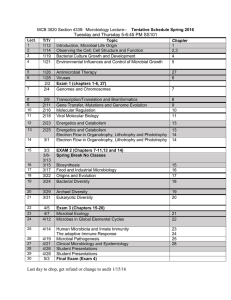
A comparison of the microbial community structure between inflamed and non-inflamed sites in patients with ulcerative colitis Running head: Dysbiosis in ulcerative colitis Atsushi Hirano (1), Junji Umeno (1), Yasuharu Okamoto (1), Hiroki Shibata (2), Yoshitoshi Ogura (3), Tomohiko Moriyama (1), Takehiro Torisu (1), Shin Fujioka (1), Yuta Fuyuno (1), Yutaka Kawarabayasi (4), Takayuki Matsumoto (5), Takanari Kitazono (1), Motohiro Esaki (1) 1. Department of Medicine and Clinical Science, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan 2. Medical Institute of Bioregulation, Kyushu University, Fukuoka, Japan 3. Department of Bacteriology, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan 4. National Institute of Advanced Industrial Science and Technology (AIST), Ibaraki, Japan 5. Division of Gastroenterology, Department of Internal Medicine, Iwate Medical University, Iwate, Japan Correspondence to: Motohiro Esaki, M.D, PhD. This article has been accepted for publication and undergone full peer review but has not been through the copyediting, typesetting, pagination and proofreading process which may lead to differences between this version and the Version of Record. Please cite this article as doi: 10.1111/jgh.14129 This article is protected by copyright. All rights reserved. Department of Medicine and Clinical Science, Graduate School of Medical Sciences, Kyushu University, Maidashi 3-1-1, Higashi-ku, Fukuoka 812-8582, Japan Phone: +81-92-642-5261; Fax: +81-92-642-5273; E-mail mesaki@intmed2.med.kyushu-u.ac.jp Financial support: This work was supported by grants awarded to AH by Mitsubishi Tanabe Pharma Corporation [grant number MTPS20160411025]. The funder had no role in study design, collection, or interpretation of data. Declaration of conflict of interest: The authors declare that there is no conflict of interest. Acknowledgments We graciously thank the patients for providing samples. Itemized list: Word count for abstract: 245 Word count for text: 2661 This article is protected by copyright. All rights reserved. Tables: 1 Figure: 5 Supplementary figure: 4 References: 38 Abstract Background and Aim: The gut microbiota is suggested to play an important role in the pathogenesis of ulcerative colitis (UC). However, inter-individual and spatial variations hamper the identification of UC-related changes. We thus investigated paired mucosa-associated microbiota obtained from both inflamed and non-inflamed sites of UC patients and corresponding sites of non-IBD controls. Methods: Mucosal biopsies of both inflamed and non-inflamed sites were obtained from 14 patients with active UC of the left-sided or proctitis type. Paired mucosal biopsies of the corresponding sites were obtained from 14 non-IBD controls. The microbial community structure was investigated using 16S rRNA gene sequences, followed by data analysis using Qiime and LEfSe software. Results: Microbial alpha diversity in both inflamed and non-inflamed sites was significantly lower in UC patients compared with non-IBD controls. There were more microbes of the genus Cloacibacterium and the Tissierellaceae family, and there were less microbes of the This article is protected by copyright. All rights reserved. genus Neisseria at the inflamed site when compared to the non-inflamed site in UC patients. Decreased abundance of the genera Prevotella, Eubacterium, Neisseria, Leptotrichia, Bilophila, Desulfovibrio, Butyricimonas was evident at the inflamed site of UC patients compared to the corresponding site of non-IBD controls. Among these taxa, the genera Prevotella and Butyricimonas were also less abundant at the non-inflamed site of UC patients compared to the corresponding site in non-IBD controls. Conclusions: Mucosal microbial dysbiosis occurs at both inflamed and non-inflamed sites in UC patients. The taxa showing altered abundance in UC patients might mediate colonic inflammation. Keywords ulcerative colitis; mucosal microbiota; dysbiosis; 16S rRNA gene sequence Author contributions AH, JU, TK and ME conceived and designed this study. AH, JU, YO, TM, TT, SF, YF and ME collected and processed mucosal biopsies. AH and HS performed the experiments. AH, JU, HS and YO analyzed and interpreted the data. AH, YK, TM and ME drafted the manuscript. All authors approved the final