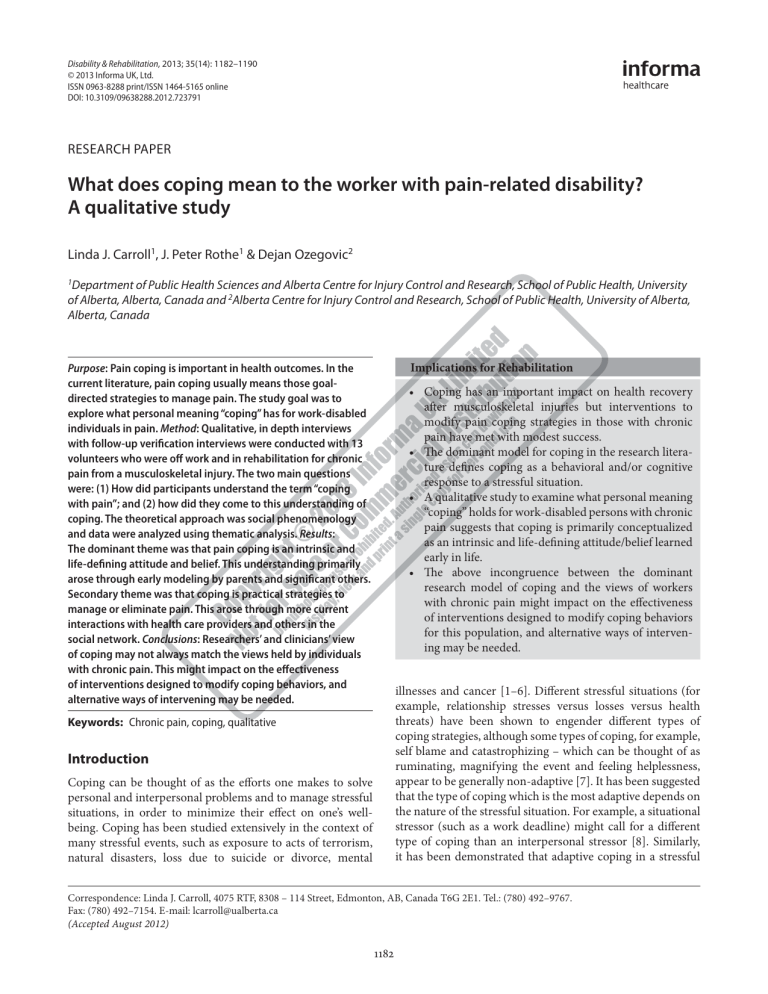
Disability & Rehabilitation, 2013; 35(14): 1182–1190 © 2013 Informa UK, Ltd. ISSN 0963-8288 print/ISSN 1464-5165 online DOI: 10.3109/09638288.2012.723791 RESEARCH PAPER What does coping mean to the worker with pain-related disability? A qualitative study Linda J. Carroll1, J. Peter Rothe1 & Dejan Ozegovic2 1 Department of Public Health Sciences and Alberta Centre for Injury Control and Research, School of Public Health, University of Alberta, Alberta, Canada and 2Alberta Centre for Injury Control and Research, School of Public Health, University of Alberta, Alberta, Canada Implications for Rehabilitation Purpose: Pain coping is important in health outcomes. In the current literature, pain coping usually means those goaldirected strategies to manage pain. The study goal was to explore what personal meaning “coping” has for work-disabled individuals in pain. Method: Qualitative, in depth interviews with follow-up verification interviews were conducted with 13 volunteers who were off work and in rehabilitation for chronic pain from a musculoskeletal injury. The two main questions were: (1) How did participants understand the term “coping with pain”; and (2) how did they come to this understanding of coping. The theoretical approach was social phenomenology and data were analyzed using thematic analysis. Results: The dominant theme was that pain coping is an intrinsic and life-defining attitude and belief. This understanding primarily arose through early modeling by parents and significant others. Secondary theme was that coping is practical strategies to manage or eliminate pain. This arose through more current interactions with health care providers and others in the social network. Conclusions: Researchers’ and clinicians’ view of coping may not always match the views held by individuals with chronic pain. This might impact on the effectiveness of interventions designed to modify coping behaviors, and alternative ways of intervening may be needed. t Coping has an important impact on health recovery after musculoskeletal injuries but interventions to modify pain coping strategies in those with chronic pain have met with modest success. t The dominant model for coping in the research literature defines coping as a behavioral and/or cognitive response to a stressful situation. t A qualitative study to examine what personal meaning “coping” holds for work-disabled persons with chronic pain suggests that coping is primarily conceptualized as an intrinsic and life-defining attitude/belief learned early in life. t The above incongruence between the dominant research model of coping and the views of workers with chronic pain might impact on the effectiveness of interventions designed to modify coping behaviors for this population, and alternative ways of intervening may be needed. illnesses and cancer [1–6]. Different stressful situations (for example, relationship stresses versus losses versus health threats) have been shown to engender different types of coping strategies, although some types of coping, for example, self blame and catastrophizing – which can be thought of as ruminating, magnifying the event and feeling helplessness, appear to be generally non-adaptive [7]. It has been suggested that the type of coping which is the most adaptive depends on the nature of the stressful situation. For example, a situational stressor (such as a work deadline) might call for a different type of coping than an interpersonal stressor [8]. Similarly, it has been demonstrated that adaptive coping in a stressful Keywords: Chronic pain, coping, qualitative Introduction Coping can be thought of as the efforts one makes to solve personal and interpersonal problems and to manage stressful situations, in order to minimize their effect on one’s wellbeing. Coping has been studied extensively in the context of many stressful events, such as exposure to acts of terrorism, natural disasters, loss due to suicide or divorce, mental Correspondence: Linda J. Carroll, 4075 RTF, 8308 – 114 Street, Edmonton, AB, Canada T6G 2E1. Tel.: (780) 492–9767. Fax: (780) 492–7154. E-mail: lcarroll@ualberta.ca (Accepted August 2012) 1182 Meaning of coping situation that is clearly within the individual’s control (for example, preparing for an exam) differs from adaptive coping in a situation that is not (or no longer) within that person’s control (for example, awaiting a grade after an exam) [9]. de Ridder and Schreurs point to a number of conceptual issues to be considered when applying the concept of coping to health conditions in particular. These include the question of whether coping should be considered a trait or a state. In other words, is coping style a function of global and stable individual characteristics, or is coping a dynamic, process oriented construct? These authors point out that coping researchers frequently focus their attention on behavioral, cognitive or emotional coping strategies, neglecting other important aspects of coping, such as how potentially stressful events are judged and interpreted, or what personal and interpersonal resources (supportive social network, self-esteem, others) help in forming the foundation for effective coping [7,10]. Pain is one type of stressor, and is an especially common one. The prevalence rate of chronic pain is similar across the western world—20–30% of the adult population suffers from chronic pain problems [11–13]. Chronic pain is an especially important problem in the working population because it is one of the most common causes of work disability in developed countries [14]. During any 2-year period, almost 10% of workers develop chronic back pain [15]; workers with back pain lose an average of 5.3 h of productive work each week because of pain [16]. Over the past two decades, pain-related coping has become a frequent topic of research investigation and theoretical discourse. For those with chronic pain problems, coping style has been shown to be associated with concurrent and subsequent pain severity, health status, outcomes (including return to work), psychological status, response to treatment and maintenance of treatment gains [17–22]. In this literature, coping has also been linked to a particular belief—expectations. It has been shown that those who expect severe symptoms after a musculoskeletal injury also use less adaptive coping strategies [23]. Given this finding, it may be that coping serves a key role in mediating the observed association between expectations for recovery (and possibly other pain-related beliefs) and actual recovery after a musculoskeletal injury [23–27]. Such findings have lead to an interest in developing interventions to modify coping, in an effort to improve outcomes in those with chronic pain. Yet studies in this area suggest that coping behavior is resistant to change, requiring intensive interventions and, while such interventions have met with some success [28,29], they appear to result