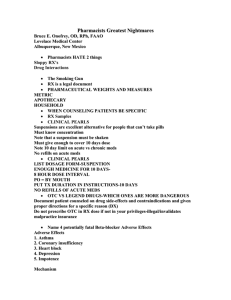
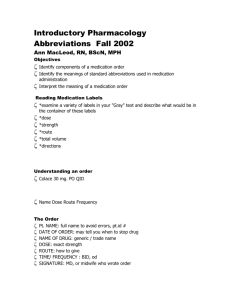
4 Basic Terms: • • • • drug: Pharmacology: Clinical pharmacology: Therapeutics / pharmacotherapeutics =: 3 most important properties of an ideal drug: • effectiveness (most important!) ◦What’s the point if it isn’t effective? No point in using it if not • Safety (second most important) ◦Can’t give a drug that’s harmful, overall the drug needs to provide more benefit than harm to the patient (risk vs. benefit) • selectivity (third most important) ◦No drug effects just one thing, drugs interact with multiple systems. ‣ Ex: Oxycodone is a pain med but it doesn’t JUST effect pain - it slows your respirations, GI motility etc. ◦We want drugs as selective as possible to decrease interactions with other symptoms ‣ Some drugs should be less selective, ex. Epinephrine calms whole body Additional ideal properties: • Reversible action: very easy for oral meds, gets more complicated with IV meds ◦We want to be able to “take it back” ◦If it isn’t reversible we have to provide support to the patient until it wears off • Predictability: we need to know what’s going to happen when you take the drug ◦Based off of when we develop drugs • Easy to administer: patient won’t take it if the med is difficult to take ◦Oral meds are the easiest to take 1x per day ◦Increased dosage and method of dosage increases difficulty of giving the med ‣ Multiple times per day, oral vs. suppository vs. injection • Freedom from drug interactions: we won’t want them to interact with other drugs, food, etc ◦Some drugs interact with each other ◦When drugs do interact but must be taken together, we need to monitor effect on organs, lab values, etc. • Low cost: ideal that we prescribe meds that patients can afford ◦When people are on high cost drugs, they are newly released and give the best benefit • Chemically stable: if the med is on a shelf it doesn’t change in activation or quality ◦Ex: Lasix’s are light sensitive, insulin is heat sensitive • Simple Generic Name: gold standard to know the generic name ◦Sometimes you’ll know the brand name, but generic is usually enough Therapeutic objective of drug therapy • We want to provide maximum benefit with minimum harm! Factors that determine the intensity of drug response: • Prescribed dose • Administered dose ◦Medication errors, patient adherence ‣ If it’s easy to administer, patients are more likely to adhere to the drug regimen ◦Ask questions! ◦Wrong med, wrong route, wrong dose • Concentration at sites of action ◦Pharmacokinetics: what your body does to break down a drug ‣ Absorption: every patient absorbs drugs differently ‣ Distribution: differences in blood pressure changes distribution of medication (low BP = longer time for meds to work) • Poor perfusion will prevent good distribution of medication ‣ Metabolism: liver metabolizes 90% of most drugs, other drugs are metabolized in the GI • When drugs can’t be metabolized, they stay in your body and increase to toxic levels ‣ Excretion: think kidneys and bowels • Kidney failure will prevent drugs to leave the body, can develop toxicity ◦Physiologic variables ◦Pathological variables ◦Genetic variables ◦Pharmacodynamics: what the drug does to your body ‣ Drug-receptor interaction ‣ Patient’s functional state (ability to open meds, cognitive issues) ‣ Placebo effect: devoid of medicinal properties but still provides a therapeutic effect • Things to consider for drug response variation in patients: ◦Genetic factors ◦Medical history ◦Diagnosis ◦Age ◦Sex Evolution of Nursing and Responsibilities Regarding Drugs Ask yourself all 5 of these when giving drugs! ◦Helps to avoid medication error 1. Right Drug 2. Right route: oral vs. IV vs. other routes 3. Right patient: name and DOB, but check the wristband 4. Right dose: dose should match order and check with colleagues for high-risk calculations 5. Right time: meds are timed to accommodate accumulation to prevent toxicity Bonus: right reason! ◦Sometimes the wrong med is ordered for the wrong patient, question reason for medication if it doesn’t seem to fit the patient ◦Doctors will write orders out in a certain way with common abbreviations, always