version. This article is protected by copyright. All rights reserved. Introduction Ulcerative colitis (UC) and Crohn’s disease (CD) are the two principal forms of inflammatory bowel disease (IBD). Although their etiology remains uncertain, complex interactions between genetic susceptibility and environmental factors are considered to play a role in the pathogenesis of IBD. An imbalance in the composition of the microbial population has been proposed to be one of the most important environmental factors, and considerable efforts have been focused on the identification of the microbial taxa that are associated with gut inflammation. Culture-independent techniques, which can identify bacteria on the basis of the nucleic acid sequence of 16SrRNA molecules 1, have recently revolutionized the understanding of the complex intestinal bacterial ecology associated with various diseases 2 3. The dysbiosis characterized by a decreased abundance of Firmicutes, particularly of Clostridium cluster IV or the enrichment of species belonging to the Enterobacteriaceae family containing adherent invasive Escherichia coli (AIEC) occurs in CD4 5. In contrast, associations between changes in the microbial population and UC are still inconsistent, suggesting that dysbiosis might be less important for UC than CD 6. However, because the genetics have been shown to contribute little to the etiology of UC when compared to CD in twin studies 7, environmental triggers, including dysbiosis, are more likely to play important roles in the pathogenesis of UC. This article is protected by copyright. All rights reserved. Faecal samples have been used to investigate the microbial population in the majority of previous studies. However, mounting evidence has indicated that the faecal microbiota is distinct from the mucosa-associated microbiota 8 9. Because the mucosa-associated microbiota shows intimate contact with the host, it is more likely to induce direct immune responses than luminal microbiota does10. Therefore, mucosal samples may be more appropriate for the identification of the microbiota associated with mucosal inflammation. Moreover, paired mucosal sampling from inflamed and non-inflamed sites in UC patients is a valid approach to minimize the effects of inter-individual variation in the microbial population. Studies of this type were carried out prior to the era of next-generation sequencing technology, but those studies utilized relatively low-resolution methods, such as temporal temperature-gradient gel electrophoresis (TTGE) 11, denaturing gradient gel electrophoresis (DGGE) 12 or sequencing by capillary electrophoresis 13 14 for the determination of the microbial population. Forbes et al. recently analysed differences in the bacterial population between inflamed and non-inflamed sites using next-generation sequencer. However, the results could have been influenced by inter-individual and spatial variations, because 3–4 mucosal samples were collected from various colonic sites in each UC patient 15. In the present study, paired mucosal samples were collected unequivocally from inflamed rectal mucosa and non-inflamed transverse colonic mucosa in UC patients. We This article is protected by copyright. All rights reserved. believe that such samplings contribute to the characterization of the microbial population that associates with colonic inflammation in UC. In addition, paired mucosal samples were also collected from non-IBD controls, and microbial population at the corresponding sites were compared between UC patients and non-IBD controls. With the analysis, site specific difference of microbial population between UC patients and non-IBD controls could be determined, while mucosa-associated microbiota has been reported to be mostly homogenous throughout the colorectum9. Using these specimens, we analysed the microbial community structure by 16S rRNA gene sequencing with next-generation sequencer. Methods Subjects Fourteen patients with active UC of the left-sided type or proctitis type, and 14 individuals without inflammatory bowel disease (non-IBD controls), who underwent colonoscopy for polyp surveillance, were enrolled in the present study. If an adenoma larger than 1 cm, cancer or inflammation were detected during surveillance colonoscopy of non-IBD control patients, these individuals were excluded from