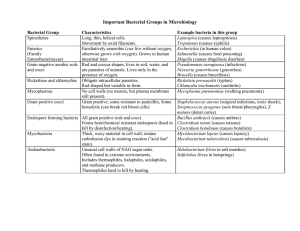
it woot i 1. What gram and catalase positive bacterial infection has a biofilm and is a cause of infections of catheters and prostheses? a. Staph aureus A endocarditis b. Staph saprophyticus c. Staph epidermidis d. MRSA Staph epidermidis Tagulase 2. What is the bacteria that causes syphilis and what stage presents with lymphadenopathy, condyloma lata (painless wart-like lesions), and a general widespread rash? disease a. Borrelia burgdorferi; stage 2 b. Leptospira; stage 1 c. Treponema pallidum; stage 2 d. Ureaplasma urealyticum, stage 3 go gym Treponema pallidum; stage 2 the É.mn 3. What bacterial infection is responsible for walking pneumonia in teens and young adults and what gram stain designation does it have? a. Mycoplasma pneumoniae; mycoplasma coolers b. Legionella pneumophila; gram negative Legionnaire's misterswater c. S. pneumoniae; gram positive 0M diplococcimeningitis d. Klebsiella pneumoniae; gram negativered jellylikesputum Mycoplasma pneumoniae; mycoplasma 4. What bacterial infection is responsible for the Bubonic plague and what gram stain is it? a. Yersinia enterocolitica; gram negative b. Yersinia enterocolitica; gram positive c. Yersinia pestis; gram positive d. Yersinia pestis; gram negative zoonotic blackdeath Yersinia pestis; gram negative grant hemorrhage 5. What gram negative bacteria is very motile; present in colon, soil, and water; and commonly causes UTIs and hospital acquired infection (nosocomial)? a. Staph saprophyticus b. Group D strep, Enterococcus c. Proteus mirabilis d. Bacillus cereus Proteus mirabilis 6. What strep organism is responsible for dental caries (cavities)? a. Group A strep, S. pyogenesx t b. Strep viridans gram viridans strep c. Group D strep, Enterococcus d. Strep pneumoniaePNA variablehemolysis biliaryUTI endocarditis e. Group B strep, S. agalactiae Strep viridans babies tests 353 weeks 7. A patient presents with fever, conjunctival redness, headache, and a palmar rash during the summer, which you believe to be Rocky Mountain Spotted Fever. Which of the following is the required vector? Rickettsiarickettsia a. Livestock b. Rats c. Mouse d. Dog e. Tick TickTickTickTick, Rickettsia rickettsii intracellular 8. a. b. c. d. e. 9. What is chandelier sign and what is it associated with? obligate Urethritis caused by Ureaplasma urealyticum Mycoplasma Cervical tenderness caused by Chlamydia trachomatis Neissetraammeningitidis Urethritis caused by Neisseria gonorrhoeae diplococci Urethritis caused by Chlamydia trachomatis Firm, ulcerated lesion caused by Treponema pallidum stage l Cervical tenderness caused by Chlamydia trachomati…. A patient presents with bloody diarrhea. Which of the following bacteria are known for causing this symptom? A. Enterotoxigenic E. coli diarrhea B. Neisseria gonorrhoeaejuggling C. Campylobacter jejuni t D. Helicobacter pylori t E. Vibrio cholerawater Égaiaitonach Campylobacter jejuni delineat listeria 10. 27-year-old woman presents to an urgent care center because of 6 days of increasing abdominal pain, bloating, and non-bloody diarrhea with four or five loose bowel movements per day. She has had mild nausea, but no vomiting and has been passing increased amounts of flatus. She has had no fever. Two weeks before onset of diarrhea, she went on a 3-day camping and rafting trip with her girlfriend, who is experiencing similar symptoms. Meds: Multivitamin with iron. • PE: T 36.6C BP 108/72 HR 110 RR 18 Abdomen is mildly distended with no guarding. Her abdomen is diffusely tender. Rectal exam demonstrates pale-colored stool, which tests negative for occult blood. Pelvic exam is normal. visible boilwater • What diagnostic tests are appropriate to send? Stool 3stooltest s cysts • How could this infection have been prevented? Boil watersterilizeH2O • What is the most likely diagnosis? Giardia giardia lamblia 11. A 19-year-old woman presents to the physician’s office for the evaluation of an itchy vaginal discharge that she has had for about a week. She has had no fever, abdominal pain, or dysuria. She became involved with a new sexual partner approximately 3 weeks ago. She takes birth control pills but does not regularly use condoms during intercourse. Her partner is asymptomatic. On examination, her vital signs are normal, and a general physical