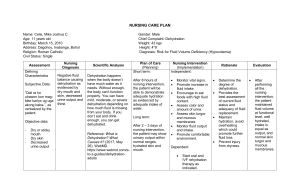
Unit 5 Review Concept Reading Sensory Perception/Pain Giddens: Chapter 28 Med Surg: Cataract pp 373-376 Med Surg: Glaucoma pp 379-382 Med Surg: Age Related Macular Degeneration pp 378 Med Surg: Conductive Hearing Loss pp 387391 Med Surg: Peripheral Neuropathy pp 11491150 Perry: Sensory Impairment pp 1032-1041 Elimination Giddens: Chapter 17 Med Surg: Obstructive Uropathies pp 10441049 Fluid & Electrolytes Giddens: Chapter 8 Med Surg: Fluid Volume Deficit and Fluid Volume Excess pp 270-283 Perry: Dehydration through Care Management pp 1255-1259 Mood & Affect Giddens: Chapter 33 Sensory Perception Cataract - MedSurg pp 373-376 ● Definition - opacity within the lens ○ May have cataract in one/both eyes ● Patho - mostly age related ○ Could be caused by - blunt/penetrating trauma, congenital factors (rubella), radiation/UV exposure, certain drugs (systemic corticosteroids/longterm topical corticosteroids), ocular inflammation ○ Pt with DM tends to develop cataracts at a younger age ● Clinical Manifestations ○ Decrease in vision ○ Abnormal color perception ○ Glare - due to light scatter caused by the lens opacities, and it may be significantly worse at night when the pupil dilates ○ Visual decline is gradual - rate varies ● Diagnostic Studies ○ Ophthalmoscopic ○ Slit lamp microscopic examination ○ Visual acuity measurement ○ Glare testing, potential acuity testing in selected patients ○ Keratometry and A-scan ultrasound (if surgery is planned) ● Interprofessional Care ○ Nonsurgical ■ Change in glasses prescription ■ Strong reading glasses/magnifiers ■ Increased lighting ■ Lifestyle adjustment ○ Surgical Therapy - when palliative measures no longer provide an acceptable level of visual function ■ Preop ● Cycloplegic agents/Mydriatic - to dilate the pupils ○ Instruct pt to wear dark glasses to minimize photophobia ○ Monitor for s/sx of systemic toxicity (tachycardia, CNS effects) ● Nonsteroidal antiinflammatory drugs ● Topical antibiotics ● Antianxiety meds ■ Surgery ● Removal of lens - lens-induced problems (IOP) may require this ● Phacoemulsification ● Extracapsular extraction Correction of surgical aphakia ● IO lens implantation (Most frequent) ● Contact lenses ■ Postop - unless complications occur, pt is usually ready to go home as soon as effects of sedation wear off ● Antibiotic drops ● Corticosteroid/antiinflammatory agent drops ● Mild analgesia (PRN) ● Eye patch/shield and activity as prescribed ● Pt should avoid activities that increase IOP (bending, stooping, coughing, or lifting) ● During each exam ○ Ophthalmologist measures pts visual acuity, checks anterior chamber depth, assesses corneal clarity, and measures IOP ● Nursing Management ○ Assessment ■ Pts distance and near visual acuity ■ If pt is undergoing surgery - note visual acuity in pt’s unoperated eye ■ Psychosocial impact of pt’s visual disability and level of knowledge regarding dz process and therapeutic options ■ Postop - assess pts level of comfort and ability to follow regimen ○ Planning ■ Preop - goals are that pt will make informed decisions regarding therapeutic options and experience minimal anxiety ■ Postop - goals are that pt will understand and comply with potop therapy, maintain acceptable level of physical/emotional comfort, and remain free of infection/other complications ○ Implementation ■ Health Promotion ● No proven measures to prevent cataracts ● Suggest pt wears sunglasses, avoids extraneous/unnecessary radiation, and maintain appropriate intake of antioxidant vitamins (C & E) ● Provide info about vision enhancement techniques for pt choosing not to have surgery ■ Acute Care ● Pupil dilation meds - produce transient stinging and burning ○ Photophobia - can be helped by dimming lights ● If eye patch is used - pt will not have depth perception until removed, so use special considerations to avoid falls/injuries ● If pain is intense pt should notify surgeon - may indicate hemorrhage, infection, or increase IOP ● Pt should notify surgeon if there is increased/purulent drainage, increased redness, or any decrease in visual acuity ○ Evaluation - overall expected outcomes are that the pt following cataract surgery will… ■ Have improved vision ■ Be better able to take care of self ■ Have minimal to no pain ■ Be optimistic about expected outcomes ○ Gerontologic Considerations ■ When elderly is visually impaired, pt may experience loss of independence, lack of control over life and a significant change in selfperception ■ They need emotional support and encouragement ■ Assure pt that cataract surgery can be accomplished safely and comfortably with minimal sedation Glaucoma - MedSurg pp 379-382 ● Risk Factors ○ Age ○ Genetics ○ African Americans ● Compare and Contrast ○ Primary Open-Angle Glaucoma (POAG) ■ Initial tx is with drugs - pt must understand continued tx and supervision are necessary because drugs control but do not cure glaucoma ■ Most common ■ Outflow of aqueous humor is decreased in the trabecular meshwork ■ Drainage channels become clogged ■ Damage to the optic nerve can result ■ Can develop slowly and without symptoms of pain or pressure ■ Symptoms ● “Tunnel vision” ■ Pt usually does not notice the gradual visual field loss until peripheral vision has been severely compromised ■ IOP - 22-32 ○ Primary Angle-Closure Glaucoma (PACG) ■ Acute PACG - emergency that requires immediate intervention ● Miotics and oral/IV hyperosmotic agents (glycerin liquid, isosorbide solution, and mannitol solution) are usually successful in immediately lowering the IOP ■ This one is worse ■ Usually caused by lens bulging forward ■ Due to a reduction in the outflow of aqueous humor ■ Sudden, excruciating pain in or around the eye ■ Result of aging ■ Mydriasis - pupils stay dilated (medical condition) ■ IOP - above 50 ■ Symptoms ● Blurred vision ● Nausea and vomiting ● Seeing colored halos around lights ● Ocular redness ● Clinical Manifestations ○ Primary Open Angle Glaucoma (POAG) develops slowly and without sx of pain or pressure. ■ Pt usually doesn’t notice gradual visual field loss until peripheral vision has been severely compromised ■ Eventually pt with untreated glaucoma has “tunnel vision,” in which only a small center field can be seen and all peripheral vision is absent ○ Acute angle-closure glaucoma causes definite sx - sudden, excruciating pain in or around the eye ■ Accompanied by nausea and vomiting, seeing colored halos around lights, blurred vision, and ocular redness ○ Subacute/chronic angle-closure glaucoma (CACG) appear more gradually. ■ Pt who has had a previous, unrecognized episode of CACG may report a history of blurred vision, seeing colored halos around lights, ocular redness, or eye or brow pain. ● Nursing Interventions ○ Primary focus is to keep IOP low enough to prevent pt from developing optic nerve damage ○ Educate ■ Safety ■ Risk of glaucoma and that it increases with age ■ Proper hygiene and eye care techniques to ensure that medications, dressings, and/or surgical wound is not contaminated during eye care ■ S/Sx of infection and when and how to report these ■ How to monitor pain, take pain medication, and report pain not relieved by medication ■ Importance of continued follow-up as recommended to maximize potential visual outcomes ■ Miotics - constricts the pupil -Warn patients about decreased visual acuity, especially in dim light. ■ Properly put eye drops in ● Pull bottom lid down ● Put head back ● Look up or away not at the drop ○ Stress importance of early detection and tx in preventing visual impairment ○ Current ophthalmic exam recommendation - every 2-4 years for people between 40-64 years and every 1-2 for people 65 and up ○ African americans should have exams more often because of higher risk ○ Assess ■ Pt’s ability to understand and adhere to rationale and regiment of prescribed therapy ■ Pt’s psychological reaction to dx of a potentially sight-threatening chronic disorder ○ Pt with acute angle-closure glaucoma requires immediate medication to lower the IOP ■ It must be administered in a timely and appropriate manner according to the ophthalmologist's prescription. ○ Most surgical procedures for glaucoma are outpatient procedures. ■ Pt needs postoperative instructions and may require nursing measures to relieve discomfort related to the procedure ■ Teach pt importance of complying with postop restrictions on head positioning, bending, coughing, and valsalva maneuver to optimize visual outcomes and prevent increased intraocular pressure ● Don’t lift heavy things, don’t bend over, don’t drive ○ Remind pt to follow the therapeutic regimen and follow-up recommendations prescribed by the ophthalmologist ■ Monitor IOP - pt will need regular check ups ○ Provide accurate info about the disease process and tx options, including the rationale underlying each option ○ PT needs information about the purpose, frequency, and technique for administration of antiglaucoma drugs ○ Encourage adherence by helping the patient identify the most convenient and appropriate times for medication administration or advocating a change in therapy if the patient reports unacceptable side effects. ● Diagnostic Studies ○ History and physical exam ○ Visual acuity measurement ○ Tonometry ○ Ophthalmoscopy (direct and indirect) ○ Slit lamp microscopy ○ Gonioscopy ○ Visual field perimetry ● Pharmacologic Interventions ○ Chronic Open-Angle Glaucoma ■ Beta-Adrenergic blockers ■ Alpha-Adrenergic agonists ■ Cholinergic agents (miotics) ■ Carbonic anhydrase inhibitors ■ Surgical Therapy ● Argon laser trabeculoplasty (ALT) - noninvasive option to lower IOP when meds are not successful/when pt cannot/will not use drug therapy as recommended ○ Outpt procedure requires only topical anesthetic ○ Laser stimulates scarring and contraction of trabecular meshwork causing the outflow channels to open ○ Most of the time reduces IOP ○ Pt uses topical corticosteroids 3-5 days after procedure ○ Most common postop complication - acute rise in IOP ○ Ophthalmologist examins pt 1 week and again 4-6 weeks after surgery ● Trabeculectomy with/without filtering implant - indicated if medical management and laser therapy are not successful ○ Acute Angle-Closure Glaucoma ■ Topical cholinergic agent ■ Hyperosmotic agent ■ Laser peripheral iridotomy ■ Surgical iridectomy ○ Patient will receive eye drops to decrease pressure ○ If pt had surgery he would have meds before, during, and after surgery Age Related Macular Degeneration - pp 378 ● Most common cause of irreversible central vision loss in people over 60 ● Two Forms of AMD: Dry vs Wet ○ Dry (nonexudative): ■ More common form (90% of all cases) ■ Close vision tasks are more difficult ■ Starts with the abnormal accumulation of yellowish extracellular deposits called drusen ■ Macular cells atrophy; leading to a slowly progressive and painless vision loss. ■ Can turn into wet ○ Wet (exudative): (Patients with wet AMD had dry AMD first.) ■ More severe form ■ Accounts for the majority of the cases of AMD-related blindness. ■ More rapid onset of vision loss ■ Characterized by growth of new BV in an abnormal location in the retinal epithelium ● Increased Risk Factors ■ Over 60 ■ White ethnicity ■ Family history of AMD ■ Chronic inflammation conditions ■ Smoking ■ Hypertension ● Diet ○ Dietary supplement of vit C, E, lutein, zeaxanthin, and zinc decreases progression of advanced AMD but has no effect on people with minimal AMD/those with no evidence of AMD ○ Eating lots of green, leafy veggies containing lutein (kale and spinach) may help reduce risk of AMD ● Clinical Manifestations ○ Blurred and darkened vision ○ Scotomas (blind spots in the visual field) ○ Metamorphopsia (distortion of vision) ● Diagnostic Studies ○ Amsler Grid Test - helps define involved area/provides a baseline for comparison ■ Do it every day ■ Hold 12-15 inch from face ■ Cover one eye with glasses and stare at the dot - if any lines like wavy, blurred, or bulging, that’s an indication that you may have macular degeneration and you need to call physician ○ Acuity measurement ○ Ophthalmoscopy - examiner looks for drusen (yellow deposits under the retina) and other fundus (Amsler grid test may help define the involved area, and it provides a baseline for future comparison) ○ Fundus photography and IV angiography with fluorescein and/or