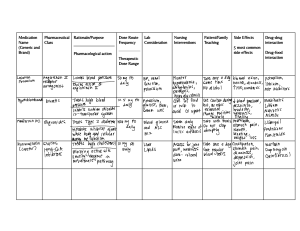
Final exam study guide Prioritization and delegation Nurses continuously set and reset priorities to meet patient needs and maintain safety. Which patients are seen first? Which assessment completed first? Which interventions are provided first? Prioritization principles Systemic before local – “life before limb” Acute before chronic – acuter exacerbation or new injury (mental confusion or chest pain) over long term chronic illness Stable vs. unstable Actual problem before potential problem (e.g., medicating for acuter pain over ambulation for client risk of DVT) Listen carefully to patient, don’t assume (post -op pain could be in another location rather than expected surgical pain) Recognize & respond to trends vs transient findings – recognize gradual deterioration Recognize signs of medical emergencies vs expected patient findings Apply clinical knowledge to procedural standards to determine priority action – recognize timing of administering certain meds (antidiabetic, antibiotics, etc.) is more important than administration of some other meds Priority setting frameworks Maslow’s hierarchy of needs 1. Physiological needs – breathing, food, water, sleep, homeostasis, excretion 2. Safety – security of body, employment, resources, morality, of family, health, property 3. Love & belonging – friendship, family, sexual intimacy 4. Esteem – self-esteem, confidence, achievement, respect of others and by others 5. Self-actualization – morality, creativity, spontaneity, problem solving, lack of prejudice, acceptance of facts ABCs = Airway, Breathing, Circulation, & Disability Airway—establish airway, identify airway concern (obstruction, stridor) Breathing– assess effectiveness of breathing (apnea, depressed RR) Circulation– includes bleeding, hypotension, dysrhythmia, inadequate cardiac output, compartment syndrome, etc. Disability—prevention of disabilities (evolving CVA, etc.) Safety/risk reduction – look for safety risk, compare to other posed risks, give priority response to greatest or most imminent risk Assessment/ data collection – nursing process. Determine if additional info is needed prior to calling provider, etc. Least restrictive/ least invasive – less is more first Acute vs chronic/ Urgent vs non-urgent/ Stable vs unstable Assigning, Delegating, & Supervising Assigning – the process of transferring authority, accountability, & responsibility of patient care to another member of health care team Delegating – the proves of transferring the authority & responsibility to another team member to complete the task, while retaining accountability Supervising – the process of directing, monitoring, & evaluating the performance of task by another member RNLPNsUAP Rights of delegation Right task Right circumstance Right person Right direction Right supervision/evaluation Task that can delegated to LPN Monitor patient findings (as input to the RNs assessment) Reinforce patient teaching from care plan Tracheostomy care Suctioning Monitor nasogastric tube patency Administer enteral feedings Insert foley catheter Medication administration(yes: peripheral IV; no: IVP or chemo) Task that can be delegated to UAP/NA/CNA/TECH Bathing/grooming/dressing Toileting Positioning/ambulating Feeding (without swallow precautions) Specimen collection Intake and output Vital signs (stable pt) RN task Assess Educate Recheck (assessment involved) Admit/Discharge IV Push medication Transfuse blood product Develop care plan/discharge plan Telephone orders Communication Nonverbal: wordless transmission of information Body language Posture, stance, gait Facial expression & eye movement Touch, gestures & symbolic expression Written communication – effective in providing details and legal documentation, lacks the nuances that voice inflection and interactive conversation can provide. The meaning of written communication is often enhanced through discussion. Electronic communication - quickly contribute to a person’s knowledge, providing patients and health care professionals with vital information. patients and nurses must take time to validate and verify shared information because misunderstandings can occur if feedback is