the study. All the participants were Japanese and none were related to each other. No individual had received antibiotics during the preceding 2 months. This article is protected by copyright. All rights reserved. Sample collection Before colonoscopy, patients received standard bowel preparation using 2L of lavage solution (NIFLEC®; EA Pharma Co., Tokyo,Japan). During colonoscopy, tissue samples were obtained from the transverse colon and the rectum in each subject using disposable biopsy forceps (Olympus, Tokyo, Japan) after washing the colorectal mucosa gently with tap water containing dimethicone solution. Bioptic forceps were also rinsed with tap water before taking each bioptic sample. Based on the disease types of UC patients in the present study, the transverse colon was regarded as the ‘non-inflamed’ site and the rectum was regarded as the ‘inflamed’ site in UC patients (see Supplementary Figure 1). Mucosal biopsy samples were stored at -80°C until extraction of DNA. DNA extraction and 16S Ribosomal RNA Gene Sequencing Mucosal bacterial DNA was extracted from mucosal samples using NucleoSpin® Tissue XS (Macherey-Nagel, Düren, Germany) and 5 mm stainless steel beads in a Tissue lyser (Qiagen Inc. CA, USA) vibrating at 25 times/sec for 1 min. Subsequently, 16S rRNA gene sequencing was conducted as described previously with minor modifications 16. Briefly, the extracted bacterial DNA was used as the template to amplify the V4 region of each 16S This article is protected by copyright. All rights reserved. rRNA gene using the primer pair 515F/806R, which included the Illumina Flowcell adapter sequences. The reverse primer also contained a 12 bases barcode sequence. Paired-end sequencing of the PCR amplicons was performed on the Illumina MiSeq platform (Illumina Inc. CA, USA) using custom primers. Bioinformatics and Statistical analysis Raw Illumina fastq files were demultiplexed, quality filtered, and analysed using QIIME v 1.9.1 software 17. The 16S rRNA operational taxonomic units (OTUs) were clustered using “open-reference OTU” of QIIME. In this open-reference OTU picking process, reads were firstly clustered against a Greengenes 13_8 reference 18 using closed-reference OTUs picking. Subsequently, 0.1% of the reads which failed to hit the reference sequence collection were randomly subsampled and clustered de novo using UCLUST 19, with an OTU cluster defined by a sequence similarity of 97%. ChimeraSlayer was employed to remove chimeric sequences 20. Alpha diversity (microbial diversity within samples) was calculated using Observed Species, Phylogenetic Diversity (PD) Whole Tree and Chao1. OTUs were rarefied at a depth of 5,500 sequences, and subsampling was performed 10 times. The measured alpha diversities were compared between each group using a non-parametric two sample t-test and the default number of Monte Carlo This article is protected by copyright. All rights reserved. permutations (999). Principal Coordinate Analysis (PCoA), based on the weighted UniFrac distances, was used to evaluate beta diversity (community diversity between samples). The significance of the distance between two groups was calculated by non-parametric MANOVA. We used linear discriminant analysis (LDA) effect size (LEfSe) 21, which is an algorithm used to discover high-dimensional biomarkers characterizing the differences between biological conditions, to identify taxa that differed consistently between sample types. LEfSe employs the non-parametric factorial Kruskal-Wallis (KS) sum-rank test (α=0.05) to identify taxa with significantly different abundances between categories, followed by LDA to estimate the effect size of each feature of the differential abundance. We regarded differences in abundance as statistically significant when the logarithmic LDA score was > 2.0. Significant taxa were used to generate taxonomic cladograms illustrating differences between sample classes in the Galaxy framework (http://huttenhower.sph.harvard.edu/galaxy) 22. If multiple varieties with different ranks showed significance in the same taxon, the lowest-ranked varieties were regarded as responsible. This article is protected by copyright. All rights reserved. Ethical considerations The present study was conducted in accordance with the Declaration of Helsinki. The protocol was approved by the Ethical Committee