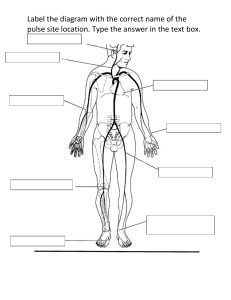
Chapter 29 – Bedside Assessment General Appearance 1. Facial expression: whether appropriate for the situation. 2. Body position: whether relaxed and comfortable or tense and in pain. 3. Level of consciousness: whether alert and oriented, attentive to your questions, and responding appropriately. 4. Skin colour: whether tone is even and consistent with ethnocultural heritage. 5. Nutritional status: whether weight appears in healthy range, fat distribution is even, and hydration appears healthy. 6. Speech: whether articulation is clear and understandable, pattern is fluent and even, and content is appropriate. 7. Hearing: whether responses and facial expression are consistent with what’s being said 8. Personal Hygiene: ability to tend to hair, makeup, shaving Measurement 1. Measure baseline vital signs: temperature, pulse, respirations, BP. Note whether you must avoid an arm because of surgery, mastectomy, IV access, or dialysis shunt. Collect and document vital signs more frequently if patient is unstable or patient condition changes. 2. Measure oxygen saturation (pulse oximetry): maintain at 92% or higher, or as ordered (e.g., 88 to 92% for patients with COPD) 3. Ask the patient to rate pain level on a scale of 0 to 10, at rest and with activity; note location and quality of pain. If appropriate, use the Faces Pain Scale-Revised. 4. Assess pain intensity on a scale of 0 to 10 before and after administration of analgesics, note response according to known pharmacokinetics of the analgesic, approximately 15 minutes after IV administration and 1 hour after oral administration. Neurological System 1. Note whether the patient's eyes open spontaneously to name 2. Note whether the patient's verbal response makes sense, and the speech is clear and articulate. 3. Measure right and left pupil sizes in millimetres and assess reaction to light. 4. Note whether the patient's motor response in upper and lower extremities is strong and equal bilaterally. 5. Assess muscle strength of right and left upper extremities, with the use of hand grips. 6. Assess muscle strength of right and left lower extremities, pushing feet against your palms. 7. Note any ptosis or facial droop. 8. Evaluate sensation (omit unless indicated). 9. Assess the patient's ability to swallow. Respiratory System 1. If the patient is receiving oxygen by mask or nasal prongs, check fitting and assess skin integrity of the nares and behind the ears. 2. Note fraction of inspired oxygen (FiO,). 3. Assess respiratory effort. 4. Inquire whether the patient is short of breath at rest or on exertion. 5. Auscultate breath sounds (do not listen over the patient's gown), and Compare sides: Anterior lobes: right upper, left upper, right middle, and lower, left lower Posterior lobes: left upper, right upper, left lower, right lower (if the patient is not able to sit up, have another nurse hold patient to each side) 6. Instruct the patient to cough and breathe deeply. Check colour, consistency, and amount of any expectorant. 7. If an incentive spirometer is ordered, encourage the patient to use it every hour for 10 inspirations. If oxygen saturation or respiratory rate drops, encourage its use every 15 minutes. Cardiovascular System 1. Auscultate rhythm at apex: Is it regular or irregular? (Do not listen over the patient's gown.) 2. Check apical pulse against radial pulse, noting perfusion of all beats. 3. Assess heart sounds in all auscultatory areas: first with the diaphragm of the stethoscope and then with the bell. 4. Check capillary refill for prompt return 5. Check for pretibial edema 6. Palpate the posterior tibial and dorsalis pedis pulses in both feet. (Assess pulses in the lower extremities by Doppler technique, if not palpable.) 7. Verify that the correct IV solution is hanging and flowing at the correct rate according to both the physician's orders and your own assessment of the patient's needs. Skin 1. 2. 3. 4. Note skin colour and whether it is consistent with the patient's ethnocultural heritage. Palpate skin temperature; expect the skin to be warm and dry Pinch up a fold of skin under the clavicle or on the forearm to note mobility and turgor Note skin integrity, any lesions, and the condition of any dressings. Note any bleeding or infection, but do not change dressing until after physical examination. 5. Note the date on the IV site and the surrounding skin condition, observing for redness, edema, drainage, etc. 6. Complete any standardized scales used to quantify risk for skin breakdown 7. Verify that any air loss or alternating pressure mattresses being used are properly applied and operating at the correct settings. Abdomen 1. 2. 3. 4. 5. Assess contour of abdomen: flat, rounded, or protuberant. Listen to bowel sounds in all four quadrants. Perform light palpation in all four quadrants. Inquire whether the patient is nauseated or has vomited. Inquire whether the patient is passing flatus or stool,or experiencing constipation or diarrhea. Note date of most recent bowel movement. 6. Check any drainage tube placement for colour, consistency, odour, and amount of drainage and evaluate the integrity of the insertion site. Assess all tubes from site to source for kinks, leaks, and disconnections. 7. Check any stoma for colour, moisture, excoriation, and bleeding, and evaluate the integrity of the stomal appliance. Check stomal drainage for colour, consistency, odour, and amount. 8. Regarding diet orders, determine whether the patient is tolerating ice chips, liquids, or solids. Order the correct diet as it is advanced. Note whether the patient is at high risk for nutrition deficit. Genitourinary System 1. Inquire whether the patient is voiding regularly, or, if indicated, assess the indwelling urinary catheter and surrounding skin integrity. 2. Check urine for colour and clarity. 3. If catheter is in place, check colour, quantity, and clarity of urine with every check of vital signs. 4. If urine output is less than the expected amount, perform a bladder scan according to agency protocol. Determine whether the problem is associated with the production of urine or its retention. 5. Assess 24-hour fluid balance to identify hydration or dehydration, kidney function, and perfusion. Activity 1. Regarding activity orders, if the patient is on bed rest, the head of the bed should be angled at 15 degrees or higher. Note whether the patient is at high risk for skin breakdown. 2. If the patient is ambulatory, assist the patient to a sitting position. Assess for orthostatic hypotension and dizziness. If none, move the patient to a chair. Increase activity as tolerated. 3. Note any assistance needed, how the patient tolerates movement, distance walked to the chair, the patient's ability to turn, and whether the patient's gait is steady and symmetrical. 4. Note any need for ambulatory aid or equipment. 5. Complete any standardized scales used to quantify the patient's risk for falling and/or functional status and assess need for referral to physiotherapy or occupational therapy. 6. If antiembolism compression (T.E.D.) stockings and sequential compression devices (SCDs) are ordered, the patient needs to use them for 22 of 24 hours. SCDs must be hooked up and turned on, except during ambulation. Report Critical Findings Note examination findings that necessitate immediate attention: 1. Altered level of consciousness, confusion 2. Systolic BP less than 90 or greater than 160 mm Hg 3. Temperature greater than 38 degrees C (100.4¬∞F) 4. Heart rate <60 or greater than 100 bpm 5. Respiratory rate <10/min or greater than 28/min 6. Oxygen saturation less than 92% 7. Urine output <30 mL/hour for 2 hours 8. Dark amber urine or bloody urine (except for urology patients) 9. Postoperative nausea or vomiting not relieved with medication 10. Surgical pain not controlled with medication; any other unusual pain, such as chest pain 11. Bleeding 12. Sudden restlessness or anxiety