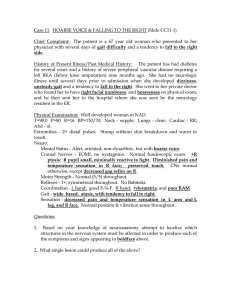
Health Assessment Lecture Neurologic Assessment Cervical Nerve Region Head and neck Diaphram (or diaphragm?) Arms and hands Thoracic Nerve Region Chest muscles Breathing Abdominal muscles Lumbar Nerve Region Legs and feet Sacral Nerve Region Bowel and bladder control Sexual functions Perception and Coordination Assessment Things to consider: The client’s chief complaints The client’s physical condition (LOC, ability to ambulate) The client’s willingness to cooperate What to Assess? Mental status including LOC Cranial nerves Reflexes Motor functions Sensory functions Equipments Sugar, salt, lemon juice, quinine flavours Percussion hammer Tongue depressors Cotton balls Optional: test tubes of hot and cold water Pins or needle for tactile discrimination Mental status Reveals the client’s general cerebral function (language, memory, concentration, or thought process) o Intellectual (cognitive) o Emotional (affective) 1. Language If the client displays difficulty speaking: Point to common objects, and ask the client to name them Ask the client to read some words and to match the printed and written words with pictures Ask the client to respond to simple verbal and written commands Aphasia Any defects in or loss of the power to express oneself by speech, writing, or signs, or to comprehend spoken or written language due to disease or injury of the cerebral cortex 1. Sensory or Receptive Aphasia The loss of the ability to comprehend written or spoken words o Auditory/Accoustic – lost the ability to understand the symbolic content associated with sounds o Visual – lost the ability to understand printed or written figures 2. Motor or Expressive Aphasia Involves loss of the power to express oneself by writing, making signs, or speaking Inability to combine speech sounds into words 2. Orientation Ability to recognize other persons, awareness of when and where they presently are (time and place), and who they, themselves are Reminder o The client is awake, alert, and oriented o This refers to the accurate awareness of persons, time and place Determine the client’s orientation to person, time, and place by tactful questioning Ask: o Place of residency o Time of day o Date o Day of the week o Duration of illness o Names of family members o Others Be sure you know the correct answers 3. Memory Assess the client’s recall of information A. Immediate recall If client can only remember information presented seconds previously B. Recent memory If client can only remember events or information from earlier in the day or examination C. Long term memory Knowledge recalled from months or years ago 4. Attention span and Calculation The client’s ability to focus on a mental task that is expected to be able to be performed by persons of normal intelligence Level of Consciousness (LOC) I – Alert Oriented 3x, follows simple command and responds completely and appropriately to stimuli The patient does not require stimulation II – Lethargic (sleepy, drowsy, obtunded, somnolent) Requires stimulation but when awakened, remained oriented 3x Awakened when called loudly then immediately fell asleep May drift off to sleep during examination III – Stuporous Requires more stimulation, but when awakened the patient is disoriented to time, person, and place Example: person under the influence of drugs and alcohol IV – Semi-comatose May respond to painful stimuli but not to verbal command With reflexes present V – Deep coma Clinical state of unconsciousness in which the patient is unaware of self or environment May or may not respond to noxious or painful stimuli Areflexic: no gag reflex when suctioned With brain injury May assyme decorticate or decerebrate posturing Glasgow Coma Scale Developed to predict recovery from a head injury Used also to assess the Level of Consciousness (LOC) A. Eye response B. Motor response C. Verbal response CN CN 1 Nerve Olfactory Maximum points/score: 15 Lowest possible score: 3 State of coma: 7 and below CN II Optic Faculty measured 1. Eye opening Response: Spontaneous = score: 4 To verbal command = score: 3 To pain = score: 2 No response = score: 1 2. Motor response Response: To verbal command. Score: 6 To localized pain. Score: 5 Flexes and withdraws. Score: 4 Decorticate. Score: 3 Decerebrate. Score: 2 No response. Score: 1 3. Verbal Response Response: Oriented, converses. Score: 5 Disoriented, converses. Score: 4 Uses inappropriate words. Score: 3 Makes incomprehensible sounds. Score: 2 No response. Score: 1 Example: 1. Eye opening: client reacts to pain = score: 2 Motor response: no response = score 1 Verbal response: uses inappropriate words = score: 3 Total score: 6 Cranial nerves Function Type Smell Sensory sight Sensory