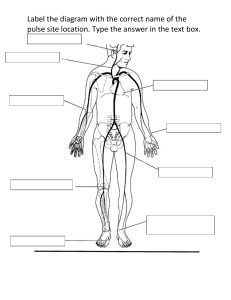
Mosby: Mosby's Nursing Video Skills Procedural Guideline for Assessing Apical Pulse Procedure Steps 1. Verify the health care provider’s orders. 2. Gather the necessary equipment and supplies. 3. Perform hand hygiene. 4. Provide for the patient’s privacy. 5. Introduce yourself to the patient and family if present. 6. Identify the patient using two identifiers. 7. Assess for factors that can affect the apical pulse rate and rhythm, such as medical history, disease processes, age, exercise, position changes, medications, temperature, or sympathetic stimulation. 8. Gloves are only worn if nurse will be in contact with bodily fluids or the patient is in protective precautions. 9. Help the patient into a supine or sitting position, and expose the sternum and the left side of the chest. 10. Locate the point of maximal impulse (PMI, or apical impulse). To do this, find the angle of Louis, which feels like a bony prominence just below the suprasternal notch. 11. Slide your fingers down each side of the angle to find the second intercostal space (ICS). Carefully move your fingers down the left side of the sternum to the fifth intercostal space and over to the left midclavicular line. 12. Feel the PMI as a light tap about 1 to 2 centimeters in diameter, reflecting the apex of the heart. 13. If the PMI is not where you would expect, as in a patient whose left ventricle is enlarged, inch your fingers along the fifth intercostal space until you feel the PMI. 14. Remember where you felt the PMI: over the apex of the heart in the fifth intercostal space at the left midclavicular line. 15. Warm the diaphragm of the stethoscope in the palm of your hand for 5 to 10 seconds. When it feels warm, clean it with alcohol and allow it to dry for 30 seconds. 16. Place the warmed diaphragm over the PMI, and auscultate for the normal S1 and S2 heart sounds of “lub-dub.” 17. Once you can hear S1 and S2 with regularity, look at your watch. When the second hand reaches a number on the dial (or when the digital display reaches a round number), start taking the pulse, counting the first beat you hear as “one.” If the apical pulse is regular, count the rate for 30 seconds and multiply the total by 2. The pulse rate normally ranges from 60 to 100 beats per minute. If the apical pulse is irregular or the patient is taking a cardiovascular drug, count for a full 60 seconds. Also, note the patterns of irregularity with any dysrhythmia, for example, if every third beat is skipped. 18. Replace the patient’s gown and bed linen, help the patient into a comfortable position, and discuss your findings if appropriate. 19. Clean the earpieces and diaphragm of the stethoscope with an alcohol swab routinely after each use, and discard the swab in an appropriate receptacle. 20. Place toiletries and personal items within reach. Copyright © 2014 by Mosby, an imprint of Elsevier Inc. All rights reserved. 2 21. Place the call light within easy reach, and make sure the patient knows how to use it to summon assistance. 22. To ensure the patient’s safety, raise the appropriate number of side rails and lower the bed to the lowest position. 23. Dispose of used supplies and equipment. Leave the patient’s room tidy. 24. Remove and dispose of gloves, if used. Perform hand hygiene. 25. As part of your follow-up care, compare the patient’s apical pulse rate and rhythm with the baseline and with the acceptable range for the patient’s age. 26. Document and report the patient’s response and expected or unexpected outcomes. Copyright © 2014 by Mosby, an imprint of Elsevier Inc. All rights reserved.