examination is unremarkable. On pelvic examination, her external genitalia are normal. After inserting a speculum you see a bubbly, thin, yellow vaginal discharge. Her cervix is erythematous but without discharge. She has no cervical motion or uterine or adnexal tenderness. A wet mount of the vaginal discharge examined microscopically reveals numerous motile, flagellated, pear-shaped organisms along with numerous white blood cells. writ strawberry • What is the most likely infectious cause of her vaginal discharge? TrichomoniasisTrichomoniasis vaginalis • What is the most likely source of her infection? New sexual partner (STI) unprotected sex 12. A 40-year-old man presents for a routine examination. He is generally feeling well but complains of some mild dysuria and increasing urinary frequency. He has never had a urinary tract infection (UTI) and thought that the increasing urinary frequency was a normal part of aging. He has not seen any blood in his urine but says that the urine does appear darker than it used to look. He has no other complaints, and his review of systems is otherwise entirely negative. He has no significant medical or family history. He smokes a pack of cigarettes a day and denies alcohol use. He is an immigrant from Ethiopia who has lived in the United States for 3 years. His vital signs and physical examination, including genital and prostate exams are normal. A urinalysis shows many red blood cells, a few white blood cells, and oval-shaped parasite eggs with terminal spines. w newpartner parasite UTI • What organism is the likely cause of his hematuria? Schistosomiasis haematobium schistosomiasis • How does this organism gain entry into humans? Skin haematobium skin 13. A patient presents with attacks of shaking chills and anemia. In exam you observe icterus and jaundice.You remember something about Sporozoites in the mosquito salivary gland and suspect Malaria, but which species would cause the most severe infection? A. Plasmodium vivax mosquito B. Plasmodium falciparum tx quinine resistance C. Plasmodium ovale D. Plasmodium malariae malarone Plasmodium falciparum 14. How do you diagnose malaria? A. Stool sample B. Wet Mount C. Giemsa peripheralblood D. Antibody detection Giemsa 15. A pregnant patient was cleaning the litter box and developed mono like symptoms. What infection is on the top of your differentials? Toxoplasma A. S. aureus B. Yersinia pestis C. Pasteurella D. Toxoplasmosis Toxoplasmosis 16. Kala-azar is transmitted by what and causes what? A. Sandfly; Leishmaniasis B. Mosquitoes; Maleria C. Kissing bug/Reduviid; American Trypanosomiasis Chaya's D. Tsetse fly; Trypanosoma sleeping sickness Sandfly; Leishmaniasis o 17. African Trypanosoma causes what symptom that can lead to death? A. Bladder cancer B. Sleeping sickness C. Myocarditis D. Red blood cell lysis Sleeping sickness 18. A patient presents with a chagoma on their arm. They also are positive for Romana’s sign. What disease do you suspect? A. Necator Americanus B. Ascaris Lumbricoides C. American Trypanosomiasis Chaya'sdisease D. Schistosomiasis swimmers itch American Trypanosomiasis O 19. What is the treatment for entamoeba? A. Metronidazole giardia entamoeba trichomoniasis B. Praziquantel C. Ivermectin D. Albendazole Metronidazole fdayil 20. Which is the most dangerous cestode? A. Taenia saginata T B. Taenia solium pigs C. Diphyllobothrium latum D. Yersinia enterocolitica Taenia solium yfish 21. What pathogen is transmitted from contaminated freshwater, invades through the skin, and is known as “swimmer’s itch”? A. Schistosomiasis B. Strongyloidiasis maturesinlungs C. Plasmodium vivax D. Vibrio cholera Schistosomiasis 22. This is transmitted through the fecal oral route and can be asymptomatic or perianal itching. The diagnosis is via the “scotch tape” test. A. Brucella B. Pthirus pubis crabs C. Enterobius Vermicularis pinworm D. Neisseria gonorrhoeae Enterobius Vermicularis 23. What organ is part of the maturation process of Strongyloidiasis? A. Lungs B. Duodenum C. Upper jejunum D. Urinary system Lungs 24. A patient has moved from a humid tropical region and comes in to see you. They are experiencing abdominal pain and persistent diarrhea. They are presenting with a cough, wheezing, and chronic bronchitis. Their skin is presenting with pruritus and urticaria. What