of Kyushu University (approval number: 27-176), and written informed consent was obtained from all participants. Results Fifty-six mucosal samples were collected from 28 participants, including paired samples from 14 patients with active UC and 14 non-IBD controls. The clinical characteristics of the participants are listed in Table1. Most of the UC patients exhibited the left-sided type, and their endoscopic findings were classified as mild to moderately active. Mesalazine was administered to 13 UC patients and probiotics were administered to 10 UC patients. Three UC patients and two non-IBD controls were taking proton pump inhibitor. While no UC patient experienced abdominal surgery, two non-IBD controls experienced appendectomy. A total of 2,732,338 quality-filtered sequences were obtained from the samples, with a mean of 48,791±32,360 (standard deviation; SD) sequences per sample. The filtered data were assigned to 11 bacterial phyla. The most diverse phylum was Firmicutes, followed by Bacteroidetes and Proteobacteria, and the rank order of abundance of these three phyla in the four sample groups (transverse colon and rectum of UC patients and non-IBD controls) was similar (see Supplementary Figure 2). This article is protected by copyright. All rights reserved. Comparison of alpha and beta diversity according to colonic site and disease status The alpha diversities expressed as observed species index were significantly lower in both the transverse colon (non-inflamed site) and the rectum (inflamed site) of UC patients compared with those of non-IBD controls (Figure 1). Other indices of alpha diversity (PD Whole Tree, Chao1) showed similar trends (see Supplementary Figure 3). These results indicate that the mucosal microbial diversities of UC patients were lower in both non-inflamed and inflamed sites. No apparent clustering was observed in PCoA using the beta diversity metrics of weighted UniFrac between the transverse colon and the rectum of both UC patients and non-IBD controls (Figure 2 a, b). Conversely, the composition of the bacterial populations tended to be different between UC and non-IBD controls in both the transverse colon (p=0.18) and rectum (p=0.12) (non-parametric MANOVA), although the differences did not reach statistical significance (Figure 2 c, d). This article is protected by copyright. All rights reserved. Comparison of taxonomic composition according to biopsy site in UC patients and non-IBD controls When the taxonomic composition was compared between the rectum (inflamed site) and the transverse colon (non-inflamed site) of UC patients using LEfSe, the abundances of the genus Cloacibacterium and the Tissierellaceae family were significantly greater at the inflamed site compared to the non-inflamed site. In contrast, the abundance of the genus Neisseria was lower at the inflamed site than the non-inflamed site (Figure 3). However, no significant difference was observed in taxonomic composition between the transverse colon and the rectum among non-IBD controls. Comparison of taxonomic composition between UC patients and non-IBD controls When the taxonomic composition of microbiota in the rectum of UC patients and non-IBD controls was compared, the abundance of the genera Prevotella, Eubacterium, Neisseria, Leptotrichia, Bilophila, Desulfovibrio, and Butyricimonas was lower in UC patients than non-IBD controls (Figure 4). Conversely, only the abundance of the Bifidobacterium genus was greater in UC patients than non-IBD controls. When the taxonomic composition of microbiota in the transverse colon was compared between UC patients and non-IBD controls, the abundance of the genera Prevotella and Butyricimonas was significantly lower in UC patients than non-IBD controls (Figure 5). This article is protected by copyright. All rights reserved. Thus, the abundance of the genera Prevotella and Butyricimonas was lower in both the non-inflamed and inflamed sites of UC patients. Discussion In this study, we have demonstrated decreased alpha diversity in both inflamed and non-inflamed sites of UC patients compared to non-IBD controls, indicating that dysbiosis was present not only at inflamed sites but also at non-inflamed sites in UC patients. The strength of the present study is that we were able to compare the microbiota between inflamed and non-inflamed sites by