indocyanine green dyes ○ Optical coherence tomography (OCT) or scanning laser ophthalmoscopy ● Pharmacologic - limited treatment options for patients with wet AMD include several medications that are injected directly into the vitreous cavity. ○ Ranibizumab (Lucentis) ○ Bevacizumab (Avastin) ○ Aflibercept (Eylea) ○ Pegaptanib (Macugen) ■ Selective inhibitors of endothelial growth factor, helping to slow vision loss in wet AMD ■ Side Effects - blurred vision, eye irritation and pain, and photosensitivity ■ Injections are given 4-6 week intervals, depending on tx response ● Photodynamic Therapy (PDT) - uses verteporfin IV and a “cold” laser to excite the dye ○ Used in wet AMD and damages abnormal BV ○ Verteporfin - photosensitizing drug that becomes active when exposed to low-level laser light wave ■ Caution pts to avoid direct exposure to sunlight and other intense forms of light for 5 days after tx ■ Pts must be completely covered after tx because any exposure of skin to sunlight could activate the drug in that area, resulting in a chemical burn ● Interprofessional Care ○ Those at risk for advanced AMD should consider supplements of vitamins and minerals ○ Pts with low-vision assistive devices can continue reading and retain a license to drive during the day and at lower speeds Conductive Hearing Loss - MedSurg pp 387 ● Overview ○ Occurs when conditions in the outer or middle ear impair the transmission of sound through air to the inner ear ○ Common cause - otitis media with effusion. ○ Other causes - impacted cerumen, perforation of the TM, otosclerosis, and narrowing of the external auditory canal. ○ The audiogram demonstrates better hearing through bone than through air (airbone gap) ○ Pt often speaks softly because hearing own voice (which is conducted by bone) seems loud. This pt hears better in a noisy environment. ○ The first step - identify and tx the cause if possible. ■ If correction is not possible, a hearing aid may help if the loss is greater than 40 to 50 dB. ● Clinical Manifestation ○ Early signs ■ Answering questions inappropriately ■ Not responding when not looking at the speaker ■ Asking others to speak up ■ Showing irritability with others who do not speak up ■ Straining to hear, cupping the hand around the ear, reading lips, and an increased sensitivity to slight increases in noise level ○ Sudden Hearing Loss (sudden deafness) - occurs as an unexplained, rapid loss of hearing (usually in one ear) either at once or over several days. ■ This is a medical emergency and pt should see an HCP immediately ○ Often pt refuses to admit or may be unaware of impaired hearing ○ Irritability is common because the pt must concentrate so hard to understand speech. ■ The loss of clarity of speech in the pt with sensorineural hearing loss is most frustrating. Pt may hear what is said but not understand it. ■ Withdrawal, suspicion, loss of self-esteem, and insecurity are commonly associated with advancing hearing loss ● Tinnitus - perception of sound in the ears where no external source is present (“ringing in the ears” or “head noise”) ○ Sometimes the first sx of hearing loss, especially in older people. May be soft or loud, high pitched or low pitched. ○ Tinnitus and hearing loss are directly related. Both are caused by inner ear nerve damage ■ Main difference - the extent of the damage (tinnitus can still be heard) ○ Although the most common cause of tinnitus is noise, it can also be a side effect of medications ● Health Promotion ○ Noise - most preventable cause of hearing loss ■ Sudden severe loud noise (acoustic trauma) and chronic exposure to loud noise (noise-induced hearing loss) can damage hearing ■ Acoustic trauma causes hearing loss by destroying the hair cells of the organ of Corti ■ Sensorineural hearing loss as a result of increased and prolonged environmental noise (amplified sound) is occurring in young adults at an increasing rate. Amplified music (e.g., on iPods or MP3 players) should not exceed 50% of maximum volume. ■ Ear protection should be worn when firing a gun and during other recreational pursuits with high noise levels. ■ Teaching regarding avoidance of continued exposure to noise levels greater than 70 dB is essential ■ Occupational Safety and Health Administration (OSHA) standards require ear protection for workers in environments where the noise levels consistently exceed 85 dB. ● Periodic audiometric screening should be part of the health maintenance policies of industry. This provides baseline data on hearing to measure subsequent hearing loss. ○ Immunizations ■ Various viruses can cause deafness as a result of fetal damage and malformations affecting the ear ■ Promote childhood and adult immunizations, including the MMR vaccine ● Rubella infection during the first 8 weeks of pregnancy is associated with a high incidence of congenital rubella syndrome, which causes sensorineural deafness. ■ Women should avoid pregnancy for at least 3 months after being immunized. Immunization must be delayed if the woman is pregnant ○ Ototoxic Substances ■ Ototoxicity include salicylates, loop diuretics, chemotherapy drugs, and antibiotics ■ Chemicals used in industry (e.g., toluene, carbon disulfide, mercury) may damage the inner ear ■ The pt who is receiving ototoxic drugs/is exposed to ototoxic chemicals should be monitored for s/sx associated with ototoxicity (tinnitus, diminished hearing, and changes in equilibrium) ● If these sx develop, stop medication ● Assistive Devices and Techniques ○ Hearing Aids ■ If a hearing aid is indicated - should be fitted by an audiologist/speech and hearing specialist ■ Goal of hearing aid therapy is improved hearing with consistent use ■ Determine pt’s readiness for hearing aid therapy - acknowledgment of a hearing problem, pt’s feelings about wearing hearing aid, degree to which the hearing loss affects life, and any difficulties pt has manipulating small objects (putting a battery in a hearing aid) ■ First - the hearing aid should be restricted to quiet situations in the home. ● Pt must first adjust to voices and household sounds. ● Pt should also experiment by increasing and decreasing the volume as situations. ■ Then the environment can be expanded to the outdoors and then a shopping mall/grocery store. Adjustment to different environments occurs gradually, depending on the individual patient. ■ When the hearing aid is not being worn - should be placed in a dry, cool area where it will not be inadvertently damaged or lost ○ Speech Reading - “lip reading” ■ Pt is able to use visual cues associated with speech, such as gestures and facial expression, to help clarify the spoken message ■ Nonverbal Aids ● Draw attention with hand movements. ● Have speaker's face in good light. ● Avoid covering mouth or face with hands. ● Avoid chewing, eating, smoking while talking. ● Maintain eye contact. ● Avoid distracting environments. ● Avoid careless expression that the patient may misinterpret. ● Use touch. ● Move close to better ear. ● Avoid light behind speaker. ■ Verbal Aids ● Speak normally and slowly. ● Do not overexaggerate facial expressions. ● Do not overenunciate. ● Use simple sentences. ● Rephrase sentence. Use different words. ● Write name or difficult words. ● Do not shout. ● Speak in normal voice directly into better ear. ○ Sign Language - form of communication for people with profound hearing impairment. ■ Involves gestures and facial features such as eyebrow motion and lipmouth movements. ■ Sign language is not universal. ○ Cochlear Implant - hearing device for people with severe to profound sensorineural hearing loss in one or both ears. ■ Ideal candidate - one who has become deaf after acquiring speech and language ■ System consists of an external microphone placed behind the ear, a speech processor and a transmitter implanted under the skin that change sounds into electrical impulses, and a group of electrodes placed within the cochlea that stimulate the auditory nerves in the ear ■ Positive aspects - providing sound, improving lip-reading ability, monitoring loudness of the person's own speech, improving the sense of security, and decreasing feelings of isolation ● Profound Deafness - they may be assisted by text-telephone alerting systems that flash when activated by sound, closed captioning on television, and a specially trained dog. ○ The dogs are trained to alert their owners to specific sounds within the environment, thus increasing the person's safety and independence Sensory Impairment - Perry pp 1032-1041 (da damn babies) ● Hearing Impairment - general term indicating disability that may range in severity from slight to profound hearing loss ● Hearing Loss - may be caused by a number of prenatal and postnatal conditions ○ Family hx of childhood hearing impairment ○ Anatomic malformations of head/neck ○ Low birth weight ○ Severe perinatal asphyxia ○ Perinatal infection (cytomegalovirus, rubella, herpes, syphilis, toxoplasmosis, bacterial meningitis) ○ Maternal prenatal substance abuse ○ Chronic ear infection ○ Cerebral palsy ○ Down syndrome ○ Prolonged neonatal oxygen supplementation/administration of ototoxic drugs ○ Sounds loud enough to damage sensitive hair cells of the inner ear can produce irreversible hearing loss ○ Very loud, brief noise (e.g., gunfire) can cause immediate, severe, and permanent hearing loss ○ Longer exposure to less intense but still hazardous sounds (e.g., loud persistent music via headphones, sound systems, concerts, or industrial noises) may also produce hearing loss ● Classification of Sx Severity - hearing impairment is expressed in terms of a decibel (dB), a unit of loudness ○ Slight: 16-25 ■ Has difficulty hearing faint or distant speech ■ Usually is unaware of hearing difficulty ■ Likely to achieve in school but may have problems ■ No speech defects ○ Mild to Moderate: 26-55 ■ May have speech difficulties ■ Understands face-to-face conversational speech at 0.9 to 1.5 m (3 to 5 ft) ○ Moderately Severe: 56-70 ■ Unable to understand conversational speech unless loud ■ Considerable difficulty with group or classroom discussion ■ Requires special speech training ○ Severe: 71-90 ■ May hear a loud voice if nearby ■ May be able to identify loud environmental noises ■ Can distinguish vowels but not most consonants ■ Requires speech training ○ Profound: 91 ■ May hear only loud sounds ■ Requires extensive speech training ● Conductive Hearing Loss ○ Tx - depends on the cause and type of hearing impairment. ■ Many defects respond to medical/surgical treatment, such as antibiotic therapy for acute otitis media or insertion of tympanostomy tubes for chronic otitis media. ○ The nurse should be familiar with the types, basic care, and handling of hearing aids, especially when the child is hospitalized. ○ Types of Aids - those worn in or behind the ear, models incorporated into an eyeglass frame, and types worn on the body with a wire connection to the ear ○ Most common problems with a hearing aid is acoustic feedback - an annoying whistling sound usually caused by improper fit of the ear mold. ■ To reduce/eliminate whistling from a hearing aid, try removing and reinserting the aid, making certain that no hair is caught between the ear mold and the ear canal; cleaning the ear mold or ear; or lowering the volume of the aid. ● Sensorineural Hearing Loss ○ Children with sensorineural hearing loss have lost or damaged some or all of their hair cells or auditory nerve fibers ○ These children cannot benefit from conventional hearing aids because they only amplify sound that cannot be processed by a damaged inner ear. A cochlear implant bypasses the hair cells to directly stimulate surviving auditory nerve fibers so that they can send signals to the brain. ○ Treatment for sensorineural hearing loss is much less satisfactory. Because the defect is not one of intensity of sound, hearing aids are of less value in this type of defect. ● Care Management Identification of hearing loss before the first 3 months of age with intervention no later than 6 months of age is essential to improve the language and educational development for children with hearing impairments ○ Assessment of children for hearing impairment is a critical nursing responsibility ○ ○ At birth, the nurse can observe the neonate's response to auditory stimuli, as evidenced by the ■ Startle