is the most likely cause? A. Toxoplasmosis B. Trichomoniasis itching C. Strongyloidiasis D. Malaria Strongyloidiasis thives 25. You ate salmon and trout while on vacation in Europe. Now you have nausea, diarrhea, and weakness. What would be the best diagnostic test to identify the cause? A. Brain CT or MRI B. Abdominal US C. Fecal sample D. Colon biopsy Brain CT or MRI for Diphyllobothrium Latum Tiphyllobothrium 26. What nematode causes intestinal obstruction, peritonitis, biliary obstruction, and malnutrition? A. Plasmodium ovalex B. Trypanosoma C. Ascaris Lumbricoides D. Strongyloidiasis x Ascaris Lumbricoides 27. What stain can you visualize fungi with? A. Gram stain around B. India stain fungi halos C. Fluorescent stain D. Acid fast India stain 28. What do most antifungal agents work to disrupt? A. Ergosterol B. Cholesterol C. Polysaccharides D. Peptidoglycan Ergosterol 29. On physical examination you note hypopigmented or hyperpigmented patches on your patient after being in hot and humid weather. You do a KOH and discover “spaghetti and meatballs”. What do they have? A. Candida albicans yeasttmold B. Pityriasis versicolor dimorphic C. Coccidioides immitis D. Cryptococcosis Pityriasis versicolor O 30. Dermatophytes and candida are what type of fungal infection? A. Cutaneous B. Superficial C. Subcutaneous sporothrix schenkii s D. Systemic Cutaneous 31. You discover a red raised border of active inflammation with a central clearing on your body. What infection do you suspect? A. Cryptococcosis capitis B. Staph epidermidis C. Tinea corporis D. Treponema pallidum Tinea corporis 32. Wood’s light helps to diagnose which species? A. Microsporum B. Histoplasma capsulatum C. Candida blastomycosis URI D. Malassezia furfur Microsporum cutaneous Fjjjithoriverfallery systemic 33. You see an infant in your clinic and on physical exam note a diaper rash with “satellite lesions”. What is the most likely pathogen? A. Malassezia furfur B. Tinea cruris ampiggyperficial C. Sporothrix schenckii D. Candida albicans Candida albicans 34. You have a patient who enjoys gardening. He recalls getting stuck by a rose thorn and now has a skin infection on his hand that has become ulcerated and necrotic. What is the most likely pathogen? A. Sporothrix schenckii B. Coccidioidomycosis C. Cryptococcosis D. Histoplasma capsulatum opportunistic Sporothrix schenckii t systemic 35. A patient recently traveled to Ohio and explored a bat cave but avoided the forest. Now they have a pulmonary infection. What should be at the top of the differential diagnosis list? A. Coccidioidomycosis B. Leptospira Ipatisitlargest x silent disseminate itraconazole C. Ascaris Lumbricoides D. Histoplasma capsulatum blastomyces silent disseminate Histoplasma capsulatum systemic 0 fistplasma 36. The patient’s spouse from question 35 walks in and while in Ohio enjoyed nature hikes with decomposing wood and leaves. They are worried because of their spouse and want to get checked for any pathogens. What should you check for? A. Blastomyces dermatitidis spreadsto skint bones B. Coccidioidomycosis C. Epidermophyton D. Sporothrix Blastomyces dermatitidis 37. What is known as Valley Fever or Desert Rheumatism? A. Aspergillosis B. Mucormycosis C. Coccidioides immitis D. Cryptococcosis Coccidioides immitis 38. You have an AIDS patient that was cleaning pigeon droppings off their driveway. They stopped taking their fluconazole and now have meningitis. What is the most common life-threatening fungal disease you suspect as the cause associated with pigeon droppings? A. Pneumocystis jirovecii B. Mucormycosis opportunistic C. Cryptococcosis D. Aspergillosis Cryptococcosis all 39. You notice a patient starts coughing up brownish phlegm containing hyphae and the patient seems to be presenting with new onset asthma. What infection is causing it? A. Aspergillosis bronchiopulmonary aspergillosis fungalball B. Staph saprophyticus allergic steroids aspergilluma C. Mucormycosis oral antifing D. Strongyloidiasis Aspergillosis O 40. You get a new job in the burn unit. What fungal infection should you be on the look out for in your patients? A. Pneumocystis jirovecii B. Mucormycosis bloodvessels causeinfarction burnpatients C. Cryptococcosisstack D. Vibrio cholera Mucormycosis I 41. What is the most common opportunistic