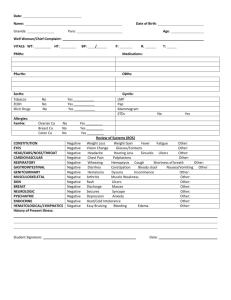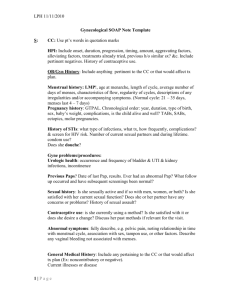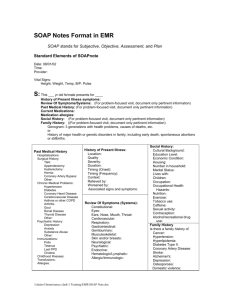
Virginia Jenkins NURS 7101 M50 Soap #2 SUBJECTIVE: Chief Complaint: Wellness visit History of Present Illness: Tina Jones is a 32-year-old African American female established patient who presents to the clinic for her annual wellness visit. Pt. denies any changes in health since her last visit. She denies pain. If pt. had a CC involving pain OLDCARTS would be evaluated. O: (onset) When did symptoms begin? Gradual or sudden? L: (location) Can you point to where the pain is? D: (duration) How long or how often? C: (character) Can you describe the pain? Ex. Burning, gnawing, sharp, dull. A: (aggravating/relieving factors) Is there anything that makes the pain better or worse? R: (radiating) Does pain travel to other parts of the body? T: (timing) Intermittent, Constant? S: (severity) Can you rate your pain on a scale of 1-10? Do symptoms interfere with daily life? Medications: Albuterol inhaler prn Lisinopril 20mg QD Metformin 500mg Bid Crestor 20 mg HS Lo Loestrin Fe QD Do you take your medications as prescribed? Do you take any vitamins, herbs, home remedies, or OTC medicine? When was the last time you used your inhaler? Do you have any trouble getting or accessing your medications? Allergies: Do you have any new allergies? Past Medical History: HTN, Type II Diabetes, Hyperlipidemia, Asthma Family History: Any new diagnoses in your family of chronic disease or terminal illness? Virginia Jenkins NURS 7101 M50 Personal & Social History ● Personal Status- graduate engineering student who works part-time as a barista on the weekends Have you visited the ER since your last visit? Have you been hospitalized or had surgery since your last visit? Have you had any new diagnoses, immunizations, diagnostic tests or screenings (last pelvic exam and PAP)? ● Social Relationships- Ask about: significant others, roommates, sexual partners, social interactions with friends ● Diet/Nutrition- Ask about: food preferences, caffeine-containing beverages, changes in appetite or weight, typical breakfast/lunch/dinner/snack. ● Functional Ability-Ask about: ability to perform self-care activities, ability to perform skills needed for independent living. ● Mental Health: Ask about personal stress, sources of stress, feelings of depression, anxiety, irritability, anger, thoughts of suicide. ● Tobacco, ETOH, Illicit Drug Use: Pt. drinks a couple of glasses of wine on weekends to wind down from the week. Denies smoking or illicit drug use. ● Health Promotion-Exercise, stress management, sleep habits, routine exams, safety practices. ● Environment-safety concerns, potential hazards at work or home Review of Systems: ● Constitutional Health-fatigue, weakness, night sweats, unexplained weight changes, fever, issues with sleep. ● HEENT- head, eyes, ears, nose, throat Head – Headaches? Ears – Any pain, cerumen, discharge, infection, decreased hearing, tinnitus? Eyes – How is your visual acuity, changes in vision, blurriness, discharge? Nose – Have you had any nasal discharge, epistaxis, sneezing, obstructions? Throat – Have you had any mouth and oropharynx soreness, hoarseness, mouth or tongue lesions, abscesses, ulcers, bleeding gums? Neck – Do you have lymph node enlargement, edema, masses, pain, tenderness, stiffness? Virginia Jenkins NURS 7101 M50 ● Respiratory System- Have you had cough productive/non-productive, hemoptysis, frequent colds, wheezing, dyspnea, snoring? ● Cardiovascular System Heart – Have you had palpitations, chest pain or tightness, dyspnea, orthopnea? PV – Have you had coldness or warmth of extremities, numbness, edema, varicose veins, pain at rest or with movement, changes in color? ● GI/GU General Abdomen – Any pain, heartburn, N/V, dysphagia, hematemesis, jaundice, ascites? Elimination –Any change in bowel habits, pain or difficulty with defecation, gas, bloating, changes in stool consistency or color, blood in stool, diarrhea/constipation. Characteristics of urine, hesitancy, frequency, urges, changes in urine stream. ● Reproductive System Female Genitalia – presence of lesions, pain, discharge, odor, menstrual history (date of onset, LMP, length of cycle, amenorrhea, dysmenorrhea, menorrhagia). Sexual History – Have you had any new sexual relationships? What is the orientation of your partner preference? How many partners have you had since your last visit? Have you been using contraception, what kind, is it effective? ● Musculoskeletal Muscles – Have you had twitching, cramping, weakness, pain? Bones/Joints - Have you had joint edema or pain, redness, stiffness, deformity, crepitus, ROM issues? ●Neurological General – Have you had syncope, changes in LOC, seizures, cognitive