paired mucosal sampling in patients with UC. Moreover, we compared the mucosal microbiota at each site between UC patients and non-IBD controls. By using these sampling, we could minimize inter-individual and spatial variations in mucosal microbiota. Consistent with the finding of the previous study 9, the populations of mucosal microbiota in the present study were roughly similar between the transverse colon and rectum. However, there was a trend towards a larger alpha diversity in the rectum compared to the transverse colon in both UC patients and non-IBD controls (see Supplementary Figure 4). This result strongly suggests the necessity of a comparison of mucosal samples obtained from the identical sites between UC patients and non-IBD controls to avoid the confounding effect of spatial variation and to detect site-specific differences in the microbial populations of the This article is protected by copyright. All rights reserved. large bowel. With regard to specific taxa in UC, greater abundance of the Cloacibacterium and Tissierellaceae were found at the inflamed site compared to the non-inflamed site. Cloacibacteria are Gram-negative bacteria that were first identified in untreated human wastewater 23. Furthermore, their greater abundance in the submucosal tissues was found in patients with Crohn's disease 24. Tissierellaceae have recently been identified within the phylum Firmicutes by reconstruction of high-rank 16S rRNA gene-based phylogenies 25, and they have been shown to be more abundant in patients with Parkinson’s disease 26. Considering the difference in their abundance among inflamed and non-inflamed sites in UC and their presence in non-IBD controls, these taxa may act as pro-inflammatory property when microbial diversity is low. Further investigation using animal models is necessary to determine whether these bacteria can actually induce colonic inflammation under specific conditions. In the present study, the abundance of the genera Eubacterium, Butyricimonas, Prevotella, Neisseria, Leptotrichia, Bilophila and Desulfovibrio was lower at the inflamed site in UC compared to the corresponding site in non-IBD controls. In addition, the abundance of the Prevotella and Butyricimonas was also lower at the non-inflamed site of UC compared to the corresponding site in non-IBD controls. Among those species, Eubacterium is categorized in cluster XIVa of the Clostridia, which have recently gained a lot This article is protected by copyright. All rights reserved. of attentions because of their anti-inflammatory properties mediated by induction of regulatory T-cells 27. Recently, the lower abundance of Eubacterium has also been shown in UC patients 28 29. A lower abundance of Butyricimonas with a negative correlation with pro-inflammatory cytokines, has recently been reported in patients with multiple sclerosis 30. In addition, Prevotella, which showed the greatest difference at both the inflamed and non-inflamed sites of UC from non-IBD controls in the present study, was reported to be less abundant in untreated multiple sclerosis patients, while this difference was ameliorated after the treatment 30. Although the potential influence of Prevotella on gut inflammation has not been fully investigated, the “Prevotella enterotype” is known to be associated with non-Western rural communities, where residents consume a plant-based diet rich in polysaccharides and fibre known to be protective against inflammation 31 32. Therefore, Prevotella provisionally plays a protective role against gut inflammation. Neisseria is considered to an orally resident microbe, with the exception of the pathogenic N. gonorrhoeae and N. meningitides species. In a previous study of the salivary microbiota in IBD patients, Neisseria was less abundant in patients with CD and UC when compared to controls 33. Given the association between the lower abundance of specific taxa and proinflammatory conditions in the present study, such taxa could play an important role in maintaining microbial homeostasis. Bilophila and Desulfovibrio have been shown to be involved in inflammation, This article is protected by copyright. All rights reserved. including UC 34 35. Leptotrichia are commensal oral and female genital bacteria, and are considered not typical of pathognomonic property 36, while invasive Leptotrichia infections