infection in AIDS patients that causes pneumonia? A. Sporothrix B. Cryptococcosis C. Pneumocystis jirovecii D. Coccidioidomycosis Pneumocystis jirovecii O 42. You ate rice and grains and now you have food poisoning. What spore, motile, exotoxin, aerobic, gram positive rod is wrecking your GI system? A. Clostridium difficile pseudomembranous B. Enterotoxigenic E coli Iwakylitfarrheat vibrio cholera C. Campylobacter jejuni bloody D. Bacillus cereus Bacillus cereus……... influenza med haemophilus otitis pneunno 43. A child presents with otitis media and you suspect a coccobacillus gram negative rod. Whatstrep bacteria is it? A. B. C. D. Moraxella catarrhalis Neisseria meningitidis dipplococci Vibrio cholera water diarrhea Corynebacterium membranein pharynx diptheria graypseudo Moraxella catarrhalis 44. A patient was cleaning the urine from their dogs and rats, but didn’t perform proper hygiene and had a skin abrasion. You see a spirochete hook under the microscope. What are they infected with? A. Borrelia burgdorferi B. Leptospira C. Treponema pallidum D. Rickettsia rickettsii Leptospira…………. i o tick 45. Your patient has a bullseye rash 10 days after hiking in the woods. You are worried about this disease causing neurologic damage in the late stage. What spiochete is causing this Lyme disease? A. Borrelia burgdorferi PNA B. Mycoplasma pneumoniae walking C. Mycoplasma leprae D. Atypical mycobacteria Borrelia burgdorferi…….. Tansey 46. A patient presents with a UTI that has dysuria and yellow discharge. You see the lab report it is a bacteria that in 60% of patients it’s normal flora and has no cell wall. What is the pathogen? A. E coli B. Proteus mirabilis C. Ureaplasma urealyticum D. Klebsiella pneumonia Ureaplasma urealyticum 47. Your AIDs patient reports fever, night sweats, and diarrhea. It’s an opportunistic infection that is an acid fast and aerobic rod. What is it? A. Atypical mycobacteria B. Chlamydia trachomatis C. Haemophilus influenzae D. Corynebacterium Atypical mycobacteria O Yobacterium 48. A college freshman presents with petechiae and meningitis. You suspect a gram negative diplococci rod with a capsule and is endotoxic (LPS). What is the cause? A. Listeria monocytogenes B. E coli meningitis C. Neisseria meningitidis D. Brucella Neisseria meningitidis peg at D rubella r 49. You observe a patient that coughs up currant jelly sputum. You recall from lecture that this is a gram negative rod that is enteric and can cause sepsis, UTI, and pneumonia. This infection is what? A. Vibrio cholera B. Bordetella pertussis C. Klebsiella pneumonia D. Legionella pneumonia Klebsiella pneumonia 50. A patient presents with Hansen disease and it’s an acid fast, aerobic infection. What is it? A. Mycobacterium leprae B. Leptospira C. Borrelia burgdorferi D. Clostridium perfringens Mycobacterium leprae Teprosy 51. The news reports a 0157:H7 outbreak from hamburger meat. What gram negative enteric rod is the source of this outbreak? A. Neisseria gonorrhoeae B. Listeria monocytogenes C. Brucella D. Enterotoxigenic E coli x enterohemorrhagic Enterotoxigenic E coli 52. Your patient has a chest x ray with caseous necrosis caused by an acid fast, obligate aerobic rod. What is it? A. S. pneumoniae B. Mycobacteria tuberculosis C. MRSA D. Bacillus anthracis Mycobacteria tuberculosis 53. You went to Chipotle and now you have rice water diarrhea. You’re picturing the little flagellum of the enteric gram negative rod and know the cause is fecal contaminated water. You have… A. Pasteurella multocida B. Proteus mirabilis C. Vibrio cholera D. Group D strep (Enterococcus) Vibrio cholera…………………. EMogbites 54. A senator was sent a letter that contained a spore forming gram positive rod that infects the lungs, skin, and intestines. What caused this? A. Staph saprophyticus B. S. aureus C. S. pneumoniae D. Bacillus anthracis Bacillus anthracis 55. While in the ED you notice a patient with lock jaw going into respiratory failure. What gram positive rod is causing this? A. Clostridium tetani B. Clostridium botulinum paralysis no musclecontraction C. E coli sepsis mostdangerous D. Corynebacterium diphtheria grantisepsis Clostridium tetani…………. O fluid 56. A patient presents with epiglottitis (which is an emergency) because they didn’t receive their HIB vaccine. What is causing this? A. Brucella B. Helicobacter pylori C. Haemophilus influenzae D. Viridans strep Haemophilus influenzae O 57. This gram positive cocci bacteria is catalase negative, part of the normal bowel, and can cause endocarditis and UTI. What pathogen is this? A. Group D strep (Enterococcus) B. S aureus C. MRSA D. Group A strep (S. pyogens) Group D strep (Enterococcus) 58. You woke up this morning with strep throat. You try to remember everything about it: gram positive, cocci, catalase negative, and beta hemolytic. What is the most likely pathogen? A. S. pneumoniae B. Group A strep (S pyogenes) C. Group B strep (S agalactiae) impetigo D. Viridans strep Group A strep (S pyogenes) O 59. What gram positive anaerobic rod causes gas gangrene? A. Enteroinvasive E coli B. Listeria monocytogenes C. Clostridium perfringens D. Haemophilus influenzae Clostridium perfringens o Tentizing fascitis 60. This gram negative enteric rod causes bright red bloody diarrhea and humans are it’s only host. A. Francisella tularensis B. Helicobacter pylori C. Klebsiella pneumonia D. Shigella Shigella…………………. 61. This gram positive cocci is catalase negative and beta hemolytic. It causes neonatal meningitis. A. Group B strep (S agalactiae) B. S aureus C. MRSA D. Staph saprophyticus Group B strep (S agalactiae) o 62. This gram positive diplococci has a polysaccharide capsule that can cause pneumonia, meningitis, and otitis media. What is it? A. MRSA B. Staph saprophyticus C. S pneumoniae D. Klebsiella pneumonia S pneumoniae 63. Infants are not supposed to have honey before the age of 1 because this anaerobic bacteria can block ACh. A. Clostridium tetani B. Clostridium difficile C. Corynebacterium diphtheria D. Clostridium botulinum Clostridium botulinum O 64. You see a gram negative enteric rod that is the most common cause of sepsis. What is it? A. MRSA B. S aureus C. Salmonella typhi D. E Coli sepsis E Coli sepsis O 65. There is an outbreak of contaminated cantaloupe and pregnant women are at high risk and it can cause neonatal meningitis. What is this gram positive non-spore forming rod? A. Brucella B. Bordetella pertussis C. Listeria monocytogenes D. Bacillus cereus Listeria monocytogenes 66. A patient presents with septic arthritis, cellulitis, and toxic shock syndrome. After wondering how they are still alive, you remembered from school that this is from a coagulase positive cocci cluster. What is it? A. MRSA B. S aureus C. S epidermidis D. Leptospira S aureus…. 67. A patient has traveler’s diarrhea similar to cholera. You’re smart and know you should also test for this. A. Pasteurella multocida B. Enterotoxigenic E coli C. Rickettsia rickettsii D. Atypical mycobacteria Enterotoxigenic E coli 68. You work in the hospital and notice your patient has developed HAP (hospital acquired pneumonia) that is resistant to penicillin G, gram positive, and cocci clusters. What is the most likely source of infection? A. S aureus B. E coli pneumonia C. MRSA D. S pneumoniae MRSA……………. o 69. This gram and catalase positive bacteria can cause UTI and is at risk of ascending to the bladder. A. Staph saprophyticus B. Vibrio cholera C. Klebsiella pneumonia D. Ureaplasma urealyticum Staph saprophyticus…... o 70. A patient presents with skin, conjunctiva, lung, and GI issues from eating infected milk products. What gram negative zoonotic is the most likely cause? A. Francisella tularensis B. Campylobacter jejuni C. Salmonella D. Brucella Brucella………………. 71. This is one of the most common bacterial infections in the United states and is a gram negative diplococci that contains pili. It causes neonatal conjunctivitis and PID. What is the pathogen? A. Neisseria gonorrhoeae B. Chlamydia trachomatis C. Leptospira D. Treponema pallidum Neisseria gonorrhoeae O 72. This enteric gram negative enteric rod causes bloody diarrhea and is an immune mediated inflammatory reaction. What is the most likely cause? A. Clostridium difficile B. Enteroinvasive E coli WBCsoRBCs C. Proteus mirabilis D. Pasteurella multocida Enteroinvasive E coli 73. You handled your chickens and didn’t wash your hands and ate some eggs Gaston style. Now you have gastroenteritis. What gram negative rod caused this infection? A. Brucella B. Yersinia pestis C. Vibrio cholera D. Salmonella Salmonella….. O 74. A patient has developed a UTI, you know the most common UTI is cause by this gram negative rod. A. Corynebacterium diphtheria B. E coli UTI C. Staph saprophyticus D. Group D strep (Enterococcus) E coli UTI…………………………... O 75. A patient was hanging out with their rabbits and developed ulceroglandular disease. You add the Bubonic plague and this gram negative zoonotic rod bacteria to your differential list. A. Mycobacteria tuberculosis B. Leptospira C. Borrelia pallidum D. Francisella tularensis Francisella tularensis……. 