make sure the order is written out • Nurses are very responsible for the drugs given to patients: pay attention! Last line of defense ◦What medications are appropriate for the patient ‣ Advocate for your patients, you know them best ‣ Pay attention to the orders for all drugs to prevent negative interactions ◦What drugs are contraindicated for the patient ◦The probably consequences of the interactions between the drug and the patient Apply Pharmacologic knowledge to 2 areas: 1. Patient Care 2. Patient education: when a patient is educated about their medicine, they are more likely to take the medication. Giving the right education to the patient can prevent medication error, this is dependent on capacity Application of Pharmacology in Patient Care: • collecting patient data ◦Age, sex, genetic factors: influence patient response to drug • Identify high risk patients: ◦Liver and kidney impairments ◦Genetic factors ◦Drug allergies ‣ Follow up with / prophylactic benadryl if the patient MUST have a drug they are allergic to ◦Pregnancy ‣ Can make patients hypertensive, release hormones, develop diabetes ‣ All changes from pregnancy can change patient drug response ‣ Many medicines are toxic to fetuses • Switch to a medicine that is compatible with pregnancy, while keeping in mind risk vs. benefit ◦Older adult vs. pediatric patients ‣ Difference in organ function, metabolism and excretion ‣ Older adults hold onto medications longer in their systems ‣ Pediatric patients have less developed organs • Weight based at this age ◦Tools: patient history, physical exam, lab results ‣ Can effect drugs to give • Does the patient have kidney issues? Is the patient on a PRN asthma med and do they sound wheezy? Are the lab results indicative of need for med or need to hold the med? • Hold the medicine if indicated and let the MD know • IF you notice medicine toxicity: draw a serum drug sample ◦Try to draw from site of action (med dependent) ◦Shows the amount of medication in the body Dosage and Administration • Certain drugs have more than one indication ◦Ex. Tylenol: can help fever AND pain ◦Will need a new order to help BOTH if the order is only for ONE • Dosage may differ depending on the indication for which the drug is being used • Many drugs can be administered by more than one route ◦IV meds are the fastest • Dosage changes when the route changes for most drugs ◦IV abx vs. oral abx dose will be different • Certain IV agents can cause severe local injury if extravasation occurs ◦Vessicans: irritate veins and can cause damage over time ◦Central lines are used for these medications to pump directly into the heart ◦Vein damage can cause loss of limb, pain, irritation • • • • ◦IVs that go past the vein and into subQ tissue can cause infiltration and will change the drug action, absorption will be slower Read the med orders CAREFULLY Verify the patient ID, dose calculation, and reason for medication Read the label carefully Implement any special handling Minimize Adverse Effects: • all drugs have potential to produce undesired effects • Always know the following: ◦The major adverse effects the drug can produce ◦The times when these reactions are likely to occur ◦Early signs that adverse reaction is developing ◦Interventions to minimize discomfort ‣ Patient education! Minimize Adverse Interactions: • take a thorough drug history ◦Medical, family, age, sex, ◦Advise the patient to avoid OTC drugs that can interact with the prescribed medication ‣ Can create issues for the patient ◦Monitor for adverse interactions that are known to occur ◦Be alert for as-yet-unknown interactions Making PRN decisions: • PRN: pro re nata, “as needed” • The RN has discretion regarding how much to give and when to give it ◦PT can also ask for PRN meds ◦Depends on if the order specifies PRN delivery, otherwise ask an MD • Know the reason for the drug’s use • Be able to assess the patients medication needs Managing Toxicity: • early ID makes early intervention possible ◦Notice that toxicity is occurring? Obtain serum drug level, notify MD, withhold med • Know the early signs • Know the procedure for MGMT Application of pharm. in patient education: evaluate