have been reported in immunosuppressed patients. However, further investigation of the association of these taxa with UC is necessary. The present study has some limitations. First, most UC patients were taking probiotics (Table 1), because a possible beneficial effect on UC has been suggested 37. Consequently, the abundance of the Bifidobacteria was greater in UC patients than non-IBD controls, which was the opposite trend to that observed in a previous study38. Thus, the probiotics might have influenced the results of the present study to some degree. Second, possible bacterial contamination through the endoscopy channel needs to be considered. However, mucosal samples were collected using biopsy forceps. Therefore, biopsy samples were considered to be less susceptible to contamination, because tissue samples were covered by biopsy forceps during the procedure of sample collection. Third, because the present study included a small sample size, it is necessary to validate our observations in a larger cohort free from the use of probiotics. In conclusion, the present study demonstrated a disturbed mucosa-associated microbial population at the inflamed and the non-inflamed site of UC patients. Moreover, we identified two taxa with greater abundance at the inflamed site of UC by comparing the results with the non-inflamed site of UC patients, and also seven genera that were less This article is protected by copyright. All rights reserved. abundant at the inflamed site when compared to non-IBD controls. In addition, the genera Prevotella and Butyricimonas were significantly less abundant at both the inflamed and non-inflamed sites of the UC patients, suggesting that they may play an important role in the pathogenesis of UC. References 1. Andersson AF, Lindberg M, Jakobsson H, Backhed F, Nyren P, Engstrand L. Comparative analysis of human gut microbiota by barcoded pyrosequencing. PLoS One. 2008; 3: e2836. 2. Lynch SV, Pedersen O. The Human Intestinal Microbiome in Health and Disease. N Engl J Med. 2016; 375: 2369-79. 3. Sartor RB, Wu GD. Roles for Intestinal Bacteria, Viruses, and Fungi in Pathogenesis of Inflammatory Bowel Diseases and Therapeutic Approaches. Gastroenterology. 2017; 152: 327-39 e4. 4. Kostic AD, Xavier RJ, Gevers D. The microbiome in inflammatory bowel disease: current status and the future ahead. Gastroenterology. 2014; 146: 1489-99. 5. Becker C, Neurath MF, Wirtz S. The Intestinal Microbiota in Inflammatory Bowel Disease. ILAR J. 2015; 56: 192-204. 6. Pascal V, Pozuelo M, Borruel N, et al. A microbial signature for Crohn's disease. Gut. This article is protected by copyright. All rights reserved. 2017; 66: 813-22. 7. Halfvarson J, Bodin L, Tysk C, Lindberg E, Järnerot G. Inflammatory bowel disease in a Swedish twin cohort: a long-term follow-up of concordance and clinical characteristics. Gastroenterology. 2003; 124: 1767-73. 8. Momozawa Y, Deffontaine V, Louis E, Medrano JF. Characterization of bacteria in biopsies of colon and stools by high throughput sequencing of the V2 region of bacterial 16S rRNA gene in human. PLoS One. 2011; 6: e16952. 9. Lavelle A, Lennon G, O'Sullivan O, et al. Spatial variation of the colonic microbiota in patients with ulcerative colitis and control volunteers. Gut. 2015; 64: 1553-61. 10. Sartor RB. Gut microbiota: Optimal sampling of the intestinal microbiota for research. Nat Rev Gastroenterol Hepatol. 2015; 12: 253-4. 11. Sepehri S, Kotlowski R, Bernstein CN, Krause DO. Microbial diversity of inflamed and noninflamed gut biopsy tissues in inflammatory bowel disease. Inflamm Bowel Dis. 2007; 13: 675-83. 12. Bibiloni R, Mangold M, Madsen KL, Fedorak RN, Tannock GW. The bacteriology of biopsies differs between newly diagnosed, untreated, Crohn's disease and ulcerative colitis patients. J Med Microbiol. 2006; 55: 1141-9. 13. Gophna U, Sommerfeld K, Gophna S, Doolittle WF, Veldhuyzen van Zanten SJ. Differences between tissue-associated intestinal microfloras of patients with Crohn's disease This article is protected by copyright. All rights reserved. and ulcerative colitis. J Clin Microbiol. 2006; 44: 4136-41. 14. Walker AW, Sanderson JD, Churcher C, et al. High-throughput clone library analysis of the mucosa-associated microbiota reveals dysbiosis and differences between inflamed and non-inflamed regions of the intestine in inflammatory bowel disease. BMC Microbiol. 