in less improvement than might be hoped [30–32]. This suggests that coping is resistant to change in some manner we do not yet understand, and there may be a partial answer in developing a better understanding of how individuals in pain understand the construct of coping. In the pain literature, the most commonly used conceptualization of coping has arisen from the transactional model of stress [33]. This model defines coping as a process of purposeful efforts to manage stressors, which are those “external and/ or internal demands that are appraised as taxing or exceeding the resources of the person” [34]. Thus, by this definition, © Informa UK, Ltd. 1183 pain coping is dynamic and process-oriented (as opposed to a stable individual characteristic) and involves specific, intentional, goal-directed psychological and/or behavioral efforts to minimize the physical, psychological or social harm of pain. This model places an emphasis on the actual behavioral and/or cognitive coping strategies used, along with the individual’s cognitive appraisal of the situation. Most studies of chronic pain-related coping (including coping intervention studies) have adopted this model of coping, and the majority of pain-coping studies have used a quantitative paradigm. This has generally included administration of one of a variety of coping questionnaires, which ask individuals with chronic pain whether (and/or how often) they engage in particular cognitive or behavioral activities (pain coping strategies) to cope with their pain. (for examples of coping questionnaires, see [35–39]) There have been far fewer studies using qualitative research paradigms to examine coping in those with musculoskeletal pain, but these have also been useful in identifying types of coping strategies used by individuals with pain problems [26,40–43]. Examining the behavioral and cognitive strategies used by people to cope with their pain has a substantial impact on their health and other outcomes. However, it is also important to step back and study how individuals with pain problems understand and conceptualize coping. Such an investigation may help clinicians and researchers to develop more effective ways of intervening with those who engage in ineffective ways of coping with pain. Gaining a better understanding of how individuals with pain understand coping will help to both inform pain coping theory and aid in developing ways of assisting those in pain to enhance the effectiveness of their ways of coping. Thus, understanding the lived experiences of those with pain problems is important in both theory development and clinical management [44]. The current study was designed to address two questions about pain coping that to date have not been fully explored: (a) what does “coping” mean to the individual with chronic pain (how do individuals with pain assign common sense meaning to coping); and (b) how have individuals come to develop that meaning of coping? To address these questions, we used qualitative methods, since that methodology can help define what relevance pain coping has to individuals and how it relates to their expectations and self-identity, social relationships and social contacts. Our population of interest in this study was persons who were work-disabled because of chronic (duration of 3 months or more) musculoskeletal pain. Musculoskeletal injuries and conditions, such as neck, shoulder and low back pain, are the leading cause of workplace disability, and these conditions have been widely documented as being responsible for a high level of personal, financial and societal burden [45,46]. Methods Study design We used a qualitative study design, involving in depth individual interviews, with the overall goal of assessing how injured individuals understand and perceive “coping”. Our theoretical approach to this study was social phenomenology, 1184 L. J. Carroll et al. which is grounded in the earlier theoretical work done by social science philosophers Schutz, and Berger & Luckmann [47,48]. This approach places emphasis on the intent or motives underlying peoples’ actions (in this case, coping), and the taken-for-granted common sense principles that people use in coping. Phenomenology emphasizes the shared meaning of experiences through the principle of intersubjectivity. Because the world is social and not private, the researcher and those being researched share its meaning. There are common ground and common assumptions in how people establish that meaning and what meaning it establishes [49,50]. Thus, our study objective was to engage in in-depth interviews so that we could extract generalized observations from the convergence of injured workers’ shared relevancies, experiences, attitudes and assumptions. Table I. Characteristics of participants. Participants and setting The study took place in Edmonton, Alberta, Canada, one of two major cities in a province which has universal health care coverage. We recruited participants for this study from two rehabilitation facilities. One was a large, province-wide, multidisciplinary rehabilitation facility operated by the Workers Compensation Board in Alberta, Canada. It is the largest provider of occupational rehabilitation and disability management services in the province. In addition, to allow for the possibility that individuals being treated at that facility might have different views than those being treated at a private rehabilitation clinic, we also recruited patients from a private rehabilitation clinic which also has a large occupational-injury patient complement. The recruitment strategy was purposive sampling, in order to reflect the typical characteristics of those with a prolonged course of work-related disability. The study sample consisted of 13 volunteers (10 males and three females) with musculoskeletal pain, all of whom were being treated for work-related musculoskeletal injuries, which had occurred at least 3 months prior to the study. Approximately half the participants lived locally and half were from outside the city. Participants’ age group, sex, type of occupation at the time of injury, part of body injured (location of chronic pain) participants and time since injury are listed in Table I. At the time of the interview, all were collecting workers’ compensation or disability benefits for chronic pain arising from these injuries. Characteristics of the study sample were similar to those of the larger population of WCB benefit recipients who have prolonged pain problems from musculoskeletal injuries, that is, the majority were male, over the age of 40, with high school or less education, and suffering from back or neck/ shoulder injuries [51]. Contact was made with participants through informational posters which invited participation and provided general information about the study. These were posted in a conspicuous spot in the two rehabilitation centres which comprised our sampling frame. Interested individuals were asked to phone the