the patient’s current knowledge ◦The best way to determine pt knowledge is through demonstration ◦If the patient is educated on their drugs, they are more likely to adhere • drug name and therapeutic category • Dosage size and schedule • Route and technique of administration ◦Very important to know the generic name of their meds • Expected therapeutic response and when it should develop ◦Manage patient expectations ◦Confirm side effects and prepare pt’s for them • Non-drug measures to enhance therapeutic responses • Duration of treatment • Method of drug storage • Symptoms of major adverse reactions and ways to minimize discomfort • Major adverse drug-drug and drug-food interactions • Whole to contact in the event of therapeutic failure, severe adverse reactions, or severe adverse interactions • Promote therapeutic effects: ◦Nature and time course of expected beneficial effects ◦Recognizing treatment failure • Minimizing adverse effects: ◦Insulin overdose ◦Anti-cancer meds and infection (affect white blood cell count) ◦Some side effects are benign but disturbing, especially if they are unknown to the pt Planning: • defining goals ◦Recognize the goal of the prescribed medication • Setting priorities • Identifying specific interventions ◦Drug admin ◦Interventions to enhance therapeutic effects ◦Interventions to minimize adverse effects ◦Patient education Implementation: • drug admin • Patient education • Interventions to enhance therapeutic effects • Interventions to minimize adverse effects Evaluation: • therapeutic response • Patient satisfaction Chapter 3: History of Drugs Drug regulation, development, names, and info • Landmark Drug legislation: ◦Federal Pure Food and Drug Act, 1906 ◦Food, Drug, and Cosmetic Act, 1938 ‣ First act to address drug safety ◦Harris-Kefauver Amendments, 1962 ‣ Thalidomide crisis ‣ Creating regulations of medication in pregnancy ◦Controlled Substances Act, 1970 ‣ Rules for drugs that have the potential for abuse ‣ Increased incarceration ◦Permission for accelerated drug approval, ◦Prescription Drug User Fee Act, 1992 ◦FDA Modernization Act, 1997 ◦Best Pharmaceuticals for Childrens Act, 2002 ◦Pediatric Research Equity Act, 2003 ‣ Helped research drug effects in children and pregnant women ◦FDA amendments act, 2007 ◦Family Smoking Prevention and Tobacco Control Act, 2009 ◦Comprehensive Addiction and Reocvery Act, 2016 ‣ Medical, not criminal New Drug Development: • Randomized controlled trial ◦Use of controls ◦Randomization ◦Blinds ‣ Double blind: neither patient nor provider knows what drug is being given Stages of New Drug Development: • Preclinical testing: only testing on animals, looking at chemical composition • Clinical testing: ◦Phase I: test on healthy human volunteers ◦Phases II and III: patient with the actual illness being treated, apply for and obtain FDA approval ◦Phase IV: out into the world, post-marketing surveillance ‣ Added in to monitor the side effects • Anti-cancer meds can be taken in phase I if the patient is critically ill Limitations of the testing procedures: • limited info about the majority of people: ◦Women ◦Children ◦Diversity • Failure to detect all adverse effects Which name to use: Generic or Trade? • Generic: name that gives information about a drugs classification, “non-proprietary” ◦Little problem: Generic names are more complication than the trade names ◦Big problems: single drug can have multiple brand names, assigned by the US Adopted Names Council, US drugs and drugs outside the US may have different active ingredients ◦Ending to generic drug names indicated drug family • Trade / Brand name: “proprietary” name • Generic vs. Trade ◦The medications are therapeutically equivalent but the outside of the pills are different ◦Absorption varies per brand, sensitivity to capsule / outside of the pill OTC Drugs • Americans spend $20 billion annually on OTC meds • 60% of all doses administered are OTC • 40% of Americans take at least 1 OTC drug every 2 days Most helpful resources for drug info: • clinicians and pharmacists • Poison control center ◦They know what happens when each drug is toxic • Pharmacology textbooks -Be wary of the internet, check your sources-