2011; 11: 7. 15. Forbes JD, Van Domselaar G, Bernstein CN. Microbiome Survey of the Inflamed and Noninflamed Gut at Different Compartments Within the Gastrointestinal Tract of Inflammatory Bowel Disease Patients. Inflamm Bowel Dis. 2016; 22: 817-25. 16. Caporaso JG, Lauber CL, Walters WA, et al. Ultra-high-throughput microbial community analysis on the Illumina HiSeq and MiSeq platforms. ISME J. 2012; 6: 1621-4. 17. Caporaso JG, Kuczynski J, Stombaugh J, et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods. 2010; 7: 335-6. 18. DeSantis TZ, Hugenholtz P, Larsen N, et al. Greengenes, a chimera-checked 16S rRNA gene database and workbench compatible with ARB. Appl Environ Microbiol. 2006; 72: 5069-72. 19. Edgar RC. Search and clustering orders of magnitude faster than BLAST. Bioinformatics. 2010; 26: 2460-1. 20. Haas BJ, Gevers D, Earl AM, et al. Chimeric 16S rRNA sequence formation and This article is protected by copyright. All rights reserved. detection in Sanger and 454-pyrosequenced PCR amplicons. Genome Res. 2011; 21: 494-504. 21. Segata N, Izard J, Waldron L, et al. Metagenomic biomarker discovery and explanation. Genome Biol. 2011; 12: R60. 22. Afgan E, Baker D, van den Beek M, et al. The Galaxy platform for accessible, reproducible and collaborative biomedical analyses: 2016 update. Nucleic Acids Res. 2016; 44: W3-W10. 23. Allen TD, Lawson PA, Collins MD, Falsen E, Tanner RS. Cloacibacterium normanense gen. nov., sp. nov., a novel bacterium in the family Flavobacteriaceae isolated from municipal wastewater. Int J Syst Evol Microbiol. 2006; 56: 1311-6. 24. Chiodini RJ, Dowd SE, Chamberlin WM, Galandiuk S, Davis B, Glassing A. Microbial Population Differentials between Mucosal and Submucosal Intestinal Tissues in Advanced Crohn's Disease of the Ileum. PLoS One. 2015; 10: e0134382. 25. Alauzet C, Marchandin H, Courtin P, et al. Multilocus analysis reveals diversity in the genus Tissierella: description of Tissierella carlieri sp. nov. in the new class Tissierellia classis nov. Syst Appl Microbiol. 2014; 37: 23-34. 26. Hill-Burns EM, Debelius JW, Morton JT, et al. Parkinson's disease and Parkinson's disease medications have distinct signatures of the gut microbiome. Mov Disord. 2017. 27. Atarashi K, Tanoue T, Oshima K, et al. Treg induction by a rationally selected mixture of This article is protected by copyright. All rights reserved. Clostridia strains from the human microbiota. Nature. 2013; 500: 232-6. 28. Vermeiren J, Van den Abbeele P, Laukens D, et al. Decreased colonization of fecal Clostridium coccoides/Eubacterium rectale species from ulcerative colitis patients in an in vitro dynamic gut model with mucin environment. FEMS Microbiol Ecol. 2012; 79: 685-96. 29. Knoll RL, Forslund K, Kultima JR, et al. Gut microbiota differs between children with Inflammatory Bowel Disease and healthy siblings in taxonomic and functional composition: a metagenomic analysis. Am J Physiol Gastrointest Liver Physiol. 2017; 312: G327-G39. 30. Jangi S, Gandhi R, Cox LM, et al. Alterations of the human gut microbiome in multiple sclerosis. Nat Commun. 2016; 7: 12015. 31. De Filippo C, Cavalieri D, Di Paola M, et al. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc Natl Acad Sci U S A. 2010; 107: 14691-6. 32. Wu GD, Chen J, Hoffmann C, et al. Linking long-term dietary patterns with gut microbial enterotypes. Science. 2011; 334: 105-8. 33. Said HS, Suda W, Nakagome S, et al. Dysbiosis of salivary microbiota in inflammatory bowel disease and its association with oral immunological biomarkers. DNA Res. 2014; 21: 15-25. 34. David LA, Maurice CF, Carmody RN, et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014; 505: 559-63. This article is protected by copyright. All rights reserved. 35. Earley H, Lennon G, Balfe A, et al. A Preliminary Study Examining the Binding Capacity of Akkermansia muciniphila and Desulfovibrio spp., to Colonic Mucin in Health and Ulcerative Colitis. PLoS One. 2015; 10: e0135280. 36. Couturier MR, Slechta ES, Goulston C, Fisher MA, Hanson KE. Leptotrichia bacteremia in patients receiving high-dose chemotherapy. J Clin Microbiol. 2012; 50: 1228-32. 37. Kato K, Mizuno S, Umesaki Y, et al. Randomized placebo-controlled trial assessing the effect of bifidobacteria-fermented milk on active ulcerative colitis. Aliment Pharmacol Ther 2004;20:1133-41. 