reflex, head turning, eye blinking, and cessation of body movement. ■ The infant may vary in the intensity of the response, depending on the state of alertness. However, a consistent absence of a reaction should lead to suspicion of hearing loss. ● Clinical Manifestations ○ Infants ■ Lack of startle or blink reflex to a loud sound ■ Failure to be awakened by loud environmental noises ■ Failure to localize a source of sound by 6 months of age ■ Absence of babble or voice inflections by 7 months of age ■ General indifference to sound ■ Lack of response to the spoken word; failure to follow verbal directions ■ Response to loud noises as opposed to the voice ○ Children ■ Use of gestures rather than verbalization to express desires, especially after 15 months of age ■ Failure to develop intelligible speech by 24 months of age ■ Monotone and unintelligible speech; lessened laughter ■ Vocal play, head banging, or foot stamping for vibratory sensation ■ Yelling or screeching to express pleasure, needs, or annoyance ■ Asking to have statements repeated or answering them incorrectly ■ Greater response to facial expression and gestures than to verbal explanation ■ Avoidance of social interaction; prefer to play alone ■ Inquiring, sometimes confused facial expression ■ Suspicious alertness alternating with cooperation ■ Frequent stubbornness because of lack of comprehension ■ Irritability at not making themselves understood ■ Shy, timid, and withdrawn behavior ■ Frequent appearance of being “in a world of their own” or markedly inattentive ○ When parents express concern about their child's hearing and speech development, refer the child for a hearing evaluation. Absence of well-formed syllables (da, na, yaya) by 11 months of age should result in immediate referral ○ ● Facilitating Lip Reading ○ Attract child's attention before speaking; use light touch to signal speaker's presence. ○ Stand close to child. ○ Face child directly, or move to a 45-degree angle. ○ Stand still; do not walk back and forth or turn away to point or look elsewhere. ○ Establish eye contact, and show interest. ○ Speak at eye level and with good lighting on speaker's face. ○ Be certain nothing interferes with speech patterns, such as chewing food or gum. ○ Speak clearly and at a slow and even rate. ○ Use facial expression to assist in conveying messages. ○ Keep sentences short ○ Rephrase message if child does not understand the words. ● Cued speech ○ The cued speech method of communication is an adjunct to straight lipreading. ○ Uses hand signals to help the hearing-impaired child to distinguish between words that look alike when formed by the lips (e.g., mat, bat) ○ Most commonly employed by hearing-impaired children who are using speech rather than those who are nonverbal ● Sign Language - Visual-gestural language that uses hand signals that roughly correspond to specific words and concepts in the English language ○ Encourage family members to learn signing, because using/watching hands requires much less concentration than lip reading/talking ● Speech Language Therapy - most formidable task in the education of a child who is profoundly hearing impaired is learning to speak. ○ Speech is learned through a multisensory approach using visual, tactile, kinesthetic, and auditory stimulation. ○ Encourage parents to participate ● Socialization - extremely important to children's development. ○ If children attend a special school for the hearing impaired, they are able to socialize with peers in that setting. ○ Classmates become a potential source of close friendships, because they communicate more easily among themselves. ● Support - Parents need extensive support to adjust to the shock of learning about their child's disability and an opportunity to realize the extent of the hearing loss. ○ If the hearing loss occurs during childhood, the child also requires sensitive, supportive care during the long and often difficult adjustment to this sensory loss. ○ Depression/anger is common these feelings are normal part of grieving process ● Care During Hospitalization ○ Verbal explanations must be supplemented by tactile and visual aids (books/actual demonstration and practice) ■ Children's understanding of the explanation needs to be constantly reassessed ○ Parents are encouraged to room with the child. Nurse must convey to them that this is not to serve as a convenience to the nurse but as a benefit to the child ○ Nurse can make boards by drawing pictures or writing the words on cardboard representing common needs (parent, food, water, or toilet) ○ Children with impaired hearing may have difficulty forming social relationships with other children - introduce the child to roommates and encourage them to engage in play activities ○ The hospital setting can provide growth-promoting opportunities for social relationships. ■ Child can learn new recreational activities, experiment with group games, and engage in therapeutic play. ■ Playing with puppets/dollhouses, role-playing with dress-up clothes, building with a hammer and nails, finger painting, and water play can help the child express feelings that previously were suppressed ● Visual Impairment - general term encompasses both partial sight and legal blindness ○ Partial sight/partial visual impairment - a visual acuity between 20/70 and 20/200 ○ Legal blindness/severe permanent visual impairment - a visual acuity of 20/200 or lower/a visual field of 20 degrees or less in the better eye ■ Legal blindness is not a medical dx but a legal definition ○ Visual impairment can be caused by a number of genetic and prenatal/postnatal conditions ■ Perinatal infections (herpes, chlamydia, gonococci, rubella, syphilis, toxoplasmosis) ■ Retinopathy of prematurity ■ Trauma ■ Postnatal infections (meningitis) ■ Disorders - sickle cell disease, juvenile rheumatoid arthritis, Tay-Sachs disease, albinism, and retinoblastoma ○ Refractive Errors - most common types of visual disorders in children. ■ Refraction - means bending and refers to the bending of light rays as they pass through the lens of the eye. Light rays enter the lens and fall directly on the retina. In refractive disorders, the light rays either fall in front of the retina (myopia) or beyond it (hyperopia) ○ Myopia (nearsightedness) - ability to see objects up close, not at a distance ○ Hyperopia (farsightedness) - ability to see objects at a distance, not up close ○ Astigmatism - unequal curvatures in refractive apparatus ○ Anisometropia - different refractive strength in each eye ○ Amblyopia (lazy eye) - reduced visual acuity in one eye ○ Strabismus - “Squint” or malalignment of eyes ○ Glaucoma - increased intraocular pressure ● Trauma - common cause of visual impairment in children ○ Penetrating wounds - most often a result of sharp instruments (e.g., sticks, knives, or scissors) ○ Propulsive objects (e.g., firecrackers, guns, arrows, or slingshots) ○ Nonpenetrating injuries may be a result of foreign objects in the eyes, lacerations, a blow from a blunt object such as a ball (baseball, softball, basketball, racquet sports) or fist, or thermal or chemical burns. ● Infections - of the adnexa and structures of the eyeball/globe may occur in children. ○ Most common eye infection is conjunctivitis. ○ Tx is usually with ophthalmic antibiotics - severe infections may require systemic antibiotic therapy ● Care Management ○ Discovery of a visual impairment as early as possible is essential to prevent social, physical, and psychologic damage to the child. Assessment involves ■ Identifying children at risk ■ Observing for behaviors that indicate a vision loss ■ Screening all children for visual acuity and signs of other ocular disorders (strabismus) ○ Infancy ■ Observe neonate's response to visual stimuli (following a light/object and cessation of body movement) ● Infant may vary in the intensity of the response, depending on the state of alertness. ■ Lack of eye contact from the infant must be taken seriously ■ During infancy, child should be tested for strabismus. ● Lack of binocularity after 2 to 4 months of age is considered abnormal and must be treated to prevent amblyopia (lazy eye) ○ Children ■ Most common visual impairment during childhood is refractive error, testing for visual acuity is essential ■ The school nurse usually assumes major responsibility for vision testing in schoolchildren ■ In addition to assessing for refractive errors, the nurse should be aware of s/sx that indicate other ocular problems ○ Promote Parent to Child Attachment ■ Crucial time in the life of visual impaired infants is when the infant and parents are getting acquainted with each other ■ Pleasurable patterns of interaction between the infant and parents may be lacking if there is not enough reciprocity ■ The nurse can help parents learn to look for other cues that indicate the infant is responding to them - whether the eyelids blink; activity level accelerates or slows; respiratory patterns change (faster or slower breathing, when the parents come near); and whether the infant makes throaty sounds when the parents speak to the infant ■ Encourage parents to show affection using nonvisual methods, such as talking or reading, cuddling, and walking the child ○ Promote the Child's Optimal Development ■ Motor development depends on sight almost as much as verbal communication depends on hearing ■ Parents are encouraged to expose the infant to as many visual-motor experiences as possible - sitting supported in an infant seat or swing and being given opportunities for holding up the head, sitting unsupported, reaching for objects, and crawling ■ Despite visual impairment, the child can become independent in all aspects of self-care ■ The permanently visual impaired child also must learn to become independent in navigational skills. ● Tapping method - use of a cane to survey the environment for direction and to avoid obstacles ● Guides - sighted human guide or a dog guide (seeing eye dog) ○ Play and Socialization ■ Children with severe permanent visual impairments do not learn to play automatically. ■ Because they cannot imitate others or actively explore the environment as sighted children do, they depend much more on others to stimulate and teach them how to play ■ Parents need help in selecting appropriate play materials, especially those that encourage fine and gross motor development and stimulate the senses of hearing, touch, and smell ■ Include these children with sighted children to help them adjust to the outside world for eventual independence. ■ To compensate for inadequate stimulation, these children may develop self-stimulatory activities, such as body rocking, finger flicking, or arm twirling. Discourage such habits because they delay the child's social acceptance. ○ Education ■ Main obstacle to learning is the child's total dependence on nonvisual cues. ■ Child can learn via verbal lecturing, they’re unable to read the written word/to write without special education - child must rely on braille ● Not useful for communicating with others unless they read braille ■ A recorder is especially helpful for leaving messages for others and taking notes during classroom lectures. For mathematic calculations, portable calculators with voice synthesizers are available. ■ Devices such as special plus lenses, handheld and stand magnifiers, telescopes, and video projection systems; and large print materials. Special equipment is available to enlarge print. To help with vision. ● Care for the Child During Hospitalization ○ Reassure the child and family throughout every phase of treatment ○ Orient the child to the surroundings ○ Provide a safe environment ○ Encourage independence. ○ Whenever possible, the same nurse should care for the child to ensure consistency ○ The child is encouraged to be independent in self-care activities, especially if the visual loss may be prolonged or potentially permanent. ■ During bathing, nurse sets up all of the equipment and encourages child to participate ■ At mealtimes, nurse explains where each food item is on the tray, opens any special containers, prepares cereal/toast, and encourages the child in self-feeding ● Assist in Measures to Prevent Visual Impairment ○ An essential nursing goal is to prevent visual impairment ○ Prenatal screening for pregnant women at risk (rubella/syphilis