76. THis normal intestinal flora is motile and can cause hospital acquired infections and is a gram negative enteric rod. A. Brucella B. Enterobacter C. Vibrio cholera D. Shigella Enterobacter 77. This infection is stored in the gallbladder of chronic carriers and causes fever, headache, abdominal pain 1-3 weeks after exposure. A. Yersinia pestis B. Moraxella catarrhalis C. Clostridium tetani D. Salmonella typhi Salmonella typhi……. 78. This type of CAP (community acquired pneumonia) is found in AC units or other water environments. A. Legionella pneumophila B. Klebsiella pneumonia C. Mycoplasma pneumoniae D. E coli pneumonia Legionella pneumophila O 79. A gram positive anaerobic exotoxin bacteria that causes pseudomembranous colitis. A. Bacillus cereus B. Enterotoxigenic E coli C. Clostridium difficile D. Yersinia enterocolitica Clostridium difficile…... O 80. A patient got bite by their cat and they have developed a wound infection that you know not to suture. This gram negative zoonotic rod made you leery of shady cats. A. Bordetella pertussis B. Pasteurella multocida C. Borrelia burgdorferi D. Rickettsia rickettsii Pasteurella multocida 81. This cold surviving zoonotic is a gram negative rod that presents similar to Shigella and can be caused by pork. A. Yersina enterocolitica gastroenteritis B. Yersinia pestis C. Salmonella D. Clostridium difficile Yersina enterocolitica O 82. This bacteria has a vaccination and can cause death. It colonizes pharynx and forms a gray pseudo-membrane. It is a gram positive non spore forming rod. A. Moraxella catarrhalis B. Corynebacterium diphtheriae C. Klebsiella pneumonia D. Mycobacteria tuberculosis Corynebacterium diphtheriae 83. This is the cause of a type of hospital acquired pneumonia, is gram negative, a rod, and enteric. A. Mycobacteria tuberculosis B. Yersinia pestis C. E coli pneumonia D. Mycoplasma pneumoniae E coli pneumonia……………. 84. A patient presents with a whooping cough that destroys trachea and bronchi cells. It can be treated with azythromycin and is a gram negative rod. A. Brucella B. Bordetella pertussis C. Borrelia burgdorferi D. Corynebacterium diphtheriae Bordetella pertussis…………. 85. This bacterial infection causes duodenal and gastric ulcers and is a gram negative rod. A. Helicobacter pylori B. Campylobacter jejuni C. Vibrio cholera D. Pasteurella multocida Helicobacter pylori……. 86. This negative bacteria rod is a common cause of neonatal meningitis, where they are the most susceptible during the first month of life. A. S pneumoniae B. Neisseria gonorrhoeae C. Francesella tularensis D. E coli meningitis E coli meningitis………. o 87. Which of the following is NOT true of prions? A. Composed entirely of protein B. Disrupts neuron function C. Causes transmissible spongiform encephalopathies D. Causes pneumonia Answer: D 88. madcow T/F: Naked viruses undergo fusion whereas enveloped viruses are engulfed by a vesicle Answer: False F other wayaround 89. Which of the following is NOT a way to identify a virus? A. Light/ electron microscopy B. Gram Stain C. UV microscopy D. Tzanck smear herpeszoster E. ELISA Answer: B 90. A patient presents with URI symptoms, headache, malaise and fever. What is their broad diagnosis? A. Hepatitis B. Rabies C. Meningitis D. Pharyngitis Answer D 91. Which is NOT a type of Influenza? A. Influenza C B. Influenza D C. Influenza A D. Influenza B Answer: B 92. What is the incubation period for the flu? A. 7 days B. 14 days C. 2 days D. 4 days Answer: C 93. A patient reports fever, myalgia, headache, chills followed almost immediately by a dry, nonproductive cough. What is their likely diagnosis? A. Common cold by rhinovirus B. Croup from RSV C. Aids from HIV D. Mononucleosis from Epstein-Barr virus E. Influenza by Influenza virus Answer: E 94. The spread of the virus previously identified can be reduced through which antiviral? A. Acyclovir B. Cidofovir C. Famciclovir D. Oseltamivir Answer: D (common name Tamaflu) 95. The action of this drug is to prevent the newly formed virions from exiting the infected cell. Which viral glycoprotein is this then inhibiting? A. Hemagglutinin B. Neuraminidasepinging C. Both Answer: B tearing 96. Which of the following is NOT a disease that results in Exanthem? A. Fifth Disease B. Rotavirus C. Rubella D. Roseola E. Shingles F. Measles Answer: B 97. A patient presents with fever, malaise and a pruritic papulovesicular rash on trunk that spreads later to their head and legs. What is the condition/ virus involved? A. Rubella B. Measles C. Varicella D. Fifth Disease Answer: C 98. A patient presents with painful vesicles along a sensory nerve on their upper back. Which is the most likely condition or virus involved? A. Varicella B. Shingles C. Chicken pox D. Measles Answer: B 99. A patient presents with a fever, cough, conjunctivitis & coryza followed a couple days later by Koplik spots and then followed a day later by a rash that begins on the head and then spreads to the trunk, arms and legs. What is the most likely condition? A. Measles B. Chicken pox C. Fifth Disease D. Roseola Measles…... 100. T/F: Koplik spots are seen in the mouth. Answer: True mean 9989 101. A patient presents with a fever and then several days later has a faint maculopapular rash that spreads from their trunk to their arms and legs. Which virus causes this condition? (Bonus: What is the disease name?) A. Human Herpesvirus 6 roseola B. Varicella-zoster C. Paramyxovirus D. Togavirus Answer: A Bonus- Roseola 101. A patient presents with a swollen and tender salivary gland along with fever, malaise and anorexia. What is the condition? A. Measles B. Roseola C. Rubella D. Mumps Answer: D O 102. A patient presents with a low grade fever, URI symptoms, and lymphadenopathy followed a day later by a faint macular rash and petechial lesions on the soft palate. What is the most likely condition? A. Measles B. Mumps C. Rubella D. Roseola Answer: C 103. T/F: One big complication with the disease previously mentioned can result in fetal damage. Answer: True T 104. A patient presents with fever, malaise, headache, myalgias, lymphadenopathy, splenomegaly, mild leukopenia, anemia and an itchy confluent, indurated rash on the face. The rash progresses to a macular, reticular rash on the arms and legs the next day. What is the condition? A. Roseola B. Rubella C. Mumps D. Fifth Disease E. Chicken pox Answer: D 105. A patient presents with vomiting that began abruptly and lasted a couple days followed by brown watery diarrhea that lasted about a week. They also have a low-grade fever. Which virus is responsible for this condition? A. Hepatitis B. Rotavirus C. Norwalk Virus D. Roseola Answer: B 106. A patient states that they had vomiting & diarrhea that began abruptly and the condition lasted a couple days. Which virus is responsible for this condition? A. Norwalk Virus B. Rotavirus C. Mumps D. Hepatitis Answer: A 107. A patient presents with fever, anorexia, nausea, RUQ pain, jaundice, hepatomegaly, dark urine and clay-colored stools. What is the most likely diagnosis? A. Norwalk Virus B. Rotavirus C. Hepatitis A D. Hepatitis C Answer: C 108. A patient presents with fatigue, anorexia, nausea, RUQ pain/fullness, rash, clay-colored stools, dark urine and jaundice. What is the most likely diagnosis? A. Rotavirus B. Hepatitis D C. Hepatitis B D. Norwalk Virus Answer: C 109. A patient has previously been infected with Hep B and is an injection drug user. What chronic cirrhosis virus would be most common for your patient to contract? A. Hep A B. Hep C C. Hep D D. Hep E Hep D 110. This form of Hepatitis is transmitted via a fecal oral route and can be fatal in pregnancy when symptomatic. This form of Hep also lacks a vaccine. A. Hep A B. Hep B C. Hep D D. Hep E Hep E 111. This form of enterovirus causes abortive poliomyelitis, aseptic meningitis, and paralytic poliomyelitis. A. Poliovirus B. Togavirus C. Coxsackievirus D. Echovirus Poliovirus………. 112. This enterovirus is known to cause hand foot and mouth disease. A. Poliovirus B. Coxsackievirus C. Norwalk virus D. Rotavirus Coxsackievirus 113. Your patient presents with infantile hepatitis and hemorrhagic conjunctivitis. What enterovirus is infecting them? A. RSV B. Varicella zoster C. Roseola D. Echovirus Echovirus……. 