study coordinator, at which time they were screened for inclusion criteria, provided with more information about the study, and arrangements were made for a data collection interview. Participants were provided with a small monetary reimbursement for their time, effort and expenditures. Code # 1 Age range 40’s Gender M Type of job when injured Construction 2 50’s M Manual labour 3 40’s M Transport 4 50’s M Industry 5 50’s M Construction 6 40’s M Construction 7 60s F Service Sector 8 60s M Skilled labour 9 30’s F Service sector 10 40s M Heavy labour 11 50s F Service sector 12 40s M Construction 13 30s M Transport Part of body injured, time since injury Back, 4 years ago Back, 4 years ago Neck/ shoulder, 7 months ago Neck/ shoulder 18 months ago Neck/ shoulder, 2 years ago Neck/ shoulder 1 year ago Neck/ shoulder 14 months ago, had surgery Neck/shoulder 4 months ago. Prior injuries Lower extremity 7 months ago. Prior back injury Back, lower extremity, 2 years ago Back, lower extremity, 3 months ago Back, lower extremity; 2 years ago. Back, neck 2 years ago Data collection Semi-structured interviews were conducted in a private office within the rehabilitation clinics. The interview format consisted of two interviewers in tandem with a respondent in a closed room around a table. The interview design maintained conversational levels in which free flow of information could be assured [52]. The principles of social phenomenology guided the interviews. An interview guide was developed in advance, informed by the literature, informal discussions with people in pain and health care professional and researchers’ experience with patients with chronic pain. However, interviews were designed to be iterative so that additional themes could be formulated within and between interviews, as interviews progressed. This process is consistent with social-phenomenology theory, that is, we seek to discover the world as it is experienced by those involved in it, in order to explore the nature of human experience and the meaning that Disability & Rehabilitation Meaning of coping people attach to their experiences [53]. An iterative approach permitted us to deal with unanticipated issues, classifications, illustrations and additional relevant information. It offered respondents opportunities to articulate their feelings, experiences and perceptions as fully as possible. Questions were conversational and, although pre-defined, they did not follow a particular sequence. The emphasis was on the logic-in-use or pattern of discourse, the way in which they reasoned their responses, and made connections across phenomena. To help arrive at embedded meanings, we sought maximal use of probes and tags to gain the most descriptive account possible, from the general to the specific, from the public to the private and personal, and from the least defensive to the most [52]. The main topic areas addressed by the interview were as follows: (1) How do you understand the term “coping with pain”; and (2) how did you come to know about this understanding of coping? Interviews lasted between 1.5 and 2 h, and were audio recorded and transcribed verbatim. A three-step data verification process was used. The first was the use of inter-respondent verification procedures during interviews whereby respondents were asked about critical issues or anomalies that were raised by earlier participants. The second was another on-site verification process, which consisted of tagged responses and probes, whereby the interviewer introduced such phrases as, “Do you mean that . . . ,” “Are you saying that . . .” and “Give me an example of . . .” to attain a more embedded sense of meaning and to ensure clarification, illustration and expansion of ideas [49]. The third step re-engaged participants after the first round of data analysis, and involved a follow-up interview (also recorded and transcribed) in which participants were invited to comment on the initial interpretations to ensure accuracy and relevance, and to provide participants with the opportunity to clarify, correct, add comments and further information. Ethics approval for this study was granted by the University of Alberta’s Health Research Ethics Board. Prior to the start of the interview, all participants provided written informed consent to participate in the study and to permit audio recording of the interviews. They were assured that participation would have no bearing on their health care or on their benefits and that information they provided would not be reported to their insurer or their health care providers. Once the interview process was completed, names and personally identifying information were deleted and numerical codes were assigned to ensure confidentiality. Data analysis Our goal for data analysis was to identify, through thematic analysis, dominant patterns or themes embedded in the data [54]. We used an induction strategy, which is a process of elaboration in which descriptions are achieved through an iterative approach from the analysis of one interviewee to the next [55]. First, the verbatim transcriptions were read several times as a group. The information was then classified and coded into tentative emerging themes. This first round of analysis became the foundation for engaging interviewees with verification interviews, which also became part of the data pool for analysis. The identification of emerging themes © Informa UK, Ltd. 1185 was followed by extraction of sub-themes and social contexts within which the sub themes were embedded. In a recursive process, as interviews were coded and thematized, each successive interview (including the verification interviews) became a source for additional generalizations, and the originally coded interviews were reassessed for themes or codes that arose from later reviews. Eventually a body of interrelated generalizations was elaborated, through thematic indexing, to elaborate how participants constructed their ways of coping with pain [56]. Through a process of constant comparison across all interviews and between interviews and analysis, similarities and differences across interview material were identified. The initial analysis was conducted by the second author, and then reviewed by the first author. Any areas of discrepancy between these two authors was discussed and consensus reached. Finally, agreement on the final themes was obtained from all authors. Results Saturation was reached with 13 participants. The findings from the interviews support the idea that there are overarching meanings that typify how injured workers understand and experience the concept of coping with pain. Quotations from the interviews are followed by the number of the informant in round brackets. These insider thoughts and experiences provide rich perspectives on the meaning of coping, and the context in which coping occurs. Meaning of coping There were two main conceptualizations of what “coping” means: an intrinsic and life-defining (or sometimes lifechanging) attitude; and behavioral/cognitive strategies for managing their pain. However coping was defined, however, a common thread for the persons in this study was that living with chronic pain means struggling to cope, and struggling to understand what it means to cope. How these respondents defined and understood coping served as the foundation for how they cope. Coping as an intrinsic and life-defining attitude A typical view expressed was that the concept of coping did not primarily mean a series of strategies used to manage pain; rather coping had become an intrinsic part of their overall world view, self-view and belief system. The meaning of coping transcended the day-to-day management of pain. Coping was more than technique or strategy; it was a life-altering experience; a definition or re-definition of life. For example, an injured worker, whose injury had occurred 20 months previously, told us that coping was intrinsic change in himself; the need to alter his perspectives, attitudes, life style and his expectations. He described himself as being “forced” to live with pain—something he had never before experienced. Coping, to him, meant: “[looking at] things in a different perspective. [Coping is a] rationalization in the brain [that] things will get better . . . I know I’m going to be in pain and I know it’s going to be hurting but I know I’m slowly getting better . . . I’m trying to make the best of everything I can.” (participant 4) 1186 L. J. Carroll et al. For the above individual, coping was less about “managing” the pain, and more about understanding and coming to terms with the realization that he would never be the same, but that his condition was slowly getting better. He talked about having to accept that his injury and pain had taken away his freedom of movement. Similarly, another participant equated coping with understanding and accepting the pain; using the “power of the mind” to do so. He believed that pain is a mental state, and that the mind is: “. . . more powerful than any drug in the world. The mind. Understanding your pain and working through it.” Furthermore, he went on to say “. . . a human should be able to survive anything. Basically. Pain or mental anguish, or whatever, you should be able to work your way through it. Knowledge and understanding will make you work through it . . . You’ve got to be able to take pain. You’ve got to be able to figure out a way to ‘yeah, okay, that pain is there.’ You’ve got to accept it!” (participant 2) For participant 6, coping reflects: “. . . mind over matter . . . I think one of the keys [to coping] might be – so much of a person’s personality plays a part”. Another emphasized the importance of “perseverance” and belief in coping: “It’s faith . . . you know what – it’s what you believe. What’s the belief? If you don’t believe that your body is not going to heal, then it isn’t” (Participant 7). Another spoke about having to have the right attitude: “it’s all about the right attitude. If you’re grumpy and angry and bitchy, it’s ain’t going to help. Nothing’s going to help. Not even the right physio people, nothing”. He went on to reflect his belief that “attitude” is the essential component in coping with all life’s problems, and that: “If you’ve got a bad attitude no, you can’t [cope], it’s an impossibility” (Participant 8). Participant 11 was more specific in her assertion that the essence of coping is having a positive attitude, and seeing the positive in every situation, no matter how difficult: “. . . you still have to bring that around – to come out with a positive. I’m a very positive person. Sometimes it just takes me a little while to get back to, ‘well, OK there was a good part to this and I have to find it’. As hard as it’s going to be, you need to find it [the positive]. You have to come up with at least a thread of positive in this ordeal. And come around. And, you can do it. So you get up, up and you can carry on. You can do it. So stop crying, and get up, and go out there, and do what you have to do.” Likewise, participant 10 said about coping: “a lot of it has to do with the fact that it’s your personal makeup, the type of person you are. Right? . . . But you know, I come from pretty sturdy stock”. Coping as cognitive or behavioral strategy As a secondary theme, coping was conceptualized as strategy-oriented; a practical action to manage or (less often) to eliminate the pain. This included such things as using ice or heat, medications, engaging in activities (as distraction) or, alternatively avoiding activities (because they make the pain worse), doing their physiotherapy exercises or (alternatively) avoiding doing their physiotherapy exercises, among other strategies. To illustrate, one participant with shoulder pain defined personal coping as: “. . . dealing with it [pain]. Dealing with it within your abilities and limitations” (Participant 3). He further described coping as practical actions, such as “exercising – just loosening it up” to manage the pain, and went on to say: “I’d like to be 100% again. I would like that. I’m thinking [I will get to] 90, 95% . . . It won’t be the [range of] motion, it would be more the strength I think . . . that’s for my job—what I need is my strength. The [range of] motion you can get around, but the strength is the thing you really need.” (participant 3) For this individual, successful management of pain was idealized as the way to attain the future goal of gaining his strength back, and “coping” meant an active process of improving shoulder strength through exercise. For participant 4, coping was described as involving an intrinsic change in himself; however, he also went on to describe some of the coping strategies he had learned: “. . . ice certainly makes a difference and then in the mornings it is somewhat stiff and then I find a hot shower and . . . a little stretching helps it out”. He also talked about effective coping as involving “. . .reading your body and just knowing what you are, or what your limitations are, but at the same time . . . also pushing those boundaries” (participant 4). In contrast, another participant with shoulder pain also saw coping as a way of managing the pain, but rather than using exercise to improve strength and movement, his way of coping focused on using his other arm more and avoiding those activities that made his pain worse. He said that to him, coping means: “trying to live with it in a way, [that] to me is coping . . . trying to find a way to deal with it. I used to take a lot of pain killers . . . and I decided to stop because I didn’t want to get used to it, get a pill to control my pain so I kind of wanted to myself control the pain in a way. Trying like say to live with it and trying to avoid those things that will alleviate pain. Go easy on the exercise . . . I go easy, I use ice at home . . . just to alleviate some of the pain.” (participant 5) Similarly, another interviewee described his meaning