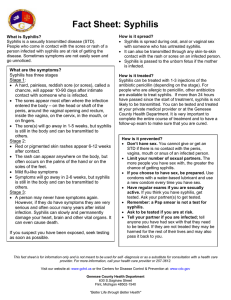
Case rates of syphilis have increased over the past decade across the United States. According to data from the San Bernardino County case rates across the US have roughly doubled over the five-year period between 2013 and 2018. Over that same period, in San Bernardino County, the case rates have increased from 3.6 cases per 100,000 residents to 14.6 cases per 100,000. The case rate of San Bernardino County is not as high as the California average; however, the steep rise of the curve requires attention. Even more concerning to some is the steep increase in cases of congenital syphilis. According to the SBC data that rates of congenital syphilis increased from 13.1 per 100,000 in 2015 to 99.9 in 2017 and in 2018. 1 Syphilis refers to an infection caused by a spirochaete bacterium called Treponema pallidum, of which there are 3 subspecies.2 The bacterium is primarily spread through oral, anal, and vaginal intercourse. However, it can also be transmitted through contaminated blood and congenitally from the mother to her unborn child. The bacterium cannot survive outside of the host so inoculation from contact with objects within the environment, which is a concern for some other types of infections.3 Syphilis is spread during sexual contact from the syphilitic core or chancre, which is typically a painless ulcer in the skin. This chancre can be visible on the exterior of the genitalia/mouth or internal and therefore not visible.4 Syphilis can also be spread during the latent stage, where there are no symptoms. The range of health hazards stemming from a syphilis infection are broad because it can affect many organ systems, including, but not limit to, the eyes, ears, skin, central nervous system, and the cardiovascular system. The primary syphilis stage is indicated by a painless ulcer in the skin at the site where the spirochaete burrowed into the skin. Secondary syphilis occurs later in the infection and typically causes a diffuse body rash. Syphilis can progress to Tertiary syphilis and Neurosyphilis which can cause permanent neurological deficits or death. Syphilis can affect the ocular system leading to permanent blindness and it can even cause aortic aneurysms. Congenital syphilis infections can be fatal in utero. If the child survives, congenital syphilis causes a wide range of permanent defects.4 Anyone who is sexually active is at risk of contracting syphilis. This risk increases in those who have multiple sexual partners, have unprotected intercourse, perform sexual acts for money, engage in same sex practices, incarcerated individuals and those who inject IV drugs. Anyone who is at risk for contracting syphilis is a stakeholder. Healthcare providers including primary care physicians, nurses, pediatricians, infectious disease specialists, obstetricians, gynecologists, neurologists, cardiologists, and geriatricians are all stakeholders. Organizations that support reproductive health such as our public health systems and Planned Parenthood are also invested in this problem. Lastly, organizations that help vulnerable populations like homeless shelters, substance use programs and treatment centers should also have a vested interest. If oral or sexual intercourse is performed the only reliable way of reducing the spread of infection is with external or internal condoms. These condoms would be considered, personal protective equipment (PPE) and would be individual controls. Contraceptive pills, rings, IUDs, or implantable devices do not protect against the spread of syphilis. Similarly, internal diaphragms or withdrawing prior to ejaculation do not protect against syphilis. Correct and consistent condom can reduce the risk of transmission; however, it does not eliminate the risk. Syphilis chancroids can be present in an area of skin that is not covered by the condom. Condoms can also fail (slip or break) even with correct and consistent use. Condoms can also have manufacturing defects decreasing effectiveness.5 This form of PPE is overall very inexpensive, especially when compared to testing and treatment, however it is less effective. The effectiveness is greatly limited because it is depending on correct and consistent use. Condoms represent the point of the Hierarchy of Controls. Preventing the rising incidence rates of syphilis infections require administrative and engineering policies to identify and eradicate infections in the population. This is challenging because many cases are asymptomatic. Unlike other infections, syphilis can be transmitted at any point within the disease process, even by asymptomatic individuals. This aspect highlights the need for increased education about the risks of syphilis and how to minimize those risks. Increased education about this infection would be an Administrative Control. This education could be conducted in many ways including pamphlets/posters in clinic waiting rooms, education in middle/high school health class, college education, and directly from their physician. Although this education would be beneficial, it would be costly to implement. The effectiveness of this control is also highly dependent on how receptive the audience is, which is a limitation. To reduce incidence of congenital syphilis the CDC, the U.S. Preventive Services Task Force (USPSTF) and the American College of Obstetrics and Gynecology (ACOG) all agree screening of asymptomatic persons is recommended at the initial prenatal visits and during the third trimester for those at higher risk. Testing should be performed in anyone experiencing symptoms or any mother who is exposed. Syphilis can be treated if infections are discovered, which reduce the risks of congenital syphilis. Treatment can become challenging during pregnancy if the mother is allergic to penicillin because there are no proven alternative treatments to penicillin during pregnancy.6,7,8 Treating someone who has a severe allergy to penicillin would require a hospital supervised desensitization protocol which is costly to the healthcare system. There are no formal recommendations for screening females who desire to become pregnant. An administrative change would be to expand screening tests to any female who is trying to conceive. This would reduce the number of prenatal cases of syphilis. This policy change would increase the number of tests performed, but this increase would not carry a significant financial burden when compared to the increased costs of prenatal treatment or treatment of congenital syphilis cases. The effectiveness of this change in screening hinges on preconception planning, which according to the CDC, in 2011 approximately 45% of pregnancies were unplanned. 