inadequate. Special care must be taken to maintain confidentiality while communicating electronically. Types of communication Intrapersonal - focuses on personal needs and can influence a person’s well-being. Positive self-talk Negative self-talk Meditation Prayer Interpersonal – formal or informal and conversational, and it may or may not have a stated goal or purpose. In the context of an interview, it may vary from the strictly formal to very casual. Interprofessional communication Ethical implications Therapeutic communication -primary focus: the patient. Nurses engaged in therapeutic conversations set their own opinions and judgments aside to listen more fully to their patients. Encourage the listener to sit facing the patient Remind nurse to maintain open stance or posture while listening Suggest listener lean towards speaker Refers to maintain eye contact without staring relax Non-therapeutic communication - can be hurtful and potentially damaging to interaction. Changing the subject or sharing personal opinions limit conversation between the nurse and the patient and discourages open conversation on sensitive topics. Communication process – respect, assertiveness, collab, delegation, advocacy o establish heling relationship – trust, empathy, est. boundaries, respect cultural influences, dev comprehensive plan of care factors that affect communication impaired verbal communication – (verbal, nonverbal, intrapersonal, interpersonal) o culture – language barrier, appearance, personal space o language o interpreter o disease process o comprehension communication tools SBAR – situation, background, assessment, recommendations Confidentiality & privacy – all pt info must be kept confidential + private; info only released E pt informed consent o HIPPA Standardized national language o NANDA Medication administration Medication administration o Pharmacological concepts − Drug names Chemical name – exact desc. of the drug is chem composition + molecular structure Generic (nonproprietary) name assigned by OSAN council when manf. is ready to market the drug Official name – generic name listed in USP +NF Brand/trade/proprietary name – what the drug is sold as in stores Mechanisms of drug action o Absorption – movement of drug from administration site to the bloodstream; passage of med molecules o Distribution – transportation of a drug in bodily fluids (i.e., bloodstream) to various tissues & organs through the body − Within the body to tissues, organs, & specific sites of action o Metabolism – AKA. Biotransformation – chemical inactivation of a drug through its conversion into a more water-soluble compound or into metabolites that can be excreted − Under influence of enzyme that detoxes, breaks down & removes active chemical o Excretion – removal of drug molecules from their sites of action & eliminated from the body − Via kidney, liver, bowel, lungs, exocrine glands Factors affecting drug action − Absorption: route, ability to dissolve, blood flow, body surface area, lipid solubility − Distribution: physical & chemical properties of med, circulation, membrane permeability, protein-binding − Metabolism: active chemical; occurs in liver, kidneys, blood, intestines, & lungs − Excretion: chemical makeup decides method of exit; delayed excretion by inactivity, poor diet, + peristalsis Drug excretion: kidneys, liver, GI tract, lung, exocrine glands classification systems for drugs: usage, body system, chem/pharm class adverse effects of drugs o allergy – damaging immune response by the body to a substance to which it has become hypersensitive − clinical manifestations: urticaria (hives), pruritis (itching), edema of soft tissue & mucosa, rhinitis (inflammation of nasal mucosa), nausea, vomiting − make sure you verify with the patient if they have any allergies to food, latex, or medications – if yes, ask what happened & notify doc; some patients may not know what a drug allergy is or if they have one − anaphylaxis: sudden constriction of bronchioles, edema of the larynx & pharynx, severe shortness of breath, wheezing, & severe hypotension; unpredictable response to med discontinue medication, get order/administer epinephrine, IV fluids, steroids, & an antihistamine