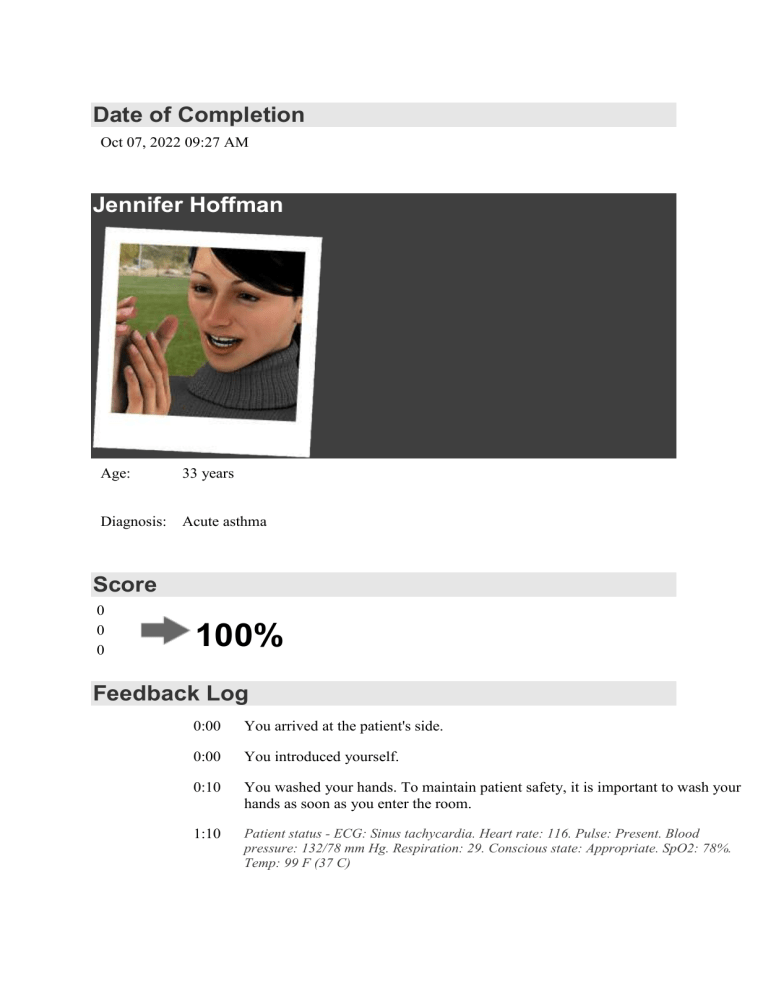
Date of Completion Oct 07, 2022 09:27 AM Jennifer Hoffman Age: 33 years Diagnosis: Acute asthma Score 0 0 0 100% Feedback Log 0:00 You arrived at the patient's side. 0:00 You introduced yourself. 0:10 You washed your hands. To maintain patient safety, it is important to wash your hands as soon as you enter the room. 1:10 Patient status - ECG: Sinus tachycardia. Heart rate: 116. Pulse: Present. Blood pressure: 132/78 mm Hg. Respiration: 29. Conscious state: Appropriate. SpO2: 78%. Temp: 99 F (37 C) 1:24 You identified the patient. To maintain patient safety, it is important that you quickly identify the patient. 1:32 You asked if the patient was allergic to anything. She replied: 'Hay fever' 1:39 You looked for normal breathing. She is breathing at 30 breaths per minute. There is a lot of audible wheezing in the chest. There is increased respiratory effort. 2:10 Patient status - ECG: Sinus tachycardia. Heart rate: 114. Pulse: Present. Blood pressure: 133/78 mm Hg. Respiration: 30. Conscious state: Appropriate. SpO2: 75%. Temp: 99 F (37 C) 2:18 You attached the pulse oximeter. It is a good idea to monitor the saturation and pulse here. This will allow you to reassess the patient continuously. 2:30 You checked the radial pulse. The pulse is strong, 105 per minute and regular. It is correct to assess the patient's vital signs. 2:59 You attached the automatic noninvasive blood pressure (NIBP) measurement cuff. This will allow you to reassess the patient continuously. 3:10 Patient status - ECG: Sinus tachycardia. Heart rate: 113. Pulse: Present. Blood pressure: 129/75 mm Hg. Respiration: 31. Conscious state: Appropriate. SpO2: 73%. Temp: 99 F (37 C) 3:17 You listened to the heart of the patient. There were only normal heart sounds. This is reasonable. 3:43 You listened to the lungs of the patient. There is a lot of audible wheezing in the chest. 3:57 You checked the temperature at the mouth. The temperature was 99 F (37 C). 4:10 Patient status - ECG: Sinus tachycardia. Heart rate: 113. Pulse: Present. Blood pressure: 123/72 mm Hg. Respiration: 31. Conscious state: Appropriate. SpO2: 71%. Temp: 99 F (37 C) 4:16 You examined the patient's skin. There is normal skin turgor. Her skin is blue. 4:23 You placed a nasal oxygen cannula. This was part of your orders. 4:28 You placed an oxygen mask on the patient. This was part of your orders. 4:28 You placed a nasal oxygen cannula. This was part of your orders. 4:33 You placed an oxygen mask on the patient. This was part of your orders. 4:39 You turned the oxygen on. 5:09 You attached a 3-lead ECG. It is correct to attach the monitor to the patient. 5:10 Patient status - ECG: Sinus tachycardia. Heart rate: 113. Pulse: Present. Blood pressure: 126/74 mm Hg. Respiration: 31. Conscious state: Appropriate. SpO2: 75%. Temp: 99 F (37 C) 5:22 You assessed the patient's IV. The site had no redness, swelling, infiltration, bleeding, or drainage. The dressing was dry and intact. This is correct. Assessing any IVs the patient has is always important. 5:45 You placed a 5 mg dose of albuterol in a nebulizer. This is part of the correct treatment of asthma. It is important to use the basic rights of medication administration to ensure proper drug therapy.. 