infection) and family histories of genetic disorders associated with visual loss ○ Adequate prenatal and perinatal care to prevent prematurity ○ Periodic screening of all children, especially newborns through preschoolers, for congenital and acquired visual impairments caused by refractive errors, strabismus, and other disorders ○ Rubella immunization of all children ○ Safety counseling regarding the common causes of ocular trauma, including safe practices when working with, playing with, and carrying objects such as scissors, knives, and balls Peripheral Neuropathy - MedSurg pp 1149-1150 ● Diabetic Nephropathy - microvascular complication associated with damage to the small blood vessels that supply the glomeruli of the kidney. ○ Leading cause of end-stage renal disease in the United States and is seen in 20% to 40% of people with diabetes. ○ Persistent hyperglycemia leads to an accumulation of sorbitol and fructose in the nerves that causes damage by an unknown mechanism. The result is reduced nerve conduction and demyelination ○ Most common type - sensory neuropathy. ■ Can lead to loss of protective sensation in the lower extremities, significantly increases the risk for complications that result in a lower limb amputation ● Risk Factors - hypertension, genetic predisposition, smoking, and chronic hyperglycemia ● Screening ○ Begins at the time of dx in pts with type 2 diabetes and 5 years after dx in pts with type 1 diabetes ○ Pyd with diabetes are screened for nephropathy annually with a random spot urine collection to assess for albuminuria and measure the albumin-to-creatinine ratio ○ Serum creatinine is also measured to provide an estimation of the glomerular filtration rate and thus the degree of kidney function ● Classification ○ Sensory Neuropathy (stocking-glove neuropathy) - distal symmetric polyneuropathy, which affects the hands and/or feet bilaterally ■ Signs and Symptoms ● Loss of sensation ● Abnormal sensations ● Pain - often described as burning, cramping, crushing, or tearing, ○ Usually worse at night and may occur only at that time ○ Foot injury and ulcerations can occur without the pt ever having pain ● Paresthesias - may be associated with tingling, burning, and itching sensations ● Pt may report a feeling of walking on pillows/numb feet. ● At times the skin becomes so sensitive (hyperesthesia) that even light pressure from bed sheets cannot be tolerated ● Complete/partial loss of sensitivity to touch and temperature ● Can also cause atrophy of the small muscles of the hands and feet, causing deformity and limiting fine movement ■ Managing blood glucose is the only tx for diabetes-related neuropathy ■ What's the drugs my dealaaa? ● Topical creams - capsaicin [Zostrix] ● Tricyclic antidepressants - amitriptyline ● SSRIs - duloxetine [Cymbalta] ● Antiseizure medications - gabapentin [Neurontin], pregabalin [Lyrica] ○ Autonomic Neuropathy - can affect nearly all body systems and lead to hypoglycemia unawareness, bowel incontinence and diarrhea, and urinary retention ■ Gastroparesis (delayed gastric emptying) - complication that can produce anorexia, nausea, vomiting, gastroesophageal reflux, and persistent feelings of fullness ● Can trigger hypoglycemia by delaying food absorption ■ Cardiovascular abnormalities associated with autonomic neuropathy are ● Postural hypotension (PH) ○ Assess pts for PH to determine risk for falls ○ Instruct the pt with PH to change positions slowly ● Resting tachycardia ● Painless myocardial infarction ■ Often the first sign in men w/diabetes - erectile dysfunction (ED) ■ ED/sexual dysfunction requires sensitive therapeutic counseling for both pt and pt’s partner ■ Neurogenic bladder may develop as the sensation in the inner bladder wall decreases, causing urinary retention ● Infrequent voiding ● Difficulty voiding ● Weak stream of urine ● Emptying the bladder every 3 hours in a sitting position helps prevent stasis and subsequent infection ● Complications of Feet and Lower Extremities ○ Sensory neuropathy and peripheral artery disease (PAD) are risk factors for foot complications ○ Sensory neuropathy is a major risk factor ○ Loss of protective sensation (LOPS) often prevents the pt from being aware that a foot injury has occurred ■ Annual screening using a monofilament is important. ● Done by applying a thin, flexible filament to several spots on the plantar surface of the foot and asking pt to report if it is felt ● Insensitivity to a monofilament has been shown to greatly increase the risk for foot ulcers that can lead to amputation ○ PAD increases risk for amputation by causing a reduction in blood flow to the LE ○ Signs of PAD - intermittent claudication, pain at rest, cold feet, loss of hair, delayed cap refill, and dependent rubor (redness of the skin that occurs when the extremity is in a dependent position) ■ The dz is dx by hx, ankle-brachial index (ABI) and angiography ○ If pt has LOPS/PAD - aggressive measures must be taken to teach the pt how to prevent foot ulcers, including ■ Selection of proper footwear (protective shoes) ■ Teach pt to carefully avoid injury to the foot, practice diligent skin and nail care, inspect the foot thoroughly each day, and treat small problems promptly Elimination Giddens - Chapter 17 ● Urinary Incontinence - disruption in the storage/emptying of the bladder with involuntary release of urine usually associated with dysfunction of the external and/or internal urinary sphincters ● Bowel Incontinence - involuntary passage of stool and ranges from an occasional leakage of stool while passing gas (flatus) to a complete loss of bowel control. ○ Can occur with diarrhea, particularly when it is associated with forceful intestinal peristalsis (cramping) ● Diet ○ High fiber foods: ■ Legumes (beans) ■ Cereals ■ Whole grains ■ Raw fruits & vegetables ○ Laxative effect foods: ■ Spicy & greasy ■ Bran/Chocolate ■ Coffee/Alcohol ■ Raw fruits & vegetables ● Lifespan Considerations ○ Child ■ Urine - incontinence (initially lack control over the sphincters and muscles that control urination and bowel elimination) ■ Bowel - constipation ■ Children are typically 18–24 months of age before they are able to identify the urge to urinate and defecate ○ Pregnant Client ■ Urine - increased frequency ● As the fetus grows, increased pressure is placed on the bladder, and frequent urination is required. ● The woman will have larger volumes of urine because she has a larger blood volume during the gestation ■ Bowel - constipation ● The growing fetus can also interfere with intestinal peristalsis and can cause constipation as well as prenatal vitamins ○ Older Adult ■ Urine - frequency & nocturia ● Bladder retains tone with age, the volume of urine that can be held reduces, leading to urinary frequency. ● Muscles around the urethra become weak, thus increasing the risk of incontinence ■ Incontinence - bowel/constipation ● Atrophy of smooth muscle layers in the colon and reduced mucous secretions ● Primary & Secondary Prevention ○ Primary Prevention ■ Hydration ■ Adequate dietary fiber ■ Regular toileting practices ■ Regular exercise ■ Avoidance of environmental contamination ○ Secondary Prevention ■ Colonoscopy screening ■ Occult blood screening ■ Prostate screening ● Incontinence Management ○ Bladder retraining ○ Pelvic floor muscle strengthening exercises ○ Timed and prompted voiding ○ Use of protective pads ○ Skin care ● Urinary Retention ○ Cause - external sphincter does not open for release of urine/blockage of urethra ■ Leads to increased urine volume and bladder distention and discomfort, backflow to UUT causes hydronephrosis (fluid in kidney), dilation of ureters and renal pelvis, can lead to pyelonephritis and renal atrophy. ■ If not outlet for urine it will destroy the kidneys - very imporant to attend too ○ Assessment - bladder distention & discomfort ○ Pt will complain of sense of fullness ○ Normal intake not a normal output ○ First thing - usually do a bladder scan, if more than 300ml they’re catheterized ● Pharmacotherapy - Urinary Elimination ○ Antibiotics - to kill bacteria ○ Antispasmodics - to relieve spasms ○ Cholinergics -increase muscle tone and tension ○ Analgesics - for UTIs ● Surgical Interventions - Urinary Elimination ○ Prostate surgery - relieve outflow obstruction ○ Bladder surgery ○ Urinary diversion - ileal conduit (do not confuse with ileostomy - liquid stool) ○ Surgery for renal calculi - to remove stones that create obstruction ○ Stents to relieve obstruction ● Urine Formation ○ Glomerular filtration GFR = amt of blood filtered per minute ○ Normal GFR: 120 ml/min. ● Pharmacotherapy - Bowel Elimination ○ Laxatives ○ Stool softeners ○ Antibiotics ○ Antispasmodics ○ Analgesics ● Surgical Interventions - Bowel Elimination ○ Bowel Diversion: Ileostomy or colostomy ● Nursing Management ○ Every shift assessment - ask when the last bowel movement was & its character ○ Educate on meds that can change bowel habits or character of stool ○ Instruct patients to not strain with BM ○ Ostomies - stoma assessment & appliance care Obstructive Uropathies - MedSurg pp 1044-1049 ● Urinary Obstruction - refers to any anatomic/functional condition that blocks/impedes the flow of urine. May be congenital or acquired ○ Obstruction at the level of the bladder neck or prostate - significant bladder changes can occur ○ Detrusor muscle fibers hypertrophy (increase in size) to contract harder to push urine out a narrower pathway. Over a long period, the detrusor loses its ability to compensate for this resistance, eventually leading to large residual urine volume in the bladder. ○ Bladder outlet obstruction - pressure increases during bladder filling/storage and can be transmitted to the ureter. ■ This pressure leads to reflux (backflow of urine) hydroureter (ureteral dilation and distention), vesicoureteral reflux (backflow [backward movement] of urine from the lower to upper urinary tract), and hydronephrosis ○ If only one kidney is obstructed, the other kidney may try to compensate by hypertrophy ○ Treatment - requires locating and relieving the blockage. ■ Insertion of a tube (e.g., urethral or ureteral), surgical correction of the primary problem, or diversion of the urinary stream above the level of blockage Urinary Calculi - Exemplar ○ Nephrolithiasis - kidney stone disease ○ Urolithiasis- stones formed in urinary tract outside the kidneys ○ Stone disorders are more common in men than in women. ○ Stone formation is more frequent in whites than in African Americans ○ Many factors are involved in the incidence and type of stone formation, including metabolic, dietary, genetic, climatic, lifestyle, and occupational influences ○ Crystals, when in a supersaturated concentration, can precipitate and unite to form a stone. Keeping urine dilute and free flowing reduces the risk of recurrent stone formation ● Risk Factors ○ Metabolic - abnormalities that result in increased urine levels of calcium, oxalate uric acid, or citric acid ○ Climate - warm climates that cause increased fluid loss, low urine volume, and increased solute concentration in urine ○ Diet ■ Large intake of dietary proteins that increases uric acid excretion ■ Excessive amounts of tea or fruit juices that elevate urinary oxalate level ■ Large intake of calcium and oxalate ■ Low fluid intake that increases urinary concentration ○ Genetic Factors ■ Family history of stone formation, cystinuria, gout, or renal acidosis ■ Lifestyle ■ Sedentary occupation, immobility ○ The higher the pH (alkaline), the less soluble are calcium and phosphate. ○ The lower the pH (acidic), the less soluble are uric acid and cystine. ■ When a substance is not very soluble in fluid, it is more likely to precipitate out of solution ● Types of Stones - the five major categories of stones (lithiasis) are (most common is calcium stones in combination of oxalate or phosphate) ○ Calcium phosphate - small enough to be trapped in ureter ○ Calcium oxalate - most common ○ Uric acid - predisposing factor may be gout (less common) ○ Cystine - genetic recessive defect (rare) ○ Struvite - usually related to UTI “infection stone” very jagged edges ○ If you have one kidney stone you are likely to have others ● Assessment ○ Past medical and surgical history ○ Medications - any meds to prevent stone ○ Diet - any excessive salt/calcium or fluid