patients with severe allergic reactions (like anaphylaxis) should wear a medic alert bracelet/necklace & carry epinephrine for emergency situation o drug tolerance – decreased response to repeated doses of medication & requires increased doses of med to reach the desired effect o toxic effect – accumulation of med within the bloodstream i.e., resp distress from excessive morphine; hypoglycemia from too much insulin o idiosyncratic effect – an unexpected, abnormal, or peculiar response to a medication − extreme sensitivity to a medication, lack of response, or a paradoxical (opposite of expected) responses o interactions − antagonistic: happens when one drug interferes with the actions of another & decreases the resultant drug effect antagonist blocks response: agonist produces response − synergistic: addictive effect effect of both drugs together is greater than the individual effects of the single med − drug incompatibilities: occur when multiple drugs are mixed, causing a chemical deterioration of one or both drugs o teratogenic – drugs known to cause developmental defects in a fetus (i.e., alcohol, Dilantin) pharmacology/analgesics o pharmacology: study of drug effects; enter body, absorbed, realistic, physiological function, metabolized, exit o pharmacokinetics: what happens to the drug in the body; absorption, distribution, metabolized, & excretion of drug; time until onset & peak o pharmacodynamics: how the drug effects the body how meds achieve their effects at various sites − opioid analgesic – provides moderate to severe pain relief − non-opioid analgesic – provides mild t moderate pain relief − non-steroidal anti-inflammatory drugs (NSAIDs) – control mild to moderate pain, fever, & various inflammatory conditions − herbal supplements – generally not regulated by the FDA & can have serious reactions when mixed with drugs principle of safe medication administration o 3 checks 1. Before you pour – check the med against the MAR; make sure name, route, dose, & time match the MAR entry 2. After you pour – before returning the container or discarding anything; verify the label against MAR 3. At the bedside – check the medication label 6 rights of medication administration – patient, drug, dose, route, time, documentation Dosage calculation – formula method most commonly used 𝑑𝑜𝑠𝑒 𝑑𝑒𝑠𝑖𝑟𝑒𝑑 (𝐷) 𝑥 𝑞𝑢𝑎𝑛𝑡𝑖𝑡𝑦 𝑜𝑛 ℎ𝑎𝑛𝑑 (𝑄) = 𝑑𝑒𝑠𝑖𝑟𝑒𝑑 𝑞𝑢𝑎𝑛𝑡𝑖𝑡𝑦 𝑑𝑜𝑠𝑒 𝑜𝑛 ℎ𝑎𝑛𝑑 (𝐻) Sites for administering medication o Oral – tablets, capsules, liquid, buccal, sublingual, enteral − Have A LOT of special considerations – i.e., how does the patient take their meds? Oral: prep by picking desired liquid/food for admin (water, juice, pudding, etc), disposable med cup, pill splitter//crusher, straw if allows/wanted, clean gloves; may also need stethoscope id giving cardiac med Buccal: rapidly absorbed in mucous membranes between gum & cheek in mouth Sublingual: rapidly absorbed in mucous membranes under the tongue Enteral: nasogastric (NG tube) & gastrotomy meds – for those that cant swallow or have feeding tubes NG tube bypasses throat in case of dysphagia when GI is intact or to attach wall suction in case of bowel surgery or obstruction (OBX) Give liquid eds, crushed meds flush before & after, elevate HOB, disconnect from suction for 30 min o Topical – applied directly to body surface/cavity; lotions/creams/ointments, transdermal patches, eye & ear, nasal, vaginal, rectal − Always wear gloves when giving/changing topical medications o Inhalation – respiratory (nebulizers – atomizers, aerosols, MDIs), dry powder inhaler − Nebulization: production of a fine spray, fig, powder, or mist from a liquid drug, inhales med mixture by breathing deeply through mouthpiece attached to neb; airways & alveoli are increasingly vascularized & absorb inhaled meds quickly − Atomizers disperse med as large droplets; aerosol suspends droplets of med in a gas; MDIs delivered measured dose of nebulized drug − Dry powder inhalers activated by a pump rather than by inhalation, no spacer needed o Parenteral – injected/infused into body tissues or into blood stream; ID, IM, IV, SQ − Intradermal (ID): given into the dermis (middle layer of skin); commonly used for allergy or TB testing * 15 needle