114. Your patient presents with acute febrile illness, encephalitis, and meningitis after traveling to a tropical region. What family of viruses are you going to check for? A. Arboviruses B. Retroviruses C. Paramyxoviruses D. Parvoviruses Arboviruses……... O 115. You went hiking in Sedona with some friends over the summer. You meet up with them again and notice that your friend is having mental dysfunction interspersed with lucid periods. They seem to have increased salivation as well. You start to wonder if they had interaction with the random racoon you met on the trail that day. What virus are you worried your friend might have? A. COVID 19 B. Rabies C. Norwalk D. Rubella Rabies….. O 116. If a patient presents with fever, lethargy, sore throat, generalized lymphadenopathy, maculopapular rash (trunks, arms,legs), and leukopenia what acute stage virus should be at the top of your differential diagnosis list? A. B. C. D. O Rubella Mumps HIV Rotavirus HIV………… 117.Scarlet fever is a complication of streptococcal infection and is preceded by A. B. C. D. Pharyngitis Toxic Shock Syndrome Rheumatic fever Pneumonia A. Pharyngitis 118. The virus responsible for causing AIDS (HIV) is classified as a retrovirus. A retrovirus contains an RNA molecule and a protein that is required for the replication of the virus. This required protein is classified as a A. Histone B. Telomerase C. DNA polymerase D. Reverse transcriptase a. Reverse transcriptase 119. A 22-year-old sexually active man develops pain when he urinates. He also notices a discharge when he urinates. He goes to his family doctor. A Gram stain of the urethral discharge is done and intracellular diplococci are visualized. What is the most likely diagnosis? A. Primary syphilis B. Condyloma acuminatum C. Gonorrhea D. Herpes genitalis a. Gonorrhea 120. A 20-year-old pregnant woman presents at 21 weeks’ gestation with symptoms and signs of preeclampsia. Her symptoms have been present for the past 2 days. Prior to that, she had flu-like symptoms and a lace-like rash on her trunk and extremities and a flushed face. Intrauterine fetal demise was detected by ultrasonogram. Labor was induced, and a stillborn male fetus was delivered. Serum was collected for viral titers of the suspected agent that had caused the patient’s flu-like symptoms and fetal demise. The viral IgM titers were positive, as suspected. What is the most likely offending agent? A. Epstein-Barr virus B. Rotavirus C. Varicella-zoster D. Parvovirus B19 a. Parvovirus B19- aka 5ths disease 121. Which of the following are structurally most closely related to the influenza virus? A. B. C. D. E. Retroviridae Togaviridae Paramyxoviruses Coronaviridae Rhabdoviridae C. Paramyxoviruses 122. In malaria, the form of plasmodia that is transmitted from mosquito to human is A. B. C. D. Hypnozoite Sporozoite Merozoite Gametozoite B. Sporozoite 123. Which of the following is an enveloped RNA virus from the family Flaviviridae and is the major cause of post-transfusion hepatitis? A. Hepatitis A virus B. Hepatitis B virus C. Hepatitis C virus D. Hepatitis D virus Hepatitis C 124. Which of the following are non-motile enteric gram-negative bacteria with a very distinct polysaccharide capsule? This capsule is thought to interfere with immunologic reactivity of the organism. These bacteria are commonly associated with lobular pneumonia and can be highly resistant to antimicrobial agents A. Escherichia coli B. Klebsiella pneumoniae C. Neisseria meningitidis D. Shigella B. Klebsiella pneumoniae 125. Which of the following about Dimorphic fungi is correct? A. B. C. D. Are always non-pathogenic to humans Can grow as yeast at 37° C and as mold at 23° C Produces yeast forms at 23° C and motile rod forms at 45° C Does not reproduce asexually B. Can grow as yeast at 37° C and as mold at 23° C 126. Which of the following is true concerning leishmaniasis? a. b. c. d. Worldwide, it is estimated that there are approximately five million individuals with leishmaniasis Leishmaniasis is transmitted by phlebotomine sandflies Kala azar is caused by Leishmania mexicana The only known cure for diffuse cutaneous leishmaniasis is amphotericin B B. Leishmaniasis is transmitted by phlebotomine sandflies