intake ○ Health Management - sedentary lifestyle is a contributing factor ○ Lifestyle ○ Voiding characteristics - what kind of s/ sx? Flank or groin pain, colic back pain, dysuria, anxiety? ○ Diagnostic findings ● Clinical Manifestations ○ First symptom usually is severe pain that begins suddenly ■ Person feels a sharp pain in the flank area, back, or lower abdomen ■ Described as “the most excruciating that a person can endure” ○ Renal colic - sharp, severe pain, which results from the stretching, dilation, and spasm of the ureter in response to the obstructing stone ■ Pts with renal colic have a hard time being still, they go from walking to sitting to lying down, and repeat (kidney stone dance) ○ Nausea and vomiting - due to severe pain ○ Stones cause clinical manifestations when they obstruct urinary flow ■ Type of pain is determined by the location of the stone ○ Men may experience testicular pain, Women may complain of labial pain, Both men and women may experience pain in the groin ○ The pt may also have manifestations of UTI with dysuria, fever, and chills ○ Cool moist skin ○ Patient can get rid of stone by drinking 2-3 quarts a day to help move stones along, and taking pain meds PRN ○ If pain is severe they will be hospitalized ○ Hematuria - result as damage to epithelium ● Diagnostic Studies ○ CT scan is commonly used in patients with renal colic - detects calcium and non calcium stones ○ Complete urinalysis helps confirm the diagnosis of a urinary stone by assessing for hematuria, crystalluria, and urinary pH ○ The patient's serum calcium, phosphorus, sodium, potassium, bicarbonate, uric acid, BUN, and creatinine levels are also measured (shows if patient is at risk for calculi) ○ History should include any previous episodes of stone formation, prescribed and OTC medications, dietary supplements, and family history of urinary calculi ○ Measurement of urine pH ■ Useful in the diagnosis of struvite stones and renal tubular acidosis (tendency to alkaline or high pH) ■ Uric acid stones (tendency to acidic or low pH) ○ Pts who experience recurrent stone formation should have a 24-hour urinary measurement of calcium, phosphorus, magnesium, sodium, oxalate, citrate, sulfate, potassium, uric acid, and total volume ○ IVP - can determine presence and location of obstruction - inject dye into arm into the vein, and taking x rays or CT images (no allergy to iodine or shellfish and not pregnant) ■ Make sure diabetic patient stops taking metformin for 48 hours to prevent damage to kidneys (combination of this and dye is dangerous for kidney) if patient needs coverage they will use insulin ■ No metformin for 24 hours or until results are back from procedure ■ Must push PO fluids and pt receives IV 1000ml before and after ● Interprofessional Care ○ First approach - management of the acute attack by treating the pain, infection, and/or obstruction ○ Administer opioids to relieve renal colic pain ○ Evaluation of the cause of the stone formation ○ Patient Education – adequate fluids, dietary changes, medication to prevent stone formation, control infection ○ Second approach - evaluation of the cause of the stone formation and prevention of further stone development ■ Family history of stone formation; geographic residence; nutritional assessment, including the intake of vitamins A and D; activity pattern (active or sedentary); history of prolonged illness with immobilization or dehydration; and any history of disease or surgery involving the GI or genitourinary tract ■ Treatment of struvite stones requires control of infection, acetohydroxamic acid may be used to treat kidney infections that result in formation of struvite stones. Acetohydroxamic acid inhibits the chemical action caused by the persistent bacteria ■ The stone may have to be removed surgically if the infection cannot be controlled (Endourology, lithotripsy, or open surgical stone removal) ● Stones too large for spontaneous passage (usually greater than 7 mm) ● Stones associated with bacteriuria or symptomatic infection ● Stones causing impaired renal function ● Stones causing persistent pain, nausea, or paralytic ileus ● Inability of patient to be treated medically ● Patient with only one kidney ○ Decrease sodium intake - when Na is abundant it increases Na in urine which increases Calcium in the urine, which leads to formation of stones ○ Don't stop eating calcium, no calcium preparation (no tums), no excess ○ Decreases oxalate - no, coffee chocolate tea and nuts ● Pharmacotherapy ○ Opioids ○ tamsulosin, terazosin -Relax smooth muscle (ureter) ○ thiazide diuretics ○ antimicrobials ○ acetohydroxamic acid ○ potassium citrate ○ Allopurinol- for uric acid stones, also used for gout ○ Flomax - is given to relax ureters and facilitate expulsion of kidney stones ● Endourologic Procedures ○ If the stone is located in the bladder, a cystoscopy is done ○ Large stones, a cystolitholapaxy is done ■ Large stones are broken up with an instrument called a lithotrite (stone crusher). The bladder is then irrigated and the crushed stones washed out ○ A cystoscopic lithotripsy uses an ultrasonic lithotrite to pulverize (break up) stones. ■ Complications with these cystoscopic procedures include hemorrhage, retained stone fragments, and infection. ○ Flexible ureteroscopes, inserted via a cystoscope, can be used to remove stones from the renal pelvis and upper urinary tract ○ Percutaneous nephrolithotomy, a nephroscope is inserted into the kidney pelvis through a track (using a sheath) in the skin. The stone fragments are removed, and the pelvis is irrigated. A percutaneous nephrostomy tube is usually left in place to make sure that the ureter is not obstructed. ■ Complications include bleeding, injury to adjacent structures, and infection. ● Lithotripsy ○ A procedure used to eliminate calculi from the urinary tract ■ Laser lithotripsy - is used to fragment ureteral and large bladder stones ■ Extracorporeal shock-wave lithotripsy (ESWL) - noninvasive procedure, pt is anesthetized, a high-voltage spark generator produces high-energy acoustic shock waves that shatter the stone without damaging the surrounding tissues. Stone is broken into fine sand/excreted in the urine. ■ Percutaneous ultrasonic lithotripsy - an ultrasonic probe is placed in the renal pelvis via a percutaneous nephroscope, probe produces ultrasonic waves, which break the stone into sandlike particles. ■ Electrohydraulic lithotripsy - probe is positioned directly on a stone, but it breaks the stone into small fragments that are removed by forceps/suction. ● A continuous saline irrigation flushes out the stone particles, and outflow drainage is strained so particles can be analyzed ○ Complications are rare but include hemorrhage, sepsis, and abscess formation ○ Postop - pt usually experiences moderate to severe colicky pain ○ First few times that the pt urinates, the urine is bright red and turns to dark red/smoky color (antibiotics are usually administered) ○ A self-retaining ureteral stent is often placed after the procedure to facilitate passage of sand - usually removed 2 weeks after procedure ● Surgical Therapy - primary indications for surgery are pain, infection, and obstruction ○ Type of open surgery performed depends on the location of the stone ■ Nephrolithotomy is an incision into the kidney to remove a stone ■ Pyelolithotomy is an incision into the renal pelvis for stone removal ■ If the stone is located within the ureter, a ureterolithotomy is performed ■ Cystotomy may be indicated for bladder calculi ○ Most common complications after surgical procedures - related to hemorrhage ● Nutritional Therapy ○ Drink adequate fluids to avoid dehydration (High urine output prevents supersaturation of minerals) ○ Limit consumption of colas, coffee, and tea because high intake of these beverages tends to increase the risk of recurrent urinary calculi ○ After an episode of urolithiasis, encourage a high fluid intake (approximately 3 L/day) to produce a urine output of at least 2 L/day ○ low-sodium diet is recommended Urinary Tract Calculi ● Always push fluids ● Strain urine before flushing ● Medicate pt for pain ○ Depending on the type of calculi, modify the diet to decrease foods that are high in the substance that is the cause of the calculi ○ Purin ■ High: Sardines, herring, mussels, liver, kidney, goose, venison, meat soups, sweetbreads ■ Moderate: Chicken, salmon, crab, veal, mutton, bacon, pork, beef, ham ○ Calcium ■ High: Milk, cheese, ice cream, yogurt, sauces containing milk; all beans (except green beans), lentils; fish with fine bones (e.g., sardines, kippers, herring, salmon); dried fruits, nuts; Ovaltine, chocolate, cocoa ○ Oxalate ■ High: Dark roughage, spinach, rhubarb, asparagus, cabbage, tomatoes, beets, nuts, celery, parsley, runner beans; chocolate, cocoa, instant coffee, Ovaltine, tea; Worcestershire sauce ● Planning - the overall goals are that pt with urinary tract calculi will have ○ Relief of pain ○ No urinary tract obstruction ○ Knowledge of ways to prevent recurrence of stones ● Nursing Implementation ○ Adequate fluid intake is important to produce a urine output of approximately 2 L/day ○ The moderately active, ambulatory person should drink about 3 L/day (tali and sarah). Fluid intake must be higher in the active person who works outdoors or who regularly engages in athletic activities (guess i don't need to drink much water) ○ Preventive measures for a person who is on bed rest or is relatively immobile (me) - maintaining an adequate fluid intake, turning the patient every few hours, and helping the patient sit or stand to maximize urinary flow ○ Dietary restriction of purines (fatty foods) may be helpful for pt at risk for developing uric acid stones ○ Teach pt the dosage, scheduling, and potential side effects of drugs used to reduce the risk of stone formation ○ Some pts may be taught to self-monitor urinary pH or urine output ○ Pain management and patient comfort are primary nursing responsibilities when managing a patient who has an obstructing stone and renal colic, any spontaneously passed stones are retrieved, strain all urine voided by the patient using a gauze or a urine strainer ○ Encourage ambulation to promote movement of the stone from the upper to the lower urinary tract ● Stricture - is a narrowing of the lumen of the ureter or urethra ● Ureteral Strictures ○ Can affect the entire length of the ureter, from the UPJ to UVJ ○ Secondary to adhesions or scar formation, or may be due to extrinsic factors such as large tumors in the peritoneal cavity. ○ Ureteral obstruction can threaten the function of the kidney. ○ Clinical Manifestations ■ Mild to moderate colic. Pain may be moderate to severe in intensity if the patient consumes a large volume of fluids (such as alcohol) over a brief period ■ Infection is unusual unless a calculus or foreign object such as a stent or nephrostomy tube is present ■ Ureteral stricture may be temporarily bypassed by placing a stent ● Urethral Strictures ○ Result of fibrosis or inflammation of the urethral lumen ○ Causes - trauma, urethritis (particularly after gonococcal infection), surgical intervention or repeated catheterizations, or a congenital defect of the urethra ○ Clinical Manifestations ■ Diminished force of the urinary stream, straining to void, sprayed stream, post void dribbling, or a split urine stream ■ The patient may report feelings of incomplete bladder emptying with urinary frequency and nocturia ■ Moderate to severe obstruction of the bladder outlet may lead to acute urinary retention ■ The patient may report a history of urethritis, difficulty with insertion of a urinary catheter, or trauma involving the penis or the perineum ○ Treatment initially is based on dilation. Recurrences may necessitate selfcatheterization or surgery. ● Renal Trauma ○ Renal trauma may occur from violent crimes, traffic accidents, falls, and sports injuries. The severity of the trauma depends on the extent of injury. ○ Treatments range from bed rest, fluids, and analgesia to surgical repair and nephrectomy ● Diet for Pediatric Diarrhea: BRAT - Bananas, rice, apple sauce, and toast Fluid and Electrolytes Powerpoint Part 1 ● Fluid volume deficit - isotonic loss of water and electrolytes ● Fluid volume excess - isotonic gain of water and electrolytes ● Dehydration - hyperosmolar loss of water only ○ Person has lost water but not electrolytes ● Overhydration - hypoosmolar gain of water only ● Hypovolemia - loss of serum and blood constituents ● Osmosis - movement of fluid (solvent) from an area of lower solute concentration to an area of higher solute concentration ● Diffusion - movement of molecules and ions (solutes) from an area of higher concentration to an area of lower concentration ● Filtration - movement of fluid across a membrane, under pressure, from higher to lower pressure ○ Hydrostatic pressure - pushing force ○ Osmotic pressure - pulling force ○ Intravenous fluid therapy can manipulate either one of these pressures ■ Ex. - giving albumin IV to a client with ascites ● Ascites is in the interstitial space where it is very resistant when going back into intravascular compartment ● Albumin - protein, because they are so large they draw fluid into the vascular compartment and then they urinate it out ● Active Transport - movement of ions from low to high concentration ○ ATP is required as an energy source ● Body Compartments ○ First spacing - normal distribution of ICF and ECF ○ Second spacing - abnormal accumulation of fluid in interstitial space ■ Edema ○ Third spacing - abnormal collection of fluid in area between cells which is resistant to movement back into ICF/plasma ■ Ascites ● Fluid Regulation by Hormones ○ ADH - restores the blood volume by decreasing diuresis and increasing water retention ○ Aldosterone - causes the retention of water and sodium ● Factors Affecting Body Fluid ○ Age - changes tolerated poorly in infants and elderly ■ Infants have higher metabolism than adults/elderly and they lack the ability to concentrate urine - highest risk of dehydration ● So much of their body is made of fluid so any kind of change in their fluid composition impacts them severely ■ Elderly are second highest risk of dehydration - less muscle mass and decreased thirst drive ● Structural changes in their kidneys decreasing ability to reserve water ● Kidneys aren’t working as well ○ Gender - men have greater muscle mass which holds water ○ Body size - heavier people have increased fat which stores less water ■ Tendency to lean more to dehydrated side ○ Environment - heat causes higher water and sodium loss ○ Lifestyle ● Water intake is regulated by thirst which is triggered by receptors in the hypothalamus that respond to increased plasma osmolality or decreased fluid volume ● 20% fluid loss in adult is fatal ● S/Sx of Dehydration - Adult v. Children ○ Older adults and Children ● Elderly - Naturally have less volumes of water in their body and may take meds or have certain conditions that increase risk of dehydration ■ Headache ■ Dizziness ■ Thirst ■ Dry mouth ■ Crankiness ■ Dark colored urine ■ Dry skin ■ Constipation ○ Infants ■ Common cause of dehydration is severe diarrhea and vomiting ■ Fever may occur during dehydration but it is also the cause of it ■ Unusual tiredness ■ Crying without tears ■ Dry mouth ■ No/very few wet diapers (for 3 hours or longer) Fluid Volume Deficit and Fluid Volume Excess - MedSurg pp 270-283 ● Fluid Volume Imbalances ○ Fluid Volume Deficit (FVD) - can occur with abnormal loss of body fluids (diarrhea, vomiting, hemorrhage, polyuria), inadequate fluid intake, or plasma to interstitial fluid shift ■ Dehydration - water loss with hypernatremia ● Causes - excessive water losses (skin, GI, or kidneys); inadequate fluid intake, diabetes, third-space fluid shifts (burns, pancreatitis), hemorrhage, overuse of diuretics ■ Manifestations ● Increased serum osmolality - increased sodium ● Increased H&H (hemoglobin and hematocrit) ● Increased temp ● Decreased BP ● Increased HR ● Concentrated urine ● Decreased output ● Weakness/dizziness ● Restlessness, drowsiness, lethargy, and confusion ● Poor skin turgor ● Dry mucous membranes ● Flat veins in hands ● Loss of weight ■ Managing ● Correcting underlying cause and replacing both water and any needed electrolytes ● Replacement therapy depends on severity and type of volume loss ● Mild losses - oral rehydration is used ● Severe losses - volume is replaced with blood products/balanced IV solutions (isotonic sodium chloride/lactated Ringer’s solution) ● For rapid volume replacement - 0.9% sodium chloride is preferred ● Blood is administered when volume loss is due to blood loss ○ Fluid Excess (ECV Excess aka FVE) ■ Causes - excessive isotonic/hypotonic IV fluids, heart/renal failure, primary polydipsia, SIADH, Cushing syndrome, long-term use of corticosteroids ■ S/Sx ● Headache, confusion, lethargy ● Decreased serum osmolality ● Decreased H&H ● Peripheral edema ● Increased BP ● Bounding pulse ● Polyuria ● Dyspnea, crackles, pulmonary edema ● Bright yellow urine ● Increased output ● Seizures, coma ● Muscle spasms ● Jugular venous distention ● Increased weight ■ Managing ● Tx underlying cause and remove fluid without producing abnormal changes in the electrolyte composition/osmolality of ECF ● Primary forms of therapy - diuretics and fluid restrictions ● If it leads to ascites/pleural effusion - abdominal paracentesis/thoracentesis may be needed ● Nursing Implementation ○ Daily Weights - most accurate measure of volume status ■ Weigh pt at the same time every day, wearing the same garments and on the same carefully calibrated scale ■ Remove excess bedding and empty all drainage bags before weighing ○ Measure all fluids I&Os ■ Intake - oral, IV, and tube feeding and retained irrigants ■ Output - urine, excess perspiration, wound/tube drainage, vomitus, and diarrhea ■ Estimate fluid loss from wounds/perspiration ■ Note amount and color of urine and measure urine specific gravity (>1.025 indicate concentrated urine; <1.010 indicate dilute urine) ○ Check lab values ■ Fluid volume deficit - as pt is rehydrated, labs will get back to normal ● Increased BUN, sodium, H&H, and plasma and urine osmolality ■ Fluid volume excess ● Decreased BUN, sodium, H&H, and plasma and urine osmolality ○ Assess cardiovascular system ■ Monitor VS ■ Changes in BP, central venous pressure, pulse force, and jugular venous distention reflect ECF volume imbalances ■ Fluid volume excess - pulse is full, bounding, and not easily obliterated ● Increased volume causes distended neck veins, increased central venous pressure, and high BP ■ Fluid volume deficit (mild-moderate) - SNS compensates increasing the heart rate and causes vasoconstriction in effort to maintain BP ● Pulses may be weak and thready ● Assess for orthostatic changes ● More severe - hypotension may be present ○ Assess respiratory system - hydration is important in order to thin and clear secretions ■ ECF Excess - results in pulmonary congestion and pulmonary edema ● Pt will experience shortness of breath and moist crackles on auscultation ■ ECF Deficit - increased respiratory rate because of decreased tissue perfusion and hypoxia ● Administer O2 as ordered ○ Pt Safety - fluid volume deficit is at risk for falls because of orthostatic hypotension, muscle weakness, and changes in level of consciousness. ■ Assess LOC, gait, and muscle strength ○ orientation, vision, hearing, reflexes, and muscle strength ○ Assess for skin breakdown and good oral care ■ Lack of fluid increases chance of skin break down - check for skin turgor ■ In ECF volume deficit, skin turgor is diminished, and there is a lag in pinched skinfolds ■ In elderly, skin turgor is less predictive of fluid deficit ■ Mild Fluid Deficits - skin may appear warm, dry, and wrinkled ■ Severe deficits - skin may be cool and moist ● Dry oral mucous membranes, furrowed tongue, and pt will often complain of thirst ● Routine oral care is critical for comfort of a pt who is dehydrated/on fluid restrictions ■ Assess edema be pressing with a thumb/forefinger over tibia, fibula, or sacrum (best places to assess for pitting edema) ■ Dehydrated skin needs frequent care w/o the use of soap. Apply moisturizing creams/oils to increase moisture retention and stimulate circulation ○ Fluid Therapy - Fluid Volume Deficit ■ Administer IV fluids as ordered ■ Carefully monitor the rates of infusion of IV fluid solutions ■ Assess pt’s ability to obtain adequate fluids independently, express thirst, and swallow effectively ■ Fluids should be easily accessible ■ Provide a variety of fluids the pt likes ■ Serve fluids at a temp preferred by pt ■ Offer fluids every 1-2 hours and at select times (when admin. meds) ■ Remind pt to finish all drinks ■ If pt is choosing to limit intake to decrease nocturia/incontinence - make it easier to reach toilet ● Clinical Management ○ Primary ■ Dietary measures ■ Adequate intake with diarrhea/vomiting ■ Limiting intake when prone to edema ■ Fluid management ○ Collaborative Care - dehydration ■ Sodium restriction due to hypernatremia pt has ● Hypernatremia is corrected when given isotonic IV fluids ■ Goal is to restore water losses ○ Collaborative Care - FVE ■ Pt will have dilutional hyponatremia - as you give diuretics to get rid of fluids they will go back to normal amount of sodium and water ■ Goal is to restore homeostasis ● Hypernatremia - may occur with inadequate water intake, excess water loss, or (rarely) sodium gain (>145mEqL) ○ Hypernatremia causes hyperosmolality - this causes water to move out of the cells to restore equilibrium, leading to cellular dehydration ■ Primary protection against development of hyperosmolality is thirst ○ Hypernatremia secondary to water deficiency is often the result of an impaired LOC/inability to obtain fluids ○ Clinical Manifestations - alterations in mental status, ranging from agitation, restlessness, confusion, and lethargy to coma ■ If there is accompanying ECF volume deficit, postural hypotension, tachycardia, and weakness occur ■ Increased temperature, HR, BP, thirst ○ Nursing Implementation ■ Managing hypernatremia depends on the underlying cause ■ Primary water deficit - fluid replacement is provided orally/IV with isotonic (0.9% sodium chloride) ■ Sodium excess - dilute the high sodium concentration with sodium-free IV fluids (5% dextrose in water) and promote sodium excretion with diuretics ● Dietary sodium intake is often restricted ■ Monitor serum sodium levels, serum osmolality, and pt’s response to therapy ■ Serum sodium level should not decrease more than 8-15 mEq/L in an 8hour period ● Quickly reducing levels can cause a rapid shift of water back into cells, resulting in cerebral edema and neurologic complications ■ Give Hypotonic IV fluid ■ D5W isotonic ● Hyponatremia - may occur from a loss of sodium-containing fluids, water excess in relation to amount of sodium, or a combo of both ○ <135mEq/L ○ Usually associated with ECF hypoosmolality from the excess water ○ To restore balance, fluid shifts out of the ECF and into the cells, leading to cellular edema ○ Clinical Manifestations - first appear in the CNS ■ Mild - headache, irritability, and difficulty concentrating ■ Severe - confusion, vomiting, seizures, and even coma ● If this develops rapidly, irreversible neurologic damage/death from brain herniation can occur ■ Confusion, increased HR, decreased BP ○ Nursing Implementation ■ From fluid loss - replace fluids using isotonic sodium-containing solutions, encourage oral intake, and withhold all diuretics ■ Mild by water excess - fluid restriction is often the only tx ● Aim of restriction is 500mL less than previous 24-hour urine output ● Loop diuretics and demeclocycline may be given ■ Acute/More serious - small amounts of IV hypertonic saline solution (3% sodium chloride) can restore serum sodium levels while body is returning to a normal water balance ■ Vasopressor receptor antagonists (drugs that block ADH) are used to tx pts who cannot tolerate fluid restrictions/have more severe sxs ■ Monitor serum sodium levels and pts response to therapy to avoid rapid/overcorrection ● Level should not increase 8-12 mEq/L in the first 24 hours ● Quickly increasing levels of sodium can cause osmotic demyelination syndrome with permanent damage to nerve cells in the brain ○ Accurate urine output record is essential ■ Give hypertonic IV fluids and restrict fluids ● Hyperkalemia - may occur from impaired renal excretion, a shift of potassium from ICF to ECF, a massive intake of potassium, or a combo ○ Most common cause is renal failure ○ Other causes are Acidosis, trauma or injury ○ Digoxin-like drugs and Beta-adrenergic blockers can impair entry of potassium into cells ○ Heparin, potassium-sparing diuretics, angiotensin II receptor blockers, and ACE inhibitors can contribute to hyperkalemia by reducing kidney’s ability to excrete potassium ○ ○ Clinical Manifestations - most clinically significant problems are the disturbances in cardiac conduction ■ Initial finding is tall, peaked T waves ■ As potassium increases, cardiac depolarization decreases - loss of P waves, prolonged PR interval, ST segment depression, and widening QRS complex ● Heart block, v-fib, or cardiac standstill may occur ■ Fatigue, confusion, tetany, muscle cramps, paresthesias, and weakness ■ Loss of muscle tone and weakness/paralysis of other skeletal muscles, including the respiratory muscles can occur, leading to respiratory arrest ■ Abdominal cramping, vomiting, and diarrhea occur from GI hyperactivity ○ Nursing Implementation ■ Eliminate oral and parenteral potassium intake ■ Increase elimination of potassium - loop/thiazide diuretics, dialysis, patiromer, and/or sodium polystyrene sulfonate (Kayexalate) ● Patiromer - best for pts with chronic hyperkalemia ○ Give within 6 hours of other drugs ● Kayexalate - orally/rectally, each gram removes roughly 1mEq of potassium ○ It will give body Na ions and take K ions in return, causes diarrhea - you want patient to have diarrhea ■ Force potassium from ECF to ICF - combo of IV regular insulin and betaadrenergic agonist stimulates sodium-potassium pump ■ Stabilize cardiac membrane - IV calcium chloride/calcium gluconate ● Mild Hyperkalemia - eliminate oral potassium intake and increase elimination of potassium (diuretics) ● Severe Hyperkalemia - receives tx to force potassium into cells ■ Continuous ECG monitoring of all pts to detect dysrhythmias and monitor the effects of therapy ■ Pt experiencing dangerous cardiac dysrhythmias should receive IV calcium immediately ● Monitor BP - rapidly administering calcium can cause hypotension ■ When admin insulin - monitor for hypoglycemia and give glucose as needed ● Hypokalemia - increased loss of potassium, an increased shift of potassium for ECF to ICF, or from deficient dietary potassium intake (rarely) ○ Most common cause are abnormal losses from the kidneys/GI tract ○ Clinical Manifestations - hyperpolarization and impaired muscle contraction ■ Cardiac changes - impaired repolarization resulting in flattened T wave, depressed ST segment, and presence of U wave ● P waves peak and QRS complex is prolonged ● Increased incidence of heart block and potentially lethal ventricular dysrhythmias ■ Skeletal muscle weakness and paresthesias may occur ■ Severe - can cause paralysis ● Usually involves extremities ● Can involve respiratory muscles leading to shallow respirations and respiratory arrest ■ Impairs insulin secretion - glucose intolerance and hyperglycemia ■ Orthostatic hypotension ■ Decreased bowel sounds ○ Nursing Implementation ■ Oral/IV potassium chloride (KCl) supplements and increased dietary intake of potassium ■ Consuming potassium-rich foods can usually correct mild hypokalemia ■ Significant hypokalemia requires admin oral/IV KCl ● IV KCl infusion rates should not exceed 10 mEq/hr unless pt is in critical care setting with continuous ECG monitoring and central line access for admin ● Must be given by infusion pump to ensure correct edmin rate ● Assess IV sites at least hourly for phlebitis and infiltration (K+ irritates vein, might have to change IV location) ■ Pts critically ill and at risk for hypokalemia should have continuous monitoring to detect cardiac changes ■ Monitor serum potassium levels and urine output ■ Pts on digoxin therapy have increased risk of toxicity if theri serum potassium level is low - monitor for digitalis toxicity ■ Pts at risk should have regular serum potassium levels monitored ■ Teach pt taking digitalis to report s/sx of digoxin toxicity to HCP ■ Pt taking oral potassium supplements ● Take meds as prescribed to prevent overdosing ● Take supplement with full glass of water ● Do not crush/chew tablets ■ IV piggyback or oral K, never ever IV push ● Hypercalcemia - caused by hyperparathyroidism in about ⅓ of people. Malignancies cause remaining ○ Excess calcium acts like a sedative, leading to reduced excitability of muscles and nerves ○ Neurologic Manifestations - fatigue, lethargy, weakness, and confusion and progress to hallucinations, seizures, and coma ■ Disturbances in cardiac conduction can lead to dysrhythmias, including heart block and v-tachy ○ Nursing Implementation - depends on the degree of hypercalcemia, pt’s condition, and underlying cause ■ Mild - stop any meds related to hypercalcemia, start a diet low in calcium, increase weight-bearing activity, and maintain adequate hydration ● Must drink 3000-4000mL of fluid daily to promote renal excretion of calcium and decrease chance of kidney stones ● Fluids that promote urine acidity (cranberry/prune juice) help to prevent formation of stones ■ Severe - administering saline, a bisphosphonate, and calcitonin ● Hydrate pt with IV isotonic saline to maintain a urine output of 100-150mL/hr ○ Requires careful monitoring - fluid overload can occur if pt has impaired renal function ● Bisphosphonates - most effective agents in tx hypercalcemia ○ Takes 2-4 days for effects - pts receive IM/SC calcitonin for immediate effect ● Calcitonin rapidly increases renal calcium excretion - therapy is only effective for a few days and may cause tachycardia ● Dialysis - for life-threatening situations ● Hypocalcemia - any condition associated with PTH deficiency ○ Pt who receives multiple blood transfusions can become hypocalcemic because the citrate used to anticoagulate blood binds with calcium, decreasing ionized calcium ○ Clinical Manifestations ■ Increased nerve excitability ■ Tetany (sustained muscle contraction) - Chvostek’s sign and Trousseau’s sign ● Chvostek’s sign - contraction of facial muscles in response to a tap over the facial nerve in front of the ear ● Trousseau’s sign - carpal spasms induced by inflating a BP cuff on the arm, when cuff is inflated the carpal spasms occur within 3 minutes if hypocalcemia is present ■ Tetany manifestations - laryngeal stridor, dysphagia, paresthesia, and numbness and tingling around mouth/in the extremities ■ Cardiac effects - decreased cardiac contractility and ECG changes ○ Nursing Implementation ■ Asymptomatic - diet high in calcium-rich foods and calcium and vitamin D supplementation ■ Symptomatic - IV calcium gluconate ■ Measures to promote CO2 retention (breathing into paper bag/sedating pt) can control muscle spasms and other sx of tetany until calcium level is corrected ■ Pts taking loop diuretics may need to change to thiazide diuretics to decrease urinary calcium excretion ■ Closely observe pt who had thyroid/neck surgery ■ Adequately tx pain and anxiety - hyperventilation-induced respiratory alkalosis can precipitate hypocalcemic sx Child with GI Dysfunction Perry pp 1172-1176 ● Nursing should be alert for altered fluid requirements in various conditions ○ Increased Requirements - Fever, vomiting, diarrhea, high-output kidney failure, DI, diabetic ketoacidosis, burns, shock, tachypnea, radiant warmer (preterm infant), phototherapy (infants), postoperative bowel surgery (gastroschisis) ○ Decreased Requirements - heart failure, SIADH, mechanical ventilation, after surgery, oliguric renal failure, increased intracranial pressure ● Dehydration - occurs when the total output of fluid exceeds the total intake, regardless of the underlying cause ○ Can occur from impaired oral intake - it’s often a result of abnormal losses such as vomiting/diarrhea ○ Types Of Dehydration ■ Hypotonic (hyposmotic) Dehydration - occurs in which electrolyte and water deficits are present in approx. balanced proportions ● Primary form of dehydration in children ● Shock is the greatest threat to life, and the child with isotonic dehydration displays sx characteristic of hypovolemic shock ■ Hypotonic (hyperosmotic/hyponatremic) Dehydration - occurs when the electrolyte deficit exceeds the water deficit, leaving serum hypotonic ● Physical signs tend to be more severe with smaller fluid losses than with isotonic/hypertonic dehydration ■ Hypertonic (hyperosmotic/hypernatremic) Dehydration - results from water loss in excess of electrolyte loss and is usually caused by a proportionately larger loss of water/larger intake of electrolytes ● Most dangerous and requires more specific fluid therapy ● May occur in infants with diarrhea who are given fluids by mouth that contain large amounts of solute/in children who receive highprotein (NG) tube feedings that place an excessive solute load on the kidneys ● CNS disturbances (seizures) are more likely to occur ● Cerebral changes are serious and may result in permanent damage ○ Disturbances of consciousness, poor ability to focus attention, lethargy, increased muscle tone with hyperreflexia, and hyperirritability to stimuli (tactile, auditory, bright lights) ○ Clinical Manifestations ■ Detailed hx is first step ■ Parents reports of fluid intake, urine output, diarrhea, and emesis can aid in identification of dehydration ■ Ask parents about tears - a child who is able to produce tears is less likely to have moderate-severe dehydration ■ Weight is the most important determinant of the percent of total body fluid loss in infants and younger children ■ Assess for - changing LOC, altered response to stimuli, decreased skin elasticity and turgor, prolonged cap refill, increased HR, and sunken eyes and fontanels ■ Earliest sign - tachycardia followed by dry skin and mucous membranes, sunken fontanels, signs of circulatory failure (coolness and mottling of extremities), loss of skin elasticity, and prolonged cap filling time ■ When fluid losses exceed the ability of the body to sustain blood volume and BP, circulation is seriously compromised, and the BP falls ■ Shock, a common manifestation of severe depletion of ECF volume, is preceded by tachycardia and signs of poor perfusion and tissue oxygenation (low pulse ox readings) ○ Diagnostic Evaluation ■ In examination of an infant/younger child - most important determinants of extent of dehydration is body weight because this can help to determine percentage of total body fluid lost ■ Urine specific gravity and BUN measurements are unreliable assessments for determining dehydration ■ Serum bicarb level greater than 17 reduces the chances of dehydration whereas bicarb level of less than 13 increases the chance of dehydration requiring IV intervention ○ Therapeutic Management ■ Oral Rehydration Solution - used to tx mild-moderate dehydration ● When child is alert, awake, and not in danger, correction of dehydration may be attempted with oral fluid administration ● Mild cases can be managed at home ● Management consists of replacement of fluid loss over 4-6 hours, replacement of continuing losses, and provision for maintenance fluid requirements ● Enhance flavor of an ORS such as pedialyte by adding unsweetened flavored drink mix, such as kool-aid ● Older children may like a small popsicle orally instead of fluids ● If child is not thirsty and refuses ORS you can administer 2-5mL of ORS by a syringe/small medication cup every 2-3 minutes until child is able to tolerate larger amounts ● If child has emesis, administering small amounts of ORS after 10 mins and administering every 5 minutes may help overcome fluid deficit and emesis often lessons over time ■ Parenteral Fluid Therapy - initiated whenever child is unable to ingest sufficient amounts of fluid and electrolytes ● Pts who require IV fluids are those with severe dehydration, uncontrollable vomiting, inability to drink for any reason, and severe gastric distention ● First priority is restoration of circulation by rapid expansion of ECF volume to treat/prevent shock ● IV fluids begin immediately - typically 0.9% sodium chloride/lactated Ringer’s solution ● Initial Therapy - isotonic electrolyte solution is used at 20mL/kg given as an IV bolus over 5-20 mins and repeated as necessary after assessment of the child’s response to therapy ○ Care Management ■ Ill children have - drawn expressions, dry mucous membranes and lips, and “look sick” ■ One of first behaviors in ill children - loss of appetite ■ Infant’s/child’s