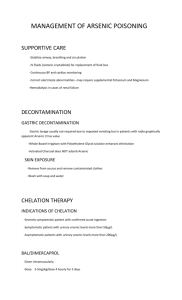
CASE STUDY: ARSENIC POISONING (Toxicology) A patient is suffering from arsenic poisoning. Arsenic is a metalloid element that occurs naturally. Abdominal discomfort, nausea, vomiting, diarrhea, and other gastrointestinal symptoms are frequently experienced by victims of acute poisoning. People who are affected could have a garlicky breath or stool odor. Depending on the quantity and kind of arsenic consumed, the ensuing dehydration herald’s cardiovascular instability, which develops quickly and proceeds from sinus tachycardia to orthostatic hypotension with a potential for shock and death. Patients may have delirium, confusion, seizures, and coma as a result of severe encephalopathy. Rhabdomyolysis and severe renal failure are two more acute consequences. At 2:17 PM, a 48-year-old male enters the emergency room. The patient's wife, a witness who brought the patient, claimed that the patient had ingested "white powder" from a bag that was handed over to him by a friend. He then developed weakness, vomiting, and diarrhea. The emergency department's early treatment to the patient was based on sensory symptoms, which typically present first and include "pins and needles" or pains similar to an electrical shock in the lower extremities. Early evaluation may reveal a single, weak, or nonexistent vibratory sensation. Later on, motor weakness may appear and occasionally seem like Guillain-Barré syndrome. Hepatitis and reversible pancytopenia might develop within a week after the initial illness. After very severe acute and chronic exposures, skin lesions, a dry, hacking cough, and Mees lines (horizontal, 1-2 mm white lines on the nails) can also appear. Further inspection quickly revealed a white powder that had been clearly identified to be arsenic, and a urine spot test was submitted for confirmation of ingestion after the identification. The lab was consulted to determine the arsenic levels in the blood and urine. Extreme care must be used to treat acute arsenic toxicity since it poses a serious health risk. The primary goals of treatment should be to stabilize the airway, breathing, and circulation. A cardiac monitor with continuous pulse oximetry should be used, and the patient should get two large-bore IVs. While pressor drugs could be necessary, crystalloid fluids should be used to treat hypotension. As cerebral and pulmonary edema may develop, fluid status needs to be closely monitored. Maintaining appropriate levels of urine output and potassium, calcium, and magnesium concentrations is important. Ventricular dysrhythmias could happen. Electrical defibrillation and lidocaine are used to treat ventricular tachycardia and ventricular fibrillation, respectively. Agents that prolong the QTc should be avoided due to the association between arsenic and QTc prolongation (class IA, IC, and III antidysrhythmic agents). Bicarbonate therapy might be successful.