of coping as strategy oriented: “. . . trying to find strategies and ways to deal with pain and managing it one way or another” (participant 13). Although some participants conceptualized coping as a way of managing the pain, for others, coping meant pain cessation—one copes in order to put an end to the experience of pain (typically through use of medication). For example, participant 13 went on to say: “[Coping] means a lot to me, actually. When you’re in pain constantly every day—you’ll pretty much to do anything not to be”. He talked about relying on medication to cope with his back injury because “nothing else seems to take the pain away”. Coping with pain is related to other life aspects A complementary theme emerging from the data is that pain coping is complex—pain coping cannot occur in isolation of coping with other aspects of life. For example, one young injured worker emphasized the importance of “stress” when talking about the personal meaning that coping has for him. He described this as a key factor in his life. “. . . being able to deal with stress . . . Yeah, coping with life—yeah —coping with pain . . . If you’re stressed out, you feel that stress everywhere—you’re in pain . . . stress . . . it doesn’t help. [Stress] makes the Disability & Rehabilitation Meaning of coping pain go from a 10 up to a 70 [on a 100 point scale of pain intensity]. I think that one of the things that makes it hurt the most is stress. Coping with stress with pain . . . If somebody’s acting or doing something to make me feel stressed, I just leave. That’s all there is to it. I give them the ‘toodles’” (participant 13). Another participant (1) also highlighted the negative impact stress has on his ability to cope: “Stress is a hard one. It takes a lot of physical and mental out of me . . . you’re stressed your body’s not working right . . . nothing is going good. Stress is not a good, a good feeling to have. It’s something everybody goes through, obviously, you know, from time to time. But to have it as top dog, always weighing on you. It’s difficult for you to cope . . . it’s harder to cope when you’re stressed, isn’t it? . . . The more stress I’m in, the more pain I have.” In summary, the meaning of coping appeared to be understood by study participants in two ways, although these themes sometimes overlapped. The dominant theme was to see coping as an intrinsic and life-defining attitude and belief system; and, related to this, to see coping with pain as a complex phenomenon that encompasses coping with other areas of one’s life. In this way, “coping” was an expression of “the way I am”. The secondary conceptualization of coping was as a way of managing or eliminating pain through practical strategies. In that respect, coping was conceptualized as “what I do”. Where did they learn this meaning of coping? Personal meanings of coping are not haphazard views about life. They represent a fundamental reference point for a person’s beliefs, attitudes and behaviors. The interview data showed three prominent ways of having come to a personal meaning of coping. These were: (1) through family role models, including modeling by parents and significant others during their childhood and early adulthood (by far, the predominant theme); (2) through their health care providers; and (c) through recent and current interactions with others who also have pain problems (e.g. in treatment programs and support groups). The most prominent theme to emerge was that the understanding of what coping means came early in life. This was especially true for those individuals who saw coping as an intrinsic part of their world and self view. These early lessons on the meaning of coping were learned primarily from parents but also through other early experiences. Sometimes “coping” was understood through the lifestyle experienced as a child. For example, living on the farm denoted toughness—no whining, and getting the job done, regardless of health. An injured worker said: “I did grow up on a farm . . . You just keep on going. That’s what we were told. Sure we had a little bit of sympathy . . . We could whine for a few days, but then it was get up and go. Get back at your chores and keep going.” (participant 7) Sometimes, learning about what it means to cope meant living in a family situation where a parent (often a father) was a role model for “toughing it out”. For example, one injured worker said: “My Dad . . . handles pain, like, he’s got a really © Informa UK, Ltd. 1187 high pain threshold. He just deals with pain like I’ve never seen anybody else” (participant 3). Another participant also learned about coping from his father: “. . . my father . . . He was a tough man . . . I learned [coping] from that” (participant 8). For many other participants, learning what it means to cope with pain also came from early life experiences in how pain was managed in the family. The message here was that a child may be injured, but should not be “coddled” by parents—that child must learn to go on with life. For example: “I also think that it [my understanding of coping] goes back to, you know, when you’re a kid and hurt yourself you cry. Well, you know, some parents will coddle and that might be important at an age, but sooner or later that has to stop. A skinned knee is a skinned knee. ‘Wake up kid . . . put a bandaid on it and stop crying.’ So as you get older, you have choices to make whether you are going to continue a sport or go to work the next day under some pain, right.” (participant 6) Early models for coping were not necessarily limited to coping with illness or injury, but were more general in nature: coping with life’s hardships of many kinds. One participant learned what it means to cope by understanding how his father coped with his wife’s death. “When my Mom died, he [my father] lost ‘till death do them part.’ He went out and he drank for a week. He didn’t want to stop drinking he says, and then he just woke up on Monday and went to work. And ever since that I think that if he’s strong enough to deal with losing his love, I should be able to deal with life right. I just get up and go.” (participant 13) Sometimes the role model for toughness was another family member. One participant told us about learning about coping from his brother, a millwright by trade who became debilitated because of knee problems, and had to walk with a leg brace and cane. According to the interviewee: “He [my brother] brought himself around. He went back to work . . . well, hell, if he can do it, why can’t I? He is older than me. And now I’ve come to the realization, well he’s been a physical labourer all his life too; he’s never had an office job, an easy job. So why am I such a wimp?” (participant 2) This interviewee came to believe that he should cope with adversity like his brother did: “Understand it. Get over it. Life goes on . . . And I’ll tell you, nine people out of ten don’t really give a shit if you got pain. You can tell them all