Test Ask the patient to identify smell Assess vision in OU (Snellen’s Chart) Abnormal Findings of CN I Inability to smell (neurogenic anosmia) or identify the correct scent may indicate olfactory tract lesion or tumor lesion of the frontal lobe Loss of smell may also be congenital or due to other causes such as nasal or sinus problems It may also be caused by injury of nerve tissue at the top of the nose or the higher smell pathways in the brain due to viral upper respiratory infection Smoking and use of cocaine may also impair one’s sense of smell Abnormal Findings of CN II Abnormal findings include difficulty reading Snellen Chart, missing letters, and squinting Client reads print by holding closer than 14 inches or holds print farther away as in presbyopia, which occurs with aging CN CN III CN IV CN V CN VI Nerve Function Oculomotor Eye movements Trochlear Superior oblique Trigeminal Mastication and facial sensation, corneal reflex Abducens Facial movements, expression, tear and saliva secretion Type Motor Test Check pupil constriction; eye movement Motor Assess patient ability to look downward and inward Both M: assess the patient to clench jaw S: facial response to touch Motor Assess lateral deviation of the eye Abnormal Findings of CN III, IV, V, VI Ptosis (drooping of the eyelids) is seen with weak eye muscles such as in myasthenia gravis Inability to feel and correctly identify facial stimuli occurs with lesions of the trigeminal nerve or lesions in the spinothalamic tract or posterior columns CN CN VII Nerve Facial Function Type Posterior Both external ear, taste (Ant 2/3) muscles of facial expressions Test M: Assess patient’s ability to smile, elevates eyebrows S: check taste on anterior 2/3 of the tongue (sugar and salt) Abnormal Findings of CN VII Inability to close eyes, wrinkle forehead, or raise forehead along with paralysis of the lower part of the face on the affected side is seen with Bell’s palsy (a peripheral injury to cranial nerve VII (facial) Paralysis of the lower part of the face on the opposite side affected may be seen with a central lesion that affects the upper motor neurons, such as from stroke Reflexes Are assessed using a percussion hammer Described on a scale of 0-4 Grade 0 1+ 2+ 3+ 4+ Abnormal Findings of CN IX, X Soft palpate does not rise with bilateral lesions of cranial nerve X (vagus). Unilateral rising of the soft palate and deviation of the uvula to the normal side are seen with a unilateral lesion of the cranial nerve X (vagus) Dysphagia or hoarseness may indicate a lesion of cranial nerve IX (glossopharyngeal) or X (vagus) or other neurologic disorder Abnormal Findings of CN XI Asymmetric muscle contraction or drooping of the shoulder may be seen with paralysis or muscle weakness due to neck injury Abnormal Findings of CN XII Atrophy of the tongue may be seen with peripheral nerve disease Deviation of the affected side is seen with a unilateral lesion Deep tendon reflexes Interpretations None Hypoactive Normal Mild hyperactive with clonus (uncontrollable jerks of the muscle) Hyperactive with clonus Babinski response Stroke the lateral aspect of the sole of each foot using a blunt object Note movements of toes o Normal – withdrawal o Abnormal – extension of big toe with fanning of other toe Biceps reflex Test the spinal cord level C5-C6 Triceps reflex Test the spinal cord C7-C8 Brachioradialis reflex Test the spinal cord C5-C6 Patellar reflex Test the spinal cord level L2-L4 (continuation ata ito? sa page 3, upper left corner) Achilles reflex Test the spinal cord level S1-S2 D. Reflex An automatic response of the body to a stimulus Not voluntary learned or conscious Plantar reflex (Babinski) Normal: (-) Babinski: all five toes bend down Deep tendon reflex It is activated when a tendon is stimulated (tapped) and its associated muscle contracts As persons ages, reflex response may become less intense E. Motor Function Evaluates proprioception and cerebellar function Abnormal response to touch Anesthesia Loss of sensation Structures involved: Proprioceptors – are sensory nerve terminals, occurring chiefly in the muscles, tendons, joints, and the internal ears, that give information about movements and the position of the body Posterior columns of the spinal cord Cerebellum Vestibular apparatus in the labyrinth of the inner ear Hyperesthesia More than normal sensation F. Sensory Function Includes: Touch Pain Temperature Position Tactile discrimination Types of Tactile Discrimination 1. One and Two Point Discrimination The ability to sense whether one or two areas of the skin are being stimulated by pressure Check for the sense of touch, presence of pain, and temperature Face Arms Legs Hands Feet If with numbness, peculiar