activity level is diminished from baseline/usual activities ■ Cry of an ill infant is less vigorous, often whining, and higher pitched than usual ■ Child is irritable, seeks parent’s comfort and attention, and displays purposeless movements and inappropriate responses to people and familiar objects ■ Some cases - child may not protest advances by health care worker and procedures ● These are signs the child truly feels bad and that condition is serious and immediate intervention is necessary ■ As child’s illness and level of dehydration increases in severity, irritability becomes lethargy and even unconsciousness ■ Assess cap refill - less than 2 sec is mild and more than 4 sec is severe dehydration ● Altered in presence of HF ■ Additional signs - mottled extremities, sunken eyes, tachypnea, and changes in sensorium ■ Assess VS every 15-30 mins ● Temp - normal, elevated, or lowered depending on degree of dehydration ● Pulse - tachycardia ● Respirations - hyperpnea ● Blood pressure - hypotension ■ Record fluid I&O’s and body weight freq. ● Use same scale, same clothing, at same time every day ● Accurate I&O’s - oral and parenteral from ○ Urine - freq, color, consistency, and volume (diapers - 1g of wet diaper equals 1mL of urine) ○ Stools - freq, volume, and consistency ○ Vomitus - volume, freq, and type ○ Sweating - only estimated from freq of clothing and linen changes ■ Assess skin - color, temp, turgor, presence/absence of edema, and cap refill ■ Assess mucus membranes - moisture, color, and presence and consistency of secretions ■ Assess body weight - decreased in relation to degree of dehydration ■ Assess fontanel (infants) - sunken, soft, or normal ■ Assess sensory alterations - presence of thirst (only in older child) ● Edema - abnormal accumulation of fluid within interstitial tissue and subsequent tissue ○ Results from anything that alters retention of sodium (renal dz/hormonal influences), affects formation/destruction of plasma proteins (starvation/liver dz), or alters membrane permeability (nephrotic syndrome/trauma) ○ Types of Edema ■ Peripheral - localized/generalized palpable swelling of interstitial space ■ Ascites - accumulation of fluid in abdominal cavity (usually associated with renal/liver abnormalities) ■ Pulmonary - occurs when interstitial volume increases ■ Cerebral - particularly threatening form of edema caused by trauma, infection, or other etiologic factors, including vascular overload/injudicious IV administration of hypotonic solutions ■ Overall fluid gain - especially seen in pts with kidney dz ○ Assessment - manifested by swelling in extremities, face, perineum, and torso ■ Loss of normal skin creases ■ Daily weight ■ Abdominal girth measurement changes ■ Pitting edema ○ Therapeutic Management - primary goal is tx of underlying dz process ■ Essential aspect in management of fluid overload is early recognition Memory joggers for fluid and electrolytes ● Clinical manifestations for heat exhaustion ○ Headache, fatigue, weakness, moist skin/sweating, low BP - orthostatic, increased pulse, anxiety-confusion ○ Body temp below 38.8 or 102*F ○ Management: water and salt replacement, rest ● Clinical manifestations for heat stroke ○ Anxiety - confusion, Skin is hot and dry, impaired sweating, increased pulse & RR, hypotension ○ Na & K+ depletion ○ Body temperature of 105*f or more ○ Can cause cerebral edema (seizures, delirium, coma) ○ Management - cooling, rest, F&E support ● Clinical manifestations of Hyperkalemia ○ Muscle twitches → cramps → paresthesia ○ Irritability and anxiety ○ Low BP ○ EKG changes ○ Dysrhythmias - irregular rhythm ○ Abdominal cramping ○ Diarrhea ● Clinical manifestations of hypokalemia and alkalosis ○ Shallow respirations ○ Irritability ○ Confusion, drowsiness ○ Weakness, fatigue ○ Arrhythmias - irregular rate, tachycardia ○ Lethargy ○ Thready pulse ○ Intestinal motility - nausea, vomiting, ileus ● Fun fact (because we are all having so much fun reading this) ○ Hyperkalemia and acidosis ■ Potassium levels go up in acidosis ● Charting body fluids “COACH” ○ C- color ○ O -Odor ○ A -Amount ○ C -Consistency ○ H -How the patient is tolerating it Mood and Affect Giddens Chapter 33 ● Mood - the way a person feels (depressed because nursing school) ● Affect - the observable response a person has to his or her own feelings. (crying because nursing school) (mode, energy, cognition are the 3 main parts) ○ Euthymia - used to describe normal, healthy fluctuations in mood ○ Mood Spectrum - continuum of all possible moods that any person may experience ○ Mood Spectrum Disorders - disrupt the individual's ability to function normally ■ Individuals with mood spectrum disorders are at increased risk for many problems, such as health status impairment, addiction, and potential for violence ■ Must be dx by physicians/other qualified advanced practitioners trained in making medical/psychiatric diagnoses; that is, the diagnosis of mood spectrum disorders is not within the scope of practice of the generalist nurse ○ Nurses must be able to recognize unstable affective states known as affective instability ■ Signs of affective instability - crying, rage, euphoria, and blunting, indicate the need for further assessment because such individuals may have a mood disorder ○ Functional status - describes the individual's ability to perform ADLs and to realistically solve problems of daily living ■ Used as one indicator to determine the severity of a mood spectrum disorder ● Scope ○ Severe melancholy ○ Mild to moderate melancholy ○ Euthymic - used to describe normal healthy fluctuations in mode ○ Hypomania (mild to moderate mania) ○ Severe mania ● Age-Related Differences - Emotional regulation evolves throughout life and is closely linked with growth and development ○ Infants and Children ■ Mood can only be determined by observation ■ Limited to facial expressions and behavior and is influenced by an increasing awareness of the environment. ■ Infants smile usually at 6 weeks of age, in response to a parent's smile, an infant's expression of emotion is regulated by the amount of physical comfort and by cues from adults ■ Emotional understanding emerges in toddlers as language, cognitive, and social development ■ Emotional regulation is associated with the child's ability to recognize the emotions of others and to mimic the behaviors he or she has observed and experienced ■ Toddlers will attempt to alleviate the distress of another by hugging ○ Adolescents ■ Develop an array of skills to regulate their emotions and are highly aware of social circumstances related to emotional regulation ■ More variability in mood states and affect compared to adults. ■ It is unclear if these differences are due to physiological changes such as hormonal imbalances or differences in emotional reactivity or emotional regulation ○ Older Adults ■ Despite the fact that older adults experience physical and cognitive decline, they often report higher levels of well-being (less negative affect and increased positive affect) and are more responsive to positive emotions compared to younger adult ■ Older adults activate emotional regulation processes to compensate for any negative stimuli they may experience ● Depressive Spectrum ○ Depression is characterized by such overwhelming sadness and despair that you feel drained of energy. Individuals suffering from depression may feel so sad and empty that he or she becomes incapacitated by a loss of the will to live, and suicidal thoughts occur ○ “depression” is commonly misused to describe normal euthymic sadness when there is little or no loss of functional status - must use term carefully ○ The undiagnosed mood state characterized by sadness, despair, and loss of functional status is best referred to as melancholy. ● Mania Spectrum ○ Recognizable by the presence of euphoric or agitated affective states, and they often suffer from degrees of perceptual disturbances as well, such as racing thoughts, grandiose delusions, difficulty concentrating, impulsivity, and lack of insight, they may be reckless and dangerous ○ Nurses are expected to be able to recognize hypomania as an unstable affective state ○ Hypomanic affective states are expansive or agitated and possibly euphoric but to a less severe degree than in mania and with less impairment ○ Perceptual disturbances are much less likely in hypomania, The presence of perceptual disturbances is used to distinguish mania from hypomania ● Consequences ○ Neuroimaging studies of mood spectrum disorders demonstrate reduced blood flow and abnormal phosphorus metabolism in the cerebral cortex and especially the prefrontal cortex ○ Neurotransmitters (dopamine, norepinephrine, and serotonin) are also disturbed in mood spectrum disorders ○ Medical interventions are aimed at restoring neurotransmitter balance ○ Increased potential for suicide ○ Psychosocial variables such as negative life events, personality traits, and individual cognitive styles are associated with mood spectrum disorder ○ Interpersonal relationships limited, productivity limited, high users of medical care ● Risk Factors ○ Lifetime prevalence is 16.2% ○ Age: highest frequency is during the late twenties and early thirties and again during the late sixties ○ Women experience depression two / three times more frequently than men • Individual risk factors ○ Stress, early trauma, neglect, abuse, family history, comorbid medical and psychiatric disorders, personality disorders ○ Substance dependence ● Assessment ○ As nurses we do not diagnose we recognize affective instability as an outward manifestation of a possible mood spectrum disorder ○ Affective instability may be shown as any combination of agitation, sadness, elation, or blunting ○ Blunting is difficult to recognize because it may not be noticeable immediately, blunting is an absence or diminished presence of any affect, and this should be considered a sign of affective instability ○ Speech may be monotone during blunting, and responses may be unusually brief. Blunting must not be overlooked because it may mask dangerously unstable affect ○ History and examination ○ Mental status assessment ○ Assess for functional impairments - unable to solve problems with ADLs ○ Assess for disturbed vegetative functioning - appetite / sleep / energy levels ○ Diagnostic tests ■ No specific diagnostic tests apply and no laboratory tests are used to confirm a diagnosis of a mood disorder ○ Persistent mood disturbance - 2 weeks of melancholic feelings or 4 days of manic behavior - this endorses a nursing assessment of affective instability ● Primary Prevention ○ Not well established - focus on reduction of poverty, racism, violence and stress, early interventions not really prevention ● Secondary Prevention ○ U.S. Preventive Services Task Force (USPSTF) recommends routine screening for mood disorders among adults in primary care settings ○ Screening tools do not diagnose mood spectrum disorder; they measure the severity of symptoms ● Clinical Management ○ Collaborative interventions ■ Motivational interviewing ■ Psychotherapy ● Cognitive therapy attempts to change thoughts ● Behavioral therapy tries to change patterns of behavior that are repeated over time with the same negative results ● Interpersonal therapy focuses on communication patterns and the way the patient relates to others ● Family-focused therapy includes family members in a therapeutic process aimed at problem solving and managing conflict in ways that produce positive outcomes ● Play therapy is an approach for children in which toys and games are used to establish rapport so that the child may better express him or herself. Toys and games may also be used for children who lack the cognitive abilities of expression ■ Pharmacology ● Antidepressants - RX to tx patients with depression ○ SSRIs - first line choice, lower incident of adverse effects ○ NDRIs ○ TCAs ○ SNRIs ○ MOAIs ● Mood stabilizers - are used to tx diagnose of mania and hypomania ○ Lithium- narrow therapeutic range (monitor closely) ○ Antiepileptic ○ Second generation antipsychotic me ■ Brain stimulation therapy - ECT, usually after pt failed to other therapies, ● Induce seizure lasting less than one minute ■ Managing emergent situations (potential for suicide and/or violence) ● Always evaluate for suicidal ideation ■ Case management