you want . . . Don’t cry to yourself and to people around you. Because it gets the point that they don’t give you a rat’s tooth about it.” He has analyzed his brother’s experiences and has come to the conclusion that the final responsibility for coping lies with the person in pain. Coping means toughing it out, as exemplified by his brother’s actions. For others, early models of coping involved learning to be positive in the face of adversity, rather than being “tough”. For example, one woman talked about the importance of positive thinking and positive attitude, and she attributed having developed this attitude to her mother’s influence, saying: “. . . I’ve just always just been a really positive person . . . I don’t know, maybe it came from [how I was] raised. My mom’s a psych nurse so she has always been a great support.” (participant 11) 1188 L. J. Carroll et al. Although not the dominant theme, the influence of health care professionals and/or the respondent’s current social network (including fellow rehabilitation patients) was also apparent. This arose when participants were discussing coping as strategy oriented, rather than as intrinsic attitudes and beliefs. For example, “[The therapist] has taught me mental imagery . . . My pain was probably a nine when we started . . . to about a two when we finished . . .” (participant 2) This respondent talked about having been taught imagery techniques by his physical therapist, which helped, not only with decreasing the pain through use of narcotics, but also with smoking cessation. He described the imaging techniques that he has been taught as “retraining the brain”. Yet another respondent had learned about pain coping strategies from a psychologist he was seeing, and in pain management classes offered as part of his rehabilitation program: “. . . I find that . . . having Dr. (psychologist) to talk to and then just those classes I had while I was at the (name of treatment facility) certainly has helped in the coping and just putting things into perspective.” (participant 4) Yet for others, the perspective of coping advocated by their health care providers received mixed reviews; for example: “Stretching. They tried to tell me stretching helps. They’re full of it. Stretching does not help. Not me anyways. It makes me want to cry and it makes me feel like my back is going to jump out and run away . . .” (participant 13) For others who saw pain coping as strategy oriented, learning about coping came by word of mouth, talking about ideas with co-workers, gym mates or other people in pain. As one participant said: “I like to hear about how they are dealing with their pain because I know how I’m dealing with mine . . .” (participant 7). Another told us: “. . . . that’s how you learn, is from the other workers” (participant 8). One worker went a step further, starting her own coping group, telling us: “. . .we just went and had to learn how to cope with no money and our problems . . . So we started our own coping group” (participant 7). However, not everyone found sharing ideas on coping useful. Respondents 12 and 13 were both adamant that “it doesn’t help talking about it”. In summary, the personal meaning of coping backstops the approach taken to coping. The main way of understanding what coping means was through early role modeling by parents and significant others. This was especially true when defining coping as an intrinsic part of their overall world view, self view and belief system—an aspect of “who I am”. When coping was conceptualized as an intrinsic characteristic—toughness or positivity—involving resilience, it was generally learned at an early age. Understanding the concept of coping through interactions with health care providers and others with pain problems was a secondary theme which emerged, and was related to the idea of coping being a strategy, or “what I do”. Discussion We conducted a qualitative study of how individuals with chronic pain conceptualize “coping”. Those interviewed had pain problems of a severity to have lead to work disability, and all were in rehabilitation treatment. The dominant theme emerging from the interviews was that pain coping is an intrinsic and life-defining attitude and belief; an idea that arose primarily through early modeling by parents and significant others. The secondary conceptualization of coping was that of practical strategies to manage or eliminate pain; this generally arose through more current interactions with health care providers and others in the current social network. These ideas of coping can be compared and contrasted with how coping is commonly presented in much of the current pain coping literature. That is, in the published literature, coping (in general) is most commonly understood to mean deliberate, goal-directed strategies to manage an unpleasant situation or stressor. Pain is one such stressor. In the pain coping literature, “coping” with pain generally refers to the various cognitive and/or behavioral efforts used by persons in pain to manage that pain. In other words, coping is something people do (i.e. a behavior and/or cognitive act). Questionnaires designed to assess coping typically ask respondents what they do (and how often) in response to pain. Interventions addressing coping are typically educational and cognitivebehavioral in orientation, aimed at changing what people in pain do (cognitively or behavioraly) in response to pain. However, in our study, the idea that coping means engaging in strategies or activities to manage or eliminate pain was clearly a secondary theme, despite that idea’s prominence in the pain coping literature. Interestingly, to many in our sample of workers with long standing and disabling pain problems, the concept of “coping” with pain had a much more profound and personal meaning. The dominant and most salient theme elicited from interviews with these individuals was that pain coping is complex and represents a fundamental and intrinsic stance in attitudes and beliefs. Pain coping was described as a complex process that could not be isolated from other aspects of life. Consistent with the idea that coping is a construct of deep personal meaning, involving intrinsic and core beliefs and attitudes, participants in this study who held this view primarily attributed their understanding of how to cope (i.e. how they learned what it is “to cope”) as stemming primarily from the early influences of parents and significant others, who passed along their values. These values include, for example, the importance of being physically and mentally “tough” or of having a positive attitude. These lessons in coping transcended the type of adversity—coping with pain was to be approached in the same way as coping with other life events. This view conceptualized coping primarily as an intrinsic resilience, learned at an early age. The message from these participants was that coping had to do with “who I am”. In contrast, when coping was seen