changes (confusion/memory loss)? Gait – Have you had any loss of coordination, ataxia, paralysis, paresis, tremors? Sensory – Have you had paresthesia, pain? ●Endocrine-Have you experienced any intolerances in heat or cold? Increased thirst, changes in facial or body hair? Changes in skin? Unexplained weight change? OBJECTIVE: Vital Signs: BP 122/84, HR 76, Resp 16, Temp 98.6, O2Sats 99% on RA. She denies any pain. Virginia Jenkins NURS 7101 M50 General Survey: Appearance, LOC & MMSE, height/weight, BMI, waist circumference Assessment: Inspection, Palpation, Auscultation, Percussion. (Neck, Eyes, Ears, Skin, Respiratory, Cardiovascular, Gastrointestinal, (Reproductive if pt. does not see a separate provider for gynecological needs). ● Inspection Skin – color, suspicious moles or skin lesions Neck – symmetry, alignment of trachea, landmarks of triangles, suppleness, masses, JVD distention Eyes – check vision (visual acuity screen) Ears – check hearing (Weber, Rinne, Whisper tests) Throat – mouth and oropharynx soreness, hoarseness, mouth or tongue lesions, abscesses, ulcers, bleeding gums? Chest– movement for symmetry, use of accessory muscles Heart - apical pulse, pulsations, heaves, lifts Abdomen – masses, hernia, separation of muscles, contour, symmetry Breast - Erythema, puckering, or peau d'orange, venous patterns, contour, symmetry Genitalia - lesions, pain, discharge, odor ● Palpation Neck – trachea, thyroid, paravertebral muscles, lymph nodes Chest – thoracic expansion, crepitus, vibrations, fremitus Heart/PV – apical impulse, thrills, heaves, lifts, dorsalis pedis pulses, radial pulses, temperature of extremities, edema Abdomen – muscle resistance, tenderness, masses, bulges, liver, gallbladder, spleen, kidneys, aortic pulsation Breast – lymph nodes, masses, tenderness Pelvic exam - -vaginal walls for smoothness, tenderness, lesions -uterus for location, position, size, shape, contour, mobility, tenderness -ovaries for size, shape, consistency, tenderness -adnexal areas for masses and tenderness. ● Auscultation Virginia Jenkins NURS 7101 M50 Chest – breath sounds, vocal resonance Heart – carotid arteries (bruits), 5 cardiac areas, extra sounds, murmurs Abdomen – bowel sounds, aortic, renal, iliac, femoral arteries (bruits) ● Percussion Chest – tone, diaphragmatic excursion Heart – estimate heart size Abdomen – tone, liver borders, splenic dullness, gastric bubble ASSESSMENT: ● Problem List 1.Asthma 2.HTN 3.DB II 4.HLD ● Labs/Diagnostics CBC- ensure adequate levels of blood and oxygen carrying capacity, evaluate immune function. CMP – Evaluate kidney, liver function, and electrolyte balances that may point to underlying disease process or complication d/t medications. Lipid profile – pt. has diagnosis of HLD. Lipid profile can help determine if medication is effective. PFTs – Monitor asthma, symptoms can vary over time. A1C – Evaluate blood sugar level over past 3 months to determine level of control. Vitamin D level- Pt. Has risk factor as AA of having deficient vit D levels that is a known contributor to CVD and diabetes. Pap smear (if not done in past 3 years per USPSTF) - some pts. Do not see a separate doctor for these tests. HCG – Pt. Is taking BC pills and is of childbearing age. PHQ-2 if positive add PHQ-9 – annual screen recommended by USPSTF. PLAN: Administer any needed immunizations such as flu shot. Educate Ms. Jones on continuing medications as prescribed pending lab results. Virginia Jenkins NURS 7101 M50 Offer resources to obtain consistent medical care and access to medications if needed. Educate pt. on the importance of healthy diet, exercise, STI prevention, asthma triggers, and regular BS and BP checks. Recommended screenings over the next 5 years: Annual pelvic/breast exam, annual depression screen, Pap smear every 3 years, annual wellness exam with PCP. Follow-ups: as needed. References Ball, Jane W., Dains, Joyce E., Flynn, John A., Solomon, Barry S., Stewart, Rosalyn W. (2019). Seidel's guide to physical examination: An interprofessional approach (9th ed). Elsevier. Johns Hopkins Medicine. Pulmonary function tests. Retrieved from https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/pulmonaryfunction-tests Parva, N. R., Tadepalli, S., Singh, P., Qian, A., Joshi, R., Kandala, H., Nookala, V. K., & Cheriyath, P. (2018). Prevalence of vitamin D deficiency and associated risk factors in the US population (2011-2012). Cureus, 10(6), e2741. https://doi.org/10.7759/cureus.2741 United States Preventive Services Task Force [USPSTF]. (2022). 2022 adult preventive health guidelines: Ages 19 through 64 years. Retrieved from https://content.highmarkprc.com/Files/Region/hbsneny/EducationManuals/PreventiveHea lthGuidelines/neny-guidelines-2022-19to64.pdf