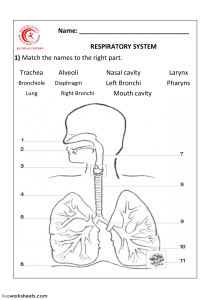
Homeostasis and Organ Systems Case 4: Bigger is better? Learning Goals: 1. 2. 3. 4. Anatomy of the respiratory system Function of the respiratory system Connection between respiratory- and nervous system Describe respiratory cycle/breathing - Lung capacity - Active/passive breathing 5. What determines optimal ventilation - Fick’s Law 6. How do you measure lung capacity? - What affects lung capacity? Anatomy of the respiratory system Nasal cavity Cells release mucus (salty, sticky, contains lysosomes) kills bacteria Nose hairs coated with mucus Trap larger particles and bacteria Paranasal sinuses: - Frontal - Ethmoid - Sphenoid - Maxillary Air filled spaces; help air get warm and moist; amplify sound. Pharynx (throat) Nasopharynx Connecting nasal cavity and pharynx - soft palate & Uvula form a valve → closes off nasopharynx when swallowing, preventing food from entering Oropharynx Connecting oral cavity and pharynx Laryngopharynx Continuous with larynx Larynx Epiglottis Seals of airway when eating, preventing food from entering. Trachea (windpipe) Descends from the larynx through the neck and into the mediastinum. It ends by dividing into the two main bronchi. The point at which they split is called the carina. The trachea uses cartilage rings for support. Since the lungs create negative pressure with every breath, the trachea needs those rings to keep it open. Wall composition: - Mucosa Pseudostratified columnar ciliated epithelium. - Submucosa Elastic fibers, fat cells tubular glands - Musculo cartilaginous Cartilaginous plates, fibroelastic tissue, smooth muscle. - Adventitia Connective tissue layer The trachea also has a layer of smooth muscle cells which has nerves of the autonomic nervous system within it. Smooth muscle along the trachea and the first few branches of bronchi have β2 adrenergic receptors and muscarine receptors, which can get stimulated by the ortho-, or parasympathetic nervous system. Bronchi The trachea divides to form the right and left main (primary) bronchi. The right main bronchus is wider, shorter, and more vertical than the left It is more common for an inhaled foreign object to get stuck there Once inside the lungs Each main bronchus subdivides into lobar (secondary) bronchi Three on the right and two on the left The lobar bronchi branch into divide into smaller and smaller bronchi Eventually into bronchioles (diameter <1mm) and terminal bronchioles (diameter <0,5mm) And lastly into respiratory bronchioles Wall composition: - Irregular plates of cartilage replace the cartilage rings. - By the time the bronchioles are reached the tube walls no longer contain supportive cartilage. - The mucosal epithelium thins as it changes from pseudostratified columnar columnar cuboidal in the terminal bronchioles. - The relative amount of smooth muscle in the tube walls increases as the passageways become smaller. Alveoli The respiratory bronchioles Alveolar ducts Terminal clusters of alveoli called alveolar sacs or alveolar saccules. Walls of alveolar ducts consist of diffusely arranged rings of smooth muscle cells, connective tissue fibers and out pocketing alveoli. Alveoli composition: - The walls of the alveoli are composed primarily of a single layer of squamous epithelial cells type I alveolar cells surrounded by a flimsy basement membrane. - The external surfaces of the alveoli are densely covered with a “cobweb” of pulmonary capillaries. - The capillary and alveolar walls and their fused basement membranes form the respiratory membrane a 0.5-μm-thick blood air barrier. - Blood flows past one side and gas on the other of the barrier - Gas exchanges occur readily by simple diffusion across the respiratory membrane. - Scattered amid the squamous type I alveolar cells that form the major part of the alveolar walls are cuboidal type II alveolar cells. - Type II alveolar cells Secrete a fluid containing a detergent-like substance called surfactant that coats the gas-exposed alveolar surfaces. (Role in reducing the surface tension of the alveolar fluid) - Type II alveolar cells also secrete several antimicrobial proteins that are important elements of innate immunity. The alveoli have 2 other significant features: 1. Open alveolar pores connecting adjacent alveoli allow air pressure throughout the lungs to be equalized and provide alternate air routes to any alveoli whose bronchi have collapsed due to disease. 