MCC: Obstruction via fecolith. pinworms too. Mainly Adolesc., young adults Dx: NΦ in muscularis Pseudomyxoma peirtoneii (mucin in peritoneal cavity w/ rupture of appendix) Liver Pathology Jaundice Unconjugated Hyperbilirubinemia Hemolysis Familial Unconj. Hyperbilirubinemia Anemia + ↑LDH1 + ↓Haptoglobin + ↑Retic Crigler-Najjar 2 3 ↑LDH1 (Pre-hepatic) 1 Fatal ↓ Activity, Live Gilbert Snd. LDH1 specific to RBCs Mut. of UGT Promoter Conjugated Hyperbilirubinemia 80% Direct Bilirubin Obstruction Familial Conjugated Hyperbilirubinemia Extrahepatic Intrahepatic CA head of Pancreas OR Primary Sclerosing Cholangitis (pANCA ) CA of Ampulla of Vater OR Direct Bilirubin >5 Alk Phosphatase >500 Primary Biliary Cirrhosis (Anti-Mitochondrial Antibodies) OR Cholestasis in Pregnancy Direct Bilirubin <5 Alk Phosphatase <500 Rotor Dubin Johnson Black Liver Mixed Hyperbilirubinemia Unconjugated 50% Conjugated 50% Parenchymal Disease Hepatitis Autoimmune Infectious Hepatitis B Serology Hepatitis A Type I Type II Anti-SMA Anti-KLM Serology Elevated Liver Enzymes: ALT + AST+ LDH5 (In 1,000s due to necrosis) Elevated Liver Enzymes: ALT + AST +LDH5 (In 1,000s due to necrosis) NOT Alk phosphatase (No obstruction) NOT Alk phosphatase (No obstruction) Heme Metabolism Drug that impairs Bilirubin uptake in liver Elevated Unconjugated Bilirubin Elevated Conjugated Bilirubin Elevated 50/50 LDH Hepatocyte Integrity Biliary Excretory Function Hepatocyte Function Acute Hepatic Failure Chronic Hepatic Failure Sx of Hepatic Failure Hyperestrogenemia sx Cause of Hepatorenal snd? Morphology of Acute Viral Hepatitis Hepatitis A (ssRNA-Picorna-N) Hepatitis B (dsDNA-Hepadna-E) HemeBiliverdin (Heme Oxygenase) BiliverdinBilirubin (Biliverdin Reductase) -Unconjugated BilirubinRifampin (may prevent binding to anion binding protein) Pre-hepatic problem Obstruction Parenchymal liver disease (problem with hepatocytes) LDH1 – Heart and RBC LDH3 – Lungs LDH5 – Liver Cytosolic hepatocyte Enzymes: AST, ALT, LDH Direct Bilirubin Plasma Membrane Enzymes: Alkaline Phosphatase –Not specific Hepatocyte Metabolism: Serum Ammonia Hepatic Failure Proteins secreted into blood ( ↓ ): Serum Albumin Factors V, VII, X, PT, Fibrinogen PT Time Massive Necrosis Drugs: Acetaminophen, Halothane, Rifampin Toxins: Mushrooms, CCl4 Viral Hepatitis: Hep A and B Caused by Cirrhosis Cirrhosis requires? 1. Degen. of hepatocytes 2. Regen. of hepatocytes 3. Fibrosis Jaundice, HYPOalbuminemia, HYPERammonemia (w/ Hepatic Encephalopathy), HYPERestrogenemia, coagulopathies, hepatorenal snd Palmar erythema, spider angiomas, hypogonadism and gynecomasti in males Tubular damage by bile plugs (Large amt of bilirubin excreted in urine) Hep B Ground glass hepatocytes (HBsAg) Hep C Fatty change Active Hepatitis Ballooning Degeneration Maybe cholestasis (bile plugs in canaliculi) Apoptosis Mallory Bodies 2-4 weeks incubation, fecal oral Dx: IgM Ab Acute Phase Can be fulminant, Never chronic 1-4 month incubation, Blood/Birthing/Baby-making Dx: HBsAg or HBcAb Hepatitis B (dsDNA-Hepadna-E) Hepatitis C (ssRNA-Flavi-E) Hepatitis E (RNA-Herpes-N) Hepatitis D (RNA-Delta) Other causes of Chronic Hepatitis Major causes of death in Chronic Hepatitis Auto-Immune Hepatitits Type I Autoimmune Hepatitis MCC Chronic Liver Disease NAFL and NASH Pathogenesis of NAFL and