38. Mylonaki M, Rayment NB, Rampton DS, Hudspith BN, Brostoff J. Molecular characterization of rectal mucosa-associated bacterial flora in inflammatory bowel disease. Inflamm Bowel Dis 2005;11:481-7. This article is protected by copyright. All rights reserved. Figure 1 Comparison of alpha diversity index between ulcerative colitis (UC) patients and individuals without inflammatory bowel disease. An alpha diversity index expressed as the observed species was compared between UC patients (n=14) and individuals without inflammatory bowel disease (non-IBD controls) (n=14) in the transverse colon (a, b), and rectum (c, d). Rarefaction curves show the observed species at various sequencing depths (a, c), and boxplots show these at higher sequencing depth (5500 reads per sample). The alpha diversities of UC patients were significantly lower in both the transverse colon and rectum. This article is protected by copyright. All rights reserved. Figure 2 Comparison of microbial diversity clustering between anatomical sites and patient groups. Principal Coordinate Analysis (PCoA) using the beta diversity metrics of weighted UniFrac within UC patients (a), non-IBD controls (b), transverse colon (c), and rectum (d), respectively. The P value was calculated using non-parametric MANOVA. There were no apparent differences in the composition of the microbial population between the transverse colon and rectum in both UC patients and non-IBD controls (a, b). Conversely, the composition of the microbial population tended to be phenotypically different between UC and non-IBD controls in both the transverse colon and rectum, although these differences did not reach statistical significance. This article is protected by copyright. All rights reserved. Figure 3 Comparison of the taxonomic composition of the microbiome in the transverse colon and rectum of ulcerative colitis patients. The cladogram and bar graph indicate the taxa that discriminate between transverse colon (non-inflamed site) and rectum (inflamed site) of UC patients, based on LEfSe method and LDA analysis. If multiple varieties with different ranks showed significance in the same taxon, the lowest-ranked varieties were regarded to be responsible. While the abundance of the genus Cloacibacterium and the Tissierellaceae family was greater in the rectum, the abundance of the genus Neisseria was lower. This article is protected by copyright. All rights reserved. Figure 4 Comparison of the taxonomic composition of the microbiome in the rectum of ulcerative colitis patients and controls. The cladogram and bar graph indicate the taxa that discriminate between UC patients and non-IBD controls in the rectum. If multiple varieties with different ranks showed significance in the same taxon, the lowest-ranked varieties were regarded to be responsible. The This article is protected by copyright. All rights reserved. abundance of the genera Prevotella, Eubacterium, Neisseria, Leptotrichia, Bilophila, Desulfovibrio, and Butyricimonas was lower in UC patients compared to non-IBD controls. Conversely, the abundance of the genus Bifidobacterium was greater in UC patients. This article is protected by copyright. All rights reserved. Figure 5 Comparison of the taxonomic composition of the microbiome in the transverse colon of ulcerative colitis patients and controls. The cladogram and bar graph indicate the taxa that discriminate between UC patients and non-IBD controls in the transverse colon. If multiple varieties with different ranks showed significance in the same taxon, the lowest-ranked varieties were regarded to be responsible. The abundance of the genera Prevotella and Butyricimonas was lower in UC patients compared to non-IBD controls. This article is protected by copyright. All rights reserved. Table1. The clinical characteristics of participants UC patients (n=14) Non-IBD controls (n=14) 6/8 44.5 (17-67) 9 (1-30) 8/6 58.5 (41-73) - 13 1 - Mayo endoscopic subscore 1 2 3 8 5 1 - Concomitant drugs (n) Mesalazine Corticosteroids(oral/local) Probiotics Thiopurines Tacrolimus 13 4/3 10 3 1 - 3 1 3 0 2 2 Gender (male/female) Age (years) Disease duration (years) Ulcerative colitis extension Left-sided Proctitis Infliximab Adalimumab Proton pump inhibitor History of abdominal surgery This article is protected by copyright. All rights reserved.