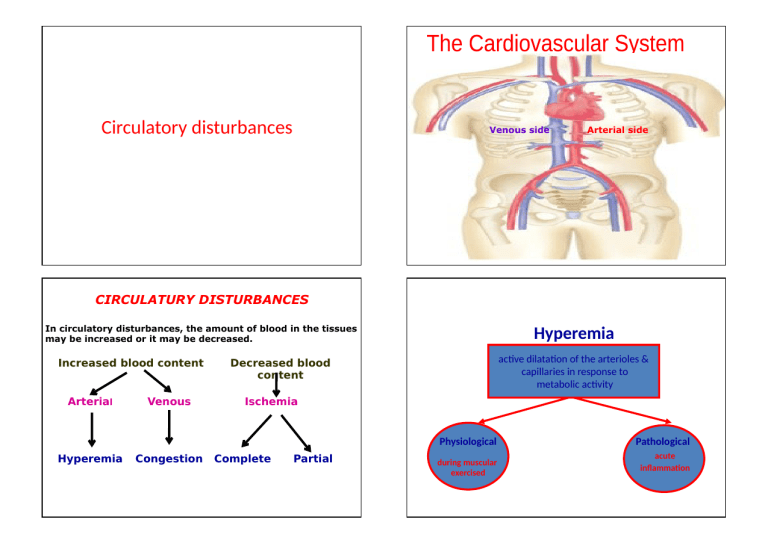
Circulatory disturbances Venous side Arterial side CIRCULATURY DISTURBANCES In circulatory disturbances, the amount of blood in the tissues may be increased or it may be decreased. Increased blood content Arterial Venous Hyperemia ac1ve dilata1on of the arterioles & capillaries in response to metabolic ac1vity Decreased blood content Ischemia Physiological Hyperemia Congestion Complete Partial during muscular exercised Pathological acute in6amma7on Conges7on Physiological hyperemia • Because the increased oxygen consump1on of during muscle contrac1on s1mulates the produc1on of vasoac1ve substances that dilate the vessels in the skeletal muscle. Other examples include the increase in gastrointes1nal blood >ow during diges1on of food Passive dilata1on of the veins & capillaries in response to obstruc1on of the venous ouAlow General acute local Chronic acute Chronic Ischemia Generalized conges7on: Acute as acute heart failure Chronic ( gradual) e.g. chronic RT sided HF. Localized conges7on: Acute: Sudden complete venous obstruc7on due to thrombosis Chronic: Gradual incomplete venous obstruc7on e.g. venous compression It is decrease of blood supply to an organ due to occlusion of its arteries: These occlusion may be: Partial : usually gradual Complete : usually sudden Causes of Ischemia Generalized ischaemia : Due to low cardiac output Localized ischaemia : Due to arterial or venous obstruction Venous obstruction --- cong. & oedema --increase in the tissue pressure ------- arterial obstruction ------ ischemia INFARCTION Is an area of coagulative necrosis (liquefactive in the brain) due to sudden occlusion of either arterial or venous supply (ischemia) 1-Sudden Ischemia (Acute ischemia): Sudden complete arterial occlusion by: Thrombosis or embolism Surgical ligature of the artery EFFECTS: sudden occlusion----- infarc1on (coagula1ve necrosis) and gangrene 2-Gradual Ischemia (Chronic ischemia) Gradual incomplete occlusion: • Atherosclerosis • Pressure on the artery EFFECTS: Cellular degenera1on, atrophy, degenera1on and replacement Jbrosis TYPES OF INFARCTION RED INFARCTION: (Hemorrhagic) Its occur in soM and vascular organs as lung, liver and intes1ne, early – red due to hemorrhage and late – pale in color PALE INFARCTION: Are more common and occur in Jrm and less vascular organs as kidney, heart and spleen Bed Sores: It is ischemic necrosis with subsequent sloughing of skin as a result of pressure of prolonged recumbency It is of special clinical importance. It is the name given to ulcers occurring over bony prominence (sacrum) as a complica7on of prolonged recumbency specially in old or debilitated pa7ents. - Prolonged pressure over bony prominence interferes with the circula7on of the 7ssues necrosis of 7ssues sloughing and ulcera7on secondary bacterial infec7on with putrefac7on. Veins are the commonest site of thrombus formation due to : 1. 2. 3. 4. 5. Thin wall : easily comprisable Superficial :easily traumatized Inactive :lack of muscular pumping action Low blood pressure Slower blood flow Thrombosis Thrombosis It is formation of a solid mass from the constituent of the circulating blood within the cardiovascular system. Site : Veins Arteries Capillaries Heart 3 factors that predispose to thrombosis (Virchow’s Triad) Stasis Injury to the vessel wall Hypercoagulability Pathogenesis of thrombosis Stasis of blood: (slow blood >ow) as • In case of local venous conges7on • Heart failure • Prolonged recumbency. Injury of blood vessels: as in case of • Repeated venous injec7on • In6amma7on of vessels wall • Atherosclerosis. factor VIII Platelets adherent to the injured endothelium Endothelial cells produced von willebrand (factor VIII) which act as a bridge between platelet surface receptor & collagen Hypercoagulability of blood: as in cases of • Decrease plasma of blood……dehydra7on • Increase blood cells…………polycythemia and leukemia Types( classiJca1on ) of thrombi Fate of the Thrombus According to Extent of thrombus •Mural •Occlusive •Propagated Present of organisms •Sep7c •Asep7c Thromboplas7n liberate from damaged 7ssue& platelet Convert Ubrinogen into Ubrin which deposit on pale thrombus Color & cons7tuent •Red •Pale •Mixed 1-Septic thrombus----- fragmented by the proteolytic enzymes into septic emboli causes pyaemic abscesses 2-Aseptic thrombus If mass is small it dissolves by fibrinolysis If mass is large it undergoes: If mass is large it undergoes: Organization(fibrosis): the thrombus is invaded by capillaries and fibroblast --- change to fibrous mass– lead to permanent vascular occlusion Organization and Canalization; some time capillaries dilated and allow Passage of blood through the thrombus; Incorporation : the fibrosed thrombus shrinks from the vascular wall leaving a space which gets lined by endothelium Dystrophic calcification----- phlebolith (stone in blood vessels) Detachment--- aseptic emboli--- infarctions Propagating thrombus--- due to spread of venous thrombosis Main differences between Clot & Thrombosis Clot Thrombosis Vital or not ,during live or after death Vital process (occurring only during life ) In vivo or vitro Only in vivo (inside blood vessels) Fibrin is the main lement Platelet are essential Blood is stagnant Blood is in motion Not adherent to vessel wall Adherent to vessel wall Wet & elastic Dry & friable