NASH Hemochromatosis Wilson’s Disease 3 Presentations: 1. Acute w/ resolution 2. Chronic - Cirrhosis or Carrier 3. Fulminant Hepatitis Fatal Inc. Risk Hepatocellular CA 7-8 week incubation, parenteral/IVD/Cocaine intranasal Maj. Chronic Fulminant is VERY rare Dx: HCV Ab after 3-6 weeks (IgG) –for life via ELISA or HCV RNA ↑risk Cirrhosis, Carcinoma 4-5 week incubation High mortality in pregnant F Dx: PCR, IgM and IgG Ab Dx: IgM and IgG ab, HDV RNA serum, HDAg liver Wilson Dz, alpha-1 AT, Alcoholic, Drugs (Isoniazid/methyldopa), Autoimm. Cirrhosis, Liver Failure w/ hepatic encephalopathy, Massive hematemesis from varices, hepatocellular CA (HBV-esp. Neonates or HCV) Predom. F w/ ↑Risk RA, Thyroiditis, Sjogren, UC; Elevated IgG; HLA-B8 or Drw3 responds well to anti-infl. Associated with HLA-DR3 +ANA, SMA, AAA Solube Ant-liver and Anti-Pancreas Ag Ab (SLA/LP) Non-Alcoholic Fatty Liver Disease-3 types 1. Simple hepatic steatosis 2. w/ min. infl. 3. non alcoholic steatohepatitis (NASH)Serious –can lead to cirrhosis Obesity, Insulin-R/Hyperinsulinemia, Dyslipidemia, Type II DM Principal Cause of Cryptogenic Cirrhosis 2 Hit: 1. Hepatic fat accum. 2. oxidative stress Lipid peroxidation ROSDmg Due to def. of Hepcidin deposition of iron in parenchymal cells Mutation of HFE (CysTyr = C282Y) Activates Stellate Cells Collagen Clinical Triad: Cirrhosis, DM, Bronze Skin (due to ↑pituitary hormones!) Also: Arthralgia, ED, Arrhythmia Accumulation of Copper in tissues: Brain (Basal Ganglia), Liver hepatocytes, Eye Dx: Liver Biopsy Presentation: Adolescent w/ diff. in school, Alpha-1 Antitrypsin Deficiency new onset ataxic gait, maybe tremors. Eye exam shows green-yellow ring around cornea. Emphysema and Liver Disease Histo: PAS + Intrahepatic inclusions Intrahepatic Biliary Tract Diseases Primary Sclerosing Cholangitis Primary Biliary Cirrhosis Secondary Biliary Cirrhosis All 3 Lab Findings M>F, IBD common, Beaded Intrahepatic Ducts (US), +pANCA Onion skinning of intrahepatic bile ducts Sx: pruritis, jaundice, dark urine, light stool, hepatosplenomegaly Inc. Risk Extrahepatic bile duct CA F>M, Autoimmune Anti-Mitochondrial Ab Sx: Extreme itching—bile salts in skin Liver Biopsy: Granulomas around ducts w/ lymphocytic infiltrate in portal tracts Extrahepatic bile duct obstruction, biliary atresia, gallstones, stricture, CA of pancreatic head Sx: same as PSC Conjugated Hyperbilirubinemia (obstruct.) Inc. Alk Phos, Bile Acids, Choleset↑ Extrahepatic: Alk Phos >500, Bili >5 Intrahepatic: Alk Phos <500, Bili <5 Drug Induced Liver Diseases Injury Pattern Cholestasis Morphologic Findings Bland biliary plugs, no infl Cholestatic Hepatitis Cholestasis w/ lobular necrosis and infl. Macrovesicular Steatosis Steatohepatitis Microvesicular, Mallory Bodies Fibrosis + Cirrhosis Periportal and pericellular fibrosis Noncaseating epitheloid granulomas Sinusoidal Obstruction Syndrome (Venous occlusion)—Obliteration of Central Veins Granulomas Vascular Lesions Ex. of Agents Estrogen (BC, steroids, postmenopause) Antibioitics Phenothiazines ETOH, MTX, Corticosteroids, Total Parenteral Nutrition Amiodarone ETOH Tetracycline MTX, Isoniazid, Enalapril (Iso is anti-Tb) Sulfonamides High Dose Chemo Neoplasms Budd-Chiari Syndrome = Hepatic Vein Thrombosis --medical emergency w/ severe abdominal pain Oral Contraceptives Sinusoidal Dilatation Oral contraceptives, etc. Peliosis Hepatis-blood filled cavities NOT lined by endothelial cells—can rupture causing intraabd. hemorrhage Hepatic Adenoma Anabolic steroids, Tamoxifen Hepatocellular Carcinoma & Cholangiocarcinoma Thorotrast Angiosarcoma Thorotrast and Vinyl Chloride Oral contraceptives, Anabolic Steroids Chronic anemia since childhood assoc. with Budd-Chiari (severe abd P!)— Paroxysmal Nocturnal Hemoglobinuria Pathogenesis of hepatic injury in Alcoholic Liver Disease 1. Steatosis due to shunting normal substrates away from catabolism and to lipid biosynthesis due to 1. generation of NADH by alcohol dehydrogenase and acetaldehyde dehydrogenase; 2. Impaired assembly and secretion of lipoproteins 3. peripheral catabolism of fat. 2. Induction of cytochrome p-450 that makes other drugs toxic 3. Free radical formation from microsomal ethanol-oxidizing system oxidizes alcohol and they react with cell membranes 4. Alcohol directly toxic to microtubular and mitochondrial function 5. Acetaldehyde induces lipid peroxidation and acetaldehyde-protein adduct formation disrupts cytoskeleton and membrane Cellular Damage 6. Alcohol induces immunologic attack on hepatic neoantigens, 7. Collagen –Stimulated by inflammatory cytokines or those form Kupffer cells Morphology: Definition Hepatic steatosis = fatty changeReversible if they abstain alcoholic hepatitis= Necrosis (if continued exposure) Fatty change and necrosis cirrhosis = chronic damge Nodular liver w/ fibrosis Labs: AST/ALT/LDH –mild elevated; Alk Phos-Miled elevated (<500) REQUIRES 3 comp: Degen, Regen, Fibrosis w/ hepatitis + abstinence—resolves and left w/ fatty change Gamma GtSensitive marker for alcohol exposure (Glutamyl transferase…) –Release is stimulated by alcohol, microsomal enzyme. Elevated in binge drinking, relapsing alcoholics. Causes of death are Hepatic coma, massive GI bleed, intercurrent infection, hepatorenal syndrome, hepatocellular carcinoma in 3-6% Cirrhosis Definition: 1. Bridging fibrous speta- delicate bands of fibrous c.t. replace adjacent lobules 2. Parenchymal nodules – due to regeneration of encircling hepatocytes; small (micronod.)< 3cm – large (macronod.) several cm. 3. Disruption of entire liver architecture 4. Diffuse injury – has to be throughout liver 5. Nodularity – balance between regeneration and scarring 6. Fibrosis – irreversible 7. Vascular architecture reorganized – due to parenchymal injury and scarring, abnormal interconnections between vascular inflow and hepatic vein outflow channels Hepatic Dz. In pregnancy Hepatic Adenoma Child Malignancy Adult Malignancy Hepatocellular CA Preclampsia and Eclampsia: HELLP Snd Hemolysis Elevated liver enz. Low Platelets DIC Acute fatty liver of pregnancy MICROvesicular infiltration Intrahepatic Cholestasis (Estrogen) -3rd Tri Extreme Pruritis Dark urine/Pale stool Jaundice Presents w/ Severe RUQ Assoc. w/ oral contraceptives—young F Hepatoblastoma—chromosomal del. Angiosarcoma—Vinyl chloride Very aggressive Assoc. w/ cirrhosis related to HBV/HCV Other cause: Aflatoxins-long standing consumption of food Clinical Features: ill-defined Elevated Serum Alpha-Fetoprotein = HCC Metastatic Tumors—MCC liver CA #1 = Colon #2 = Breast #3 = Lung Usually multiple and necrotic Very few clinical manifestation