10 A similar administrative control would be to increase asymptomatic screening. Currently the CDC recommends only screening individuals at higher risk, which include persons with HIV, incarcerated persons, persons engaging in sex acts for money, transgender persons, and persons engage in same sex practices. The screening frequency is broad, ranging between yearly to every 3 months. Comparatively, the CDC and USPSTF recommend screening all sexually active females under age 25 on a yearly basis.7 It is my recommendation that screening should be expanded to include sexually active females and males, regardless of the type of sexual acts they engage in. This change would significantly increase the number of tests performed. In high incidence areas such as San Bernardino, this would also increase the number of cases identified. If cases are identified and eradicated, reducing spread of disease, and reducing complications from infection. Expanding the number of screening tests performed requires the infrastructure to handle that volume of tests which is a barrier to this policy benefiting the public health system. Currently syphilis and other STD tests can be performed for free or at low cost from a variety of organizations that include Planned Parenthood, SBC Public Health, and at any primary care clinic. Some labs such as Labcorp or Quest can perform these tests without a physician order. Cost of testing is varied, however both Planned Parenthood and the SBC PH clinics will offer free or discounted tests. According to San Bernardino County Public Health, it is mandatory for a healthcare provider to report a syphilis infection within 1 working day of identification. Instructions of how to report are available online. There are many reasons why this reporting system is beneficial. The Communicable Disease Section (CDS) works to minimize the spread of the disease by contacting the infected persons. The CDS can provide information and support to that person so they can receive timely treatment.11 An engineering control would be to have an automated reporting system. If reportable conditions are identified the health record could automatically contact the CDS. This would reduce the number of cases left unreported. This engineering change would be costly and would be technically challenging because of the various electronic health record systems. Elimination of syphilis within a population is possible because it is only transmitted between humans through intimate contact, vertically to fetus, and through infected blood. Vectors such as mosquitoes cannot spread human-based STDs. Elimination of the syphilis pathogen would require identification and treatment of all infected persons within a population. The smaller and more isolated the population the easier it would be to eliminate syphilis. This becomes progressively more challenging with increasing population size, increasing contacts between members of that population, and travel between discrete populations. Eradication is challenging because the infection can be asymptomatic for years and in some cases infected persons are unaware of the infection their entire life. The infection also causes such a wide range of symptoms that these symptoms may be mistaken for another illness. Syphilis can be difficult to diagnose and adequately treat because of limitations with certain testing methods. Because of these reasons, eliminating syphilis in a large population such as San Bernardino County is not a feasible goal. However, elimination of syphilis in persons who are identified to reduce incidence of new infections is possible and is a worthwhile goal. Elimination through adequate treatment requires identification and correct categorization of cases. Treatment methods differ depending on the category of the syphilis infection. Intramuscular or intravenous penicillin is the preferred treatment of adult cases at any stage of infection. Patients experiencing classical symptoms of primary or secondary syphilis, or those with a known exposure of less than 12 months can be treated with 1 dose of 2.4 million units of penicillin. Persons without obvious symptoms of primary/secondary syphilis and who have an unclear exposure history should be managed as late-latent syphilis (>12 months) requiring a 3-dose series of 2.4 million units each. Treatment of neuro, ocular, or otosyphilis requires 10-14 days of IV penicillin.12 Identification and classification can be challenging, latent syphilis can be present for years without any obvious symptoms and therefore late latent syphilis cases can mistakenly be treated as early latent. Inadequate treatment of false early latent syphilis can result in a failure to clear the infection. If this treatment failure is not identified, this person can continue to spread the infection. One change to the elimination procedure would be to treat early latent cases the same as late latent cases, with 3 doses of penicillin spaced 7 days apart. This change would reduce incidence of misclassification and suboptimal treatment. This would be an effective strategy for clearing a patient’s infection, however this increases burden on