2. Remarkably efficient alveolar macrophages crawl freely along the internal alveolar surfaces. Although huge numbers of infectious microorganisms are continuously carried into the alveoli, alveolar surfaces are usually sterile. Lungs (and Pleurae) The paired lungs occupy all the thoracic cavity except the mediastinum (Houses the heart, great blood vessels, bronchi, esophagus, and other organs). Left lung Long and narrow Is subdivided into superior and inferior lobes by the oblique fissure. Right lung Short and wide Is partitioned into superior, middle, and inferior lobes by the oblique and horizontal fissures Innervation: The lungs are innervated by parasympathetic and sympathetic motor fibers, and visceral sensory fibers. These nerve fibers enter each lung through the pulmonary plexus on the lung root and run along the bronchial tubes and blood vessels in the lungs. The pleurae Fluid-secreting membrane that folds in half around each of the lungs, forming a separation between the lungs and the chest cavity. The part of the folded membrane that borders the lungs is called the pleurae pulmonalis. The part on the outside, which therefore borders the chest cavity, is called the pleurae parietalis. Between these two membranes is an interspace, the pleural space, which is filled with a thin film of pleural fluid, which allows the membranes to move past each other during breathing. Diaphragm (and Intercostal muscles) Lungs don't have any contractible muscle tissue. To be able to expand The diaphragm, a thin set of muscles (only where it is attached to your lower ribs; the middle is tendon) that separates your thorax from your abdomen. Direction of the external intercostal muscles: outside to inside (shoulder to hip) Direction of the internal intercostal muscles: inside to outside (trachea to hip) Function of the respiratory system 1. 2. 3. 4. Respiration (exchange of O2 and CO2) Vocalization Maintaining pH Smelling and tasting Respiratory- and nervous system Breathing cycle The atmospheric pressure (Patm) The pressure exerted by the air (gases) surrounding the body. The intrapulmonary pressure (Ppul) The pressure inside the lungs. The intrapleural pressure (Pip) The pressure in the pleural cavity. The transpulmonary pressure Ppul – Pip When Pip > Ppul Lungs collapse Voluntary and involuntary Breathing Voluntary breathing By cerebral cortex Involuntary breathing By Respiratory centers in the brainstem The breathing cycle is controlled by the respiratory centre located inside the medulla and the pons of the brain stem. Three major collections of neurons form this centre: - The dorsal respiratory group Responsible for the largest part of the breathing cycle. - The ventral respiratory group Plays a role in forced expiration. - The pneumotaxic centre Controls the rate and depth of breathing. Pre-Botzinger complex (pacemaker cells) Generate rhythm of respiration To initiate breathing The dorsal respiratory group sends impulses Activate motor neurons in cervical and thoracic spinal cord Send impulses through the phrenic nerve towards the diaphragm and through the intercostal nerves towards the external intercostal muscles. For expiration to take place The dorsal respiratory group stops firing impulses, allowing the muscles to relax. (Expiration mainly by elasticity of the lungs) When forced expiration is needed Impulses from the respiratory group reaches the ventral group, activating it. In turn, this group initiates impulses, which reach the rectus abdominis through the thoracoabdominal nerves and the internal intercostals through the intercostal nerves. The efficiency of gas exchange across a surface is determined by Fick's Law. Fick's Law states that, for the diffusion of a gas to be efficient, three conditions should be met. Firstly, the surface area of the diffusion pathway should be large. Secondly, there should be large difference in concentration between the area the gas is diffusion to, and the area it is diffusing from. Finally, the diffusion pathway should be short. The alveoli allow all three of these conditions to be met, allowing efficient gas exhange within the lungs. There are around 350 million alveoli on each lung, creating a very large surface area for diffusion to take place across. Alveolar cells are specially adapted to create a short diffusion pathway to the blood capillary network. They are flattened, single-celled epithelia, meaning there is only a small area of cytoplasm for gases to diffuse through before they reached the blood capillary epithelia. Finally, a large concentration gradient is created between the alveoli and the capillaries through the removal of oxygenated blood, which is replaced with oxygenated blood. This creates a well-ventilated gas exchange surface.