5:55 You placed a 500 mcg dose of ipratropium in a nebulizer. Ipratropium is part of the correct treatment of moderate to severe asthma. 6:00 You flushed the cannula. 6:05 You administered 100 mg of methylprednisolone. You should consider administering this drug slowly. Steroids are part of the correct treatment of severe asthma. 6:10 You flushed the cannula. 6:10 Patient status - ECG: Sinus tachycardia. Heart rate: 118. Pulse: Present. Blood pressure: 132/78 mm Hg. Respiration: 32. Conscious state: Appropriate. SpO2: 80%. Temp: 99 F (37 C) 6:24 You asked the patient if she had any pain. She replied: 'No' 6:46 You provided patient education. This is correct. It is important to use every opportunity to provide patient education. 7:10 Patient status - ECG: Sinus tachycardia. Heart rate: 124. Pulse: Present. Blood pressure: 136/80 mm Hg. Respiration: 32. Conscious state: Appropriate. SpO2: 83%. Temp: 99 F (37 C) 7:23 You laid the patient down. You should probably have left the patient sitting up. 7:24 You sat the patient up. It is correct to do so. 7:42 You looked for normal breathing. She is breathing at 32 breaths per minute. There is a lot of audible wheezing in the chest. There is increased respiratory effort. 8:10 Patient status - ECG: Sinus tachycardia. Heart rate: 128. Pulse: Present. Blood pressure: 137/82 mm Hg. Respiration: 32. Conscious state: Appropriate. SpO2: 86%. Temp: 99 F (37 C) 8:27 You asked the patient how she felt. She replied: 'Not good.' 9:10 Patient status - ECG: Sinus tachycardia. Heart rate: 127. Pulse: Present. Blood pressure: 147/88 mm Hg. Respiration: 28. Conscious state: Appropriate. SpO2: 90%. Temp: 99 F (37 C) 9:28 You measured the blood pressure at 146/86 mm Hg. It is appropriate to monitor the patient by measuring the blood pressure. 9:55 The nebulized ipratropium stopped. 9:57 You phoned the provider in order to discuss the patient. 10:10 Patient status - ECG: Sinus tachycardia. Heart rate: 123. Pulse: Present. Blood pressure: 140/84 mm Hg. Respiration: 25. Conscious state: Appropriate. SpO2: 93%. Temp: 99 F (37 C) 11:10 Patient status - ECG: Sinus tachycardia. Heart rate: 118. Pulse: Present. Blood pressure: 138/82 mm Hg. Respiration: 23. Conscious state: Appropriate. SpO2: 95%. Temp: 99 F (37 C) 11:13 You provided patient education. 11:52 You looked for normal breathing. She is breathing at 22 breaths per minute. There are a few audible wheezes in the chest. The chest is moving normally on both sides. 12:10 Patient status - ECG: Sinus tachycardia. Heart rate: 115. Pulse: Present. Blood pressure: 137/81 mm Hg. Respiration: 22. Conscious state: Appropriate. SpO2: 97%. Temp: 99 F (37 C) 12:11 A patient handoff was performed. Airway and breathing are the most important initial concerns for this patient. An important goal of initial assessment is to recognize the severity of the asthma exacerbation and administer effective treatment. This patient should be placed on a cardiac monitor with automated blood pressure measurement; IV access and continuous pulse oximetry should be established. Humidified oxygen is administered either by non-rebreather mask or by nasal cannula to keep SpO2 above 92%. Commonly used quick-relief medications to treat severe asthma exacerbations include short-acting beta-2-adrenergic agonists, anticholinergics, and corticosteroids. You got 100%