the patient and clinic because they would need to have 3 visits instead of 1. Increasing the number of visits would increase treatment nonadherence and would increase a clinic’s cost to treat a case of syphilis. The cost of penicillin is low compared to the cost of 2 extra clinic visits. The costs can be reduced by having nurse only visits for the 2nd and 3rd doses. Misinterpretation of lab tests is also a source of false negatives. The classical testing algorithm involves a non-treponemal test such as the RPR, if the RPR is negative then no further testing is typically performed, and the patient is deemed “negative.” The RPR screening method is flawed because the RPR levels will fall over time during a late latent infection and can be falsely “normal.” One strategy that is being implemented in high incidence areas such as San Bernardino is a reverse algorithm which uses a treponemal antibody test as the initial screening test. The treponemal antibodies will be positive for life and if positive they indicate an active infection or a previously treated infection. Another change to the current elimination strategy would be to expand the use of the reverse screening algorithm. This change would result in more false positives, but would reduce the number of false negatives. Increasing the number of false positives would possibly result in overtreatment of some patients. The risk of overtreatment is low compared to the individual and public health risks of missed cases. The final most effective elimination control is abstinence, however this strategy has it’s obvious limitations on a population scale. Another similar strategy is monogamous relationships where both partners have tested negative and/or have been fully treated. The success of this strategy is dependent on fidelity, which highlights the main obstacle for success. For the best success in prevention of syphilis each partner should be tested prior to engaging in intimate activities with a new partner or if an additional partner enters the relationship. Elimination controls are often the most effect, but also the most expensive. Abstinence and relational fidelity are, interestingly, very cost effective. These two controls are inexpensive monetarily, but some may consider them costly because of the behavioral changes necessary. There are no viable options for a substitution control, this would not be beneficial to the public. Substitution involves replacing the hazard with a safer alternative. There is no safer alternative to a syphilis infection. Many of these strategies would be perceived well by the stakeholders identified, however the challenges in implementation and the costs are barriers. Increased and improved education on the risks of syphilis and how to reduce infections would be well received by our educational systems. Similarly improved physician education on how to correctly identify and treat the different stages of syphilis would also be well received because of the complexity of this topic. Expanding the screening for syphilis would also be well received, but likely slow to implement to evaluate if this expanded screening will have unseen harms prior to widespread policy change. Encouraging abstinence, which if performed, is the most effective control, however it is also the least practical of the controls. The rising incidence rates of syphilis infections including congenital syphilis in San Bernardino County is a critical health topic. Public health policy changes will need to be implemented if there is going to be any change to the rapidly increasing incidence rates. The complexity of the infection is the primary driver to these incidence rates, which will require improved education. Infected persons can be asymptomatic for decades while they spread the pathogen, or they can present with disease mimics that are misclassified which necessitates expanded screening. Syphilis is also challenging to correctly stage and treat, which are necessary for elimination from the host. References AMA 11th Edition: 1. Sexually transmitted diseases. San Bernardino County Community Indicators. Accessed October 6, 2022. https://indicators.sbcounty.gov/wellness/sexually-transmitted-desease/ 2. Low N, Stroud K, Lewis DA, Cassell JA. Mind your binomials: a guide to microbial nomenclature and spelling in Sexually Transmitted Infections. Sex Transm Infect. 2015;91(3):154-155. doi:10.1136/sextrans-2014-051937 3. Syphilis - sti treatment guidelines. Published July 21, 2022. Accessed October 6, 2022. https://www.cdc.gov/std/treatment-guidelines/syphilis.htm 4. Detailed std facts - syphilis. Published October 6, 2022. Accessed October 12, 2022. https://www.cdc.gov/std/syphilis/stdfact-syphilis-detailed.htm 6. Condom fact sheet in brief | cdc. Published September 14, 2021. Accessed October 12, 2022. https://www.cdc.gov/condomeffectiveness/brief.html 7. US Preventive Services Task Force, Mangione CM, Barry MJ, et al. Screening for syphilis infection in nonpregnant adolescents and adults: us preventive services task force reaffirmation recommendation statement. JAMA. 2022;328(12):1243. doi:10.1001/jama.2022.15322 8. Sti screening recommendations. Published June 6, 2022. Accessed October 19, 2022. https://www.cdc.gov/std/treatment-guidelines/screening-recommendations.htm 9. Chlamydia, gonorrhea, and syphilis. Accessed October 19, 2022. https://www.acog.org/en/womenshealth/faqs/chlamydia-gonorrhea-and-syphilis 10. Unintended pregnancy | unintended pregnancy | reproductive health | cdc. Published July 20, 2021. Accessed October 19, 2022. https://www.cdc.gov/reproductivehealth/contraception/unintendedpregnancy/index.htm 11. About cds | department of public health. Accessed October 19, 2022. https://wp.sbcounty.gov/dph/programs/cds/about-cds/ 12. P&s syphilis - sti treatment guidelines. Published July 21, 2022. Accessed October 25, 2022. https://www.cdc.gov/std/treatment-guidelines/p-and-s-syphilis.htm