length: 3/8 needle gauge: 28g, 27g, 26g max vol: 0.1mL * sites: above boob, upper back, lower forearm Subcutaneous (subcut): given into subcut tissue (layer of fat below dermis & above muscle o Slower absorption than IM because subcut tissue doesn’t have a rich blood supply o Arms &ABD fastest absorption; high & upper buttocks slowest absorption; most evenly absorbed by ABD – don’t aspirate for blood return * 45 or 90 needle length: 5/16, ½, 5/8 max vol: insulin: 1.0mL 28-31g, other SQ: 1.0mL 25-27g Intramuscular (IM): given into muscle o better than subcut because muscles can also handle more fluid o vastus lateralus preferred for infants o z track method recommended for IM injections because it's less painful & helps prevent irritation of subcutaneous tissue o deltoid, ventrogluteal, vastus lateralis sites o meds are absorbed rapidly where blood flow to the tissue is greater * 90 needle length: 1, 1½, 2 needle gauge: 23g, 22g, 21g max vol: deltoid: 1mL, other: 3mL Intravenous (IV): meds given via catheter or cannula into a vein; begins to act immediately (so you stop it if an adverse reaction) * needle length: 1 needle gauge: 19g, 18g Hypertension 1.) Discuss the risk factors, causes, and signs/ symptoms for hypertension. Risk Factors Family history, obesity, smoking/ drinking, stress, chronic kidney disease, too much salt, and certain medications and vitamins signs/ symptoms - hypertension damages vital organs - Ex: Coronary artery disease, left ventricular hypertrophy, heart failure, peripheral vascular disease, renal failure , and retinal damage. - (Other symptoms of hypertension) headache, fatigue, vision problems, chest pain, difficulty breathing, pounding in chest, neck or ears, blood in urine, and irregular heartbeat 2.) Explain the classification & stages of hypertension. Hypertension- is the persistent elevation at systolic/ diastolic blood pressure based on constant heart readings Hypertension Crisis- can be very severe, abrupt, and elevated blood pressure results - often occurs in patients who have hypertension and are not compliant with medications or are under medicated - the brain can swell, heart failure, sweat, etc. - Treatment : hospitalization, IV meds, cardiac monitor, and monitor renal function Medication classification Ace Inhibitors –“prils” drugs Generic name Common brand names Benazepril Lotensin Captopril Capoten Enalapril Vasotec Lisinopril Prinivel, Zestril o Action: Angiotensin is a chemical that causes the arteries to become narrow, especially in the kidneys but also throughout the body. ACE stands for Angiotensin-converting enzyme. ACE inhibitors help the body produce less angiotensin, which helps the blood vessels relax and open up, which, in turn, lowers blood pressure. o Indication: for mild to severe hypertension o SE: headache and skin rash, “ACE cough” – dry, hacking cough due to build up, Firstdose can cause syncope, severe hypotension and fainting within 1-4 hours after the initial dose or after a significant increase in dose o Nurse measures: monitor hourly, Instruct the client to lie down for 3-4 hours after the first dose, Give 1 hour before meals, Instruct the client to avoid substances– coffee, tea, cola, OTC, cold meds Calcium channel blockers Generic name Common brand names Amlodipine besylate Norvasc Diltiazem hydrochloride Cardizem Nifedipine Procardia Verapamil hydrochloride Calan o Action: prevents calcium from entering the smooth muscle cells of the heart and arteries. decreasing the calcium, the hearts' contraction is not as forceful. Calcium channel blockers relax and open up narrowed blood vessels, reduce heart rate and lower blood pressure. o SE: peripheral edema of legs and ankles; flushed skin, headache, dizziness, nausea, constipation, fatigue, weakness, impotence; Serious side effects- MI, hepatotoxicity, heart failure, confusion, o AE: flushing, headache, dizziness, weakness, bradycardia, orthostatic hypotension, sexual dysfunction o Nurse measures: before meals, “dangle” for a few minutes before ambulating and to change positions slowly, Avoid caffeine, Avoid grapefruit when taking nifedipine (Procardia) and Amlodipine (Norvasc) Beta blockers –“olol” drugs Generic name Common brand names Atenolol Tenormin Metoprolol Lopressor, Toprol Nadolol Corgard Propranolol Inderal Timolol Blocadren o Action: This results in slower heart rate, reduced contractility of the heart muscle, and vasodilation of the arterioles, with reduction of PVR and BP o SE: : Bradycardia, fatigue, difficult physical exertion, insomnia, impotence, confusion. Result is decreased cardiac output. Serious side effect- MI with abrupt withdrawal o Nurse measures: avoid substances that interfere with the BB’s such as caffeinecontaining beverages and OTC cold remedies, sudden cessation of BB’s because this can cause rebound hypertension Alpha adrenergic antagonists (blockers) Generic name Common brand names Doxazosin mesylate Cardura Prazosin Minipress o Action: relax muscle tone of the vascular walls, helping small blood vessels remain open. This improves blood flow and lowers blood pressure. o AE: first-dose syncope, orthostatic hypotension, reflex tachycardia & increased workload of the heart (may cause myocardial ischemia or infarction) o Nurse measures: monitor for orthostatic hypertension, weight gain w/ edema, tachycardia. Instruct clients to change positions slowly Alpha adrenergic agonists Generic name Common brand names Methyldopa Clonidine Aldomet Catapres o Action: reduce blood pressure by decreasing the activity of the sympathetic (adrenalineproducing) portion of the involuntary nervous system. Methyldopa is considered a first line antihypertensive during pregnancy because adverse effects are infrequent for the pregnant woman or the developing fetus. This results in a decrease in peripheral vascular resistance to lower BP. o AE: dry mouth, sedation, erectile dysfunction, sleep disturbances, nightmares o Nurse measures: avoid hot baths and showers because this worsens hypotension, Avoid excessive use of caffeinated beverages, Take the medication at bedtime to avoid daytime sleepiness, Suggest chewing gum or hard candies to relieve mouth dryness Angiotensin II receptor blockers (ARBs) –“sartan” drugs Generic name Common brand names Losartan potassium Cozaar Valsartan Diovan o Action: This means blood vessels stay open and blood pressure is reduced, lowering peripheral resistance and blood volume. o SE: Headache, skin rash, diarrhea, orthostatic hypotension, Good alternative for those with “Ace” cough, Not as effective in African Americans unless taken with another drug, Avoid foods high in potassium Diuretics Generic name: Thiazide diuretics Common brand names Hydrochlorothiazide Hydro-diuril, HCTZ Metolazone Zaroxolyn Usually, drug of choice for pt w/ uncomplicated hypertension o Action: : act on the renal tubules to inhibit reabsorption of sodium chloride, which increases potassium loss; water follows sodium- so sodium is not absorbed and blood volume is decreased o AE: dehydration, electrolyte imbalance, orthostatic hypotension, digoxin toxicity, erectile dysfunction, atigue, hypokalemia, affect glucose control Generic name: Potassium-sparing diuretics Common brand names Spironolactone Aldactone Triamterene Dyrenium o Action: act on distal tubules of kidneys to inhibit reabsorption of sodium reducing excretion of potassium o AE: hyperkalemia, hypotension Generic name: Loop diuretic Common brand names Furosemide Lasix Bumetanide Bumex o Action: inhibit sodium chloride reabsorption in the ascending loop of Henle, thereby increasing the excretion of sodium and potassium. Bumex has a much stronger action than Lasix, but is shorter acting o AE: electrolyte imbalance, orthostatic hypotension, ototoxicity (usually reversible), dehydration Nurse measures Diuretics reduce blood volume, Increase urine output-diuresis Long-term use results in vasodilation, which decreases B/P Monitor electrolytes, especially potassium Monitor for S/S of dehydration (thirst, weakness, muscle cramping, hypotension & tachycardia) Monitor I&O and weight Instruct the client to change positions slowly to avoid dizziness and falls Instruct the client to take the last dose in the afternoon to avoid nocturia People with diabetes may find that diuretic drugs increase their blood sugar level. A change in medication, diet, insulin or oral anti-diabetic dosage corrects this in most cases