as something one does to manage or eliminate the pain (i.e. the view that “coping” is equated with engaging in “coping strategies”), the role of health care providers, colleagues, friends and fellow pain sufferers in helping (or not Disability & Rehabilitation Meaning of coping helping) became important in understanding how to cope with pain. This conceptualization of “coping” corresponds much more closely with the conceptualization of coping more commonly seen in the literature. One interesting conjecture that arises from these data is that the fundamental view that coping arises from early lessons in how to face adversity and reflects “the way I am” may be incompatible with an intervention philosophy that coping is a set of behaviors. This may be part of the explanation of why even the most intensive interventions to address coping have only modest success. That is, for at least some individuals with pain, the paradigm behind educational and cognitive-behavioral coping interventions does not match their personal paradigm of what coping means. It may be that for these individuals, a more effective intervention approach might begin by explicitly recognizing and attending to their personal meanings of coping and the fundamental life stances that comprise coping—that is, the coping intervention paradigm may need to match the patient’s coping paradigm. On the other hand, for those whose own coping paradigm is primarily strategy-oriented, the more usual educational and cognitive-behavioral approach may be a closer treatment match, and thus (potentially) more effective. This possibility could be tested through randomized controlled trials. However, before engaging in intervention studies, it is important to better understand the linkages among world/life views and attitudes learned in early life; beliefs and attitudes specific to pain; pain coping definitions, beliefs and activities; and pain outcomes. We have evidence that certain beliefs about pain (e.g. pessimism about recovery, the belief that work will make the pain problem worse) are associated with poorer recovery outcomes [57–59]. However, our understanding of these linkages is limited and questions remain. For example, if an individual grows up with models of needing to be “tough” (or alternatively “positive”) when facing adversity such as pain problems, what implications does that have for his or her attitudes toward pain, how he or she copes, and openness to modifying maladaptive beliefs, attitudes and ways of dealing with pain? Our study has strengths and weaknesses. The social phenomenological approach used to explore the personal meanings of coping is well-suited to this research aim, and those participating in this study were representative of the target population, which was individuals with pain problems of a severity as to lead to work disability. This is a socially and clinically relevant group, given both the personal and societal costs of work disability. However, these findings arise from a relatively small sample, and may not reflect the experience and ideas of persons with less severe or more acute pain problems, or those who have not sought rehabilitation. It may also be that volunteers to this type of study relate different experiences and conceptualizations than non-participants would have, and that the phenomenon of coping might be viewed very differently by these groups. However, the ways of coping mentioned by participants (e.g., exercise, medications, talking with others, mental imagery, avoidance of those activities that hurt) are typical of those strategies endorsed in larger, quantitative studies. © Informa UK, Ltd. 1189 Quantitative studies conducted to date have lead to significant advances in our understanding of coping and pain outcomes. However, the findings in this study suggest that the use of strategy-oriented coping questionnaires when conducting research on coping and its role in pain disability and recovery may not capture all the relevant information. The addition of qualitative methods to explore pain patients’ personal meanings of coping and the associated fundamental life stances that comprise coping can help us to better understand and contextualize the existing findings from quantitative studies and develop new ways of addressing the issues. Quantitative and qualitative studies arise from different research paradigms, and produce different levels of meaning [60]. Integrating these complementary approaches by respecting what knowledge each brings can aid in formulating a more complete, embodied picture of coping with chronic pain. Declaration of Interest: This study was made possible by a grant from WCB-Alberta Research Program. References 1. Danieli Y, Brom D, Sillsk J. The trauma of terrorism: Sharing knowledge and shared care; An international handbook. New York: Routledge, 2005. 2. Ehrenreich JH. Coping with disaster: A guidebook to psychosocial intervention (Revised Edition). New York: Mental Health Workers without Borders, 2001. 3. Kaslow NJ, Gilman Aronson S. Recommendations for family interventions following a suicide. Prof Psychol Res Practice 2004;35:240–247. 4. Manuel GM, Roth S, Keefe FJ, Brantley BA. Coping with cancer. J Human Stress 1987;13:149–158. 5. McKenry PC, Price SJ. Families and change: Coping with stressful events and transitions. Thousand Oaks, California: Sage Publications, 2005. 6. Roe D, Chopra M. Beyond coping with mental illness: toward personal growth. Am J Orthopsychiatry 2003;73:334–344. 7. Schroevers M, Kraaij V, Garnefski N. Goal disturbance, cognitive coping strategies, and psychological adjustment to different types of stressful life event. Personal Individual Differences 2007;43:413–423. 8. O’Brien TB, DeLongis A. The interactional context of problem-, emotion-, and relationship-focused coping: the role of the big five personality factors. J Pers 1996;64:775–813. 9. Folkman S, Lazarus RS. If it changes it must be a process: study of emotion and coping during three stages of a college examination. J Pers Soc Psychol 1985;48:150–170. 10. de Ridder D, Schreurs K. Developing interventions for chronically ill patients: is coping a helpful concept? Clin Psychol Rev 2001;21:205–240. 11. Blyth FM, March LM, Brnabic AJ, Jorm LR, Williamson M, Cousins MJ. Chronic pain in Australia: a prevalence study. Pain 2001;89:127–134. 12. Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006;10:287–333. 13. Moulin DE, Clark AJ, Speechley M, Morley-Forster PK. Chronic pain in Canada–prevalence, treatment, impact and the role of opioid analgesia. Pain Res Manag 2002;7:179–184. 14. Vas J, Perea-Milla E, Mendez C, Silva LC, Herrera GA, Aranda Regules JM, Martinez Barquin DM, Aguilar I, Faus V. Efficacy and safety of acupuncture for the treatment of non-specific acute low back pain: a randomised controlled multicentre trial protocol. BMC Comp Altern Med 2006;6. 15. Pérez CE. Chronic back problems among workers. Health Rep 2000;12:41–55 (Eng); 45. 16. Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the US workforce. JAMA 2003;290:2443–2454. 17. Brown GK, Nicassio PM, Wallston KA. Pain coping strategies and depression in rheumatoid arthritis. J Consult Clin Psychol 1989;57:652–657. 1190 L. J. Carroll et al. 18. Carroll L, Mercado AC, Cassidy JD, Cjté P. A population-based study of factors associated with combinations of active and passive coping with neck and low back pain. J Rehabil Med 2002;34:67–72. 19. Jensen IB, Nygren Å, Gamberale F, Goldie I, Westerholm P. Coping with long-term musculoskeletal pain and its consequences: Is gender a factor? Pain 1994;57:164–151. 20. Jensen MP, Turner JA, Romano JM. Changes after multidisciplinary pain treatment in patient pain beliefs and coping are associated with concurrent changes in patient functioning. Pain 2007;131:38–47. 21. Keefe FJ, Affleck G, Lefebvre JC, Starr K, Caldwell DS, Tennen H. Pain coping strategies and coping efficacy in rheumatoid arthritis: a daily process analysis. Pain 1997;69:35–42. 22. Mercado AC, Carroll LJ, Cassidy JD, Côté P. Passive coping is a risk factor for disabling neck or low back pain. Pain 2005;117:51–57. 23. Ferrari R, Russell AS. Correlations between coping styles and symptom expectation for whiplash injury. Clin Rheumatol 2010;29:1245–1249. 24. Cole DC, Mondloch MV, Hogg-Johnson S; Early Claimant Cohort Prognostic Modelling Group. Listening to injured workers: how recovery expectations predict outcomes–a prospective study. CMAJ 2002;166:749–754. 25. Fadyl J, McPherson K. Return to work after injury: a review of evidence regarding expectations and injury perceptions, and their influence on outcome. J Occup Rehabil 2008;18:362–374. 26. Krohne K, Ihlebaek C. Maintaining a balance: a focus group study on living and coping with chronic whiplash-associated disorder. BMC Musculoskelet Disord 2010;11:158. 27. Ozegovic D, Carroll LJ, David Cassidy J. Does expecting mean achieving? The association between expecting to return to work and recovery in whiplash associated disorders: a population-based prospective cohort study. Eur Spine J 2009;18:893–899. 28. Jensen IB, Bodin L. Multimodal cognitive-behavioural treatment for workers with chronic spinal pain: a matched cohort study with an 18-month follow-up. Pain 1998;76:35–44. 29. Jensen IB, Nygren A, Lundin A. Cognitive-behavioural treatment for workers with chronic spinal pain: a matched and controlled cohort study in Sweden. Occup Environ Med 1994;51:145–151. 30. Buhrman M, Nilsson-Ihrfeldt E, Jannert M, Ström L, Andersson G. Guided internet-based cognitive behavioural treatment for chronic back pain reduces pain catastrophizing: a randomized controlled trial. J Rehabil Med 2011;43:500–505. 31. Leyshon RT. Coping with chronic pain: current advances and practical information for clinicians. Work 2009;33:369–372. 32. Meng K, Seekatz B, Roband H, Worringen U, Vogel H, Faller H. Intermediate and long-term effects of a standardized back school for inpatient orthopedic rehabilitation on illness knowledge and selfmanagement behaviors: a randomized controlled trial. Clin J Pain 2011;27:248–257. 33. Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York: Springer Publishing Company, 1984. 34. Folkman S, Lazarus RS. The relationship between coping and emotion: implications for theory and research. Soc Sci Med 1988;26:309–317. 35. Brown GK, Nicassio PM. Development of a questionnaire for the assessment of active and passive coping strategies in chronic pain patients. Pain 1987;31:53–64. 36. Folkman S, Lazarus RS. An analysis of coping in a middle-aged community sample. J Health Soc Behav 1980;21:219–239. 37. Jensen MP, Turner JA, Romano JM, Strom SE. The Chronic Pain Coping Inventory: development and preliminary validation. Pain 1995;60:203–216. 38. Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain 1983;17:33–44. 39. Sullivan MJ, Bishop S, Pivik J. The Pain Catastrophizing Scale: Development and validation. Psychological Assessment 1995;7:524–532. 40. Crowe M, Whitehead L, Jo Gagan M, Baxter D, Panckhurst A. Selfmanagement and chronic low back pain: a qualitative study. J Adv Nurs 2010;66:1478–1486. 41. Kengen Traska T, Rutledge DN, Mouttapa M, Weiss J, Aquino J. Strategies used for managing symptoms by women with fibromyalgia. J Clin Nurs 2012;21:626–635. 42. Lillrank A. Back pain and the resolution of diagnostic uncertainty in illness narratives. Soc Sci Med 2003;57:1045–1054. 43. Tveito TH, Shaw WS, Huang YH, Nicholas M, Wagner G. Managing pain in the workplace: a focus group study of challenges, strategies and what matters most to workers with low back pain. Disabil Rehabil 2010;32:2035–2045. 44. Russell G, Nicol P. ‘I’ve broken my neck or something!’ The general practice experience of whiplash. Fam Pract 2009;26:115–120. 45. Baldwin ML, Butler RJ. Upper extremity disorders in the workplace: costs and outcomes beyond the first return to work. J Occup Rehabil 2006;16:303–323. 46. Waddell G, Burton AK. Is work good for your health and well-being? London, UK: The Stationary Office, 2006. 47. Berger PL, Luckmann T. The social construction of reality. New York, NY, USA: Anchor Books, 1966. 48. Schutz A. The phenomenology of the social world. Evanston, IL, USA: Northwestern University Press, 1967. 49. Rothe JP. Undertaking qualitative research. Concepts and cases in injury, health and social life. Edmonton, Canada: The University of Alberta Press, 2000. 50. Rothe JP. Driving lessons: systems thinking and consequences. Edmonton, AB: University of Alberta Press, 2002. 51. Phillips LA, Carroll LJ, Voaklander DC, Gross DP, Beach JR. Pain coping in injured workers with chronic pain: what’s unique about workers? Disabil Rehabil 2012;34:1774–1782. 52. Rosenberg B, Silverston H. The varieties of delinquent experience. New York: Schocken Books, 1983. 53. Schutz A. Collected papers Vol. I. The problem of social reality. The Hague: Martinus Nijhoff, 1962. 54. Braun V, Clark V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 55. Homans G. The human group. New York: Harcourt, Brace & World, Inc., 1950. 56. Becker H. Sociological work: method and substance. New Brunswick, NJ: Transaction Publishers, 1977. 57. Adams N, Field L. Pain management 1: psychological and social aspects of pain. Br J Nurs 2001;10:903–911. 58. Carroll LJ, Holm LW, Hogg-Johnson S, Côté P, Cassidy JD, Haldeman S, Nordin M, et al.; Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Course and prognostic factors for neck pain in whiplash-associated disorders (WAD): results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008;33:S83–S92. 59. Cole D, Mondloch MV, Hogg-Johnson S. Listening to injured workers: how recovery expectations predict outcomes — a prospective study. Can Med Assoc J 2002;166:749–754. 60. Carroll LJ, Rothe JP. Levels of reconstruction as complementarity in mixed methods research: a social theory-based conceptual framework for integrating qualitative and quantitative research. Int J Environ Res Public Health 2010;7:3478–3488. Disability & Rehabilitation