sensation, paralysis Check sensation more carefully over flexor and extensor surfaces of the limb, examining about every 2cm (1inch) Hypoesthesia Less than normal sensation Paresthesia Abnormal sensation such as burning, pain, or an electric shock 2. Stereognosis The act of recognizing objects by touching and manipulating them Graphestesia Ability to recognize writing on the skin purely by the sensation of touch Sensory exam: Vibration (huy gagi, hindi ko na alam saang part ito, sorry T^T) Extinction Phenomenon Normal findings Both points of stimulus are felt Deviation from normal Failure to perceive touch on one side of the body when two symmetric areas of the body are focused simultenously (common to clients with lesions of the sensory cortex) Commented [T1]: Ito rin, nakakalito na yung Page 57 onwards ng PDF file ni maam T^T Motor function Gross motor and balance test 1. Walking Gait Normal findings Has upright posture and steady Gait with opposing arm swing; walks unaided, maintains balance Deviation from normal Has poor posture and unsteady; irregular staggering gait with wide stance, bends legs only from hips Has rigid or no arm movements Walking Abnormalities Waddling Gait A distinctive duck-like walk that may appear in childhood or later in life Propulsive Gait A stooped, rigid posture, with the head and neck bent forward Scissors Gait Legs flexed slightly at the hips and knees, giving the appearance of crouching, with the knees and thighs hitting or crossing in a scissors-like movement Spastic Gait A stiff, foot-dragging walk caused by one-sided, long term, muscle contraction Steppage Gait Foot drop where the foot hangs with the toes pointing down, causing the toes to scrape the ground while walking Neurodegenerative illnesses Skeletal abnormalities and disease Toxic reactions Romberg Test Normal findings Negative romber: may sway slightly but is able to maintain an upright posture and foot stance Deviation from normal Positive Romberg: cannot maintain foot stance; moves feet apart to maintain stance Ataxia – lack of coordination of the voluntary muscles Cebellar ataxia – cannot maintain balance whether eyes are shut or open Standing on One Foot with Eyes Closed Normal findings Maintain stance for at least 5 seconds Deviation from normal Cannot maintain stance for 5 seconds Heel-Toe Walking Normal findings Maintains heel-toe walking along a straight line Deviation from normal Assumes a wider foot gait to stay upright Toe or Heel Walking Normal findings Able to walk several steps on toes or heels Deviation from normal Cannot maintain balance on toes or heels Fine Motor Test for the Upper Extremities Abnormal Gait may be caused by: Central Nervous System disorders of the brain tha cause muscular problems resulting in gain disturbance Spinal cord abnormalities Degenerative muscle diseases A. Finger-to-Nose Test Normal findings Repeatedly and rhythmically touches the nose Deviation from Normal Misses the nose or gives slow response B. Alternating Supination and Pronation of Hands and Knees Normal findings Can alternately supinate and pronate hands at rapid pace Deviation from normal Performs with slow, clumsy movements and irregular timing; has difficulty alternating from supination to pronation C. Finger to Nose and to the Nurse’s fingers Normal findings Performs with coordination and rapidly Deviation from normal Misses the finger and moves slowly B. Toe or Ball of Foot to the Nurse’s Fingers Normal findings Moves smoothly, with coordination Deviation from normal Misses your finger; cannot coordinate movement (Hinid ko sure kung part pa ba ito for lower extremities) Light-Touch Sensation Normal findings Light tickling or touch sensation Deviation from normal Anesthesia, hyperesthesia, hypoesthesia or paresthesia D. Fingers to fingers Normal findings Performs with accuracy and rapidity Pain sensation Normal findings Able to discriminate “sharp” and “dull” sensations Deviation from normal Moves slowly and is unable to touch fingers consistently Deviation from normal Areas of reduced, heightened, or absent sensation (map them for recording purposes) E. Fingers to Thumb (same hand) Normal findings Rapidly touches each finger to thumb with each hand Temperature sensation Not normally done if client’s pain sensation is intact Normal findings Able to discriminate between “hot” or “cold” sensations Deviation from normal Cannot coordinate this fine discrete movement with either one or both hands Fine Motor Tests for the Lower Extremities Done in a supine position A. Heel down opposite Shin Normal findings Demonstrates bilateral equal coordination Deviation from normal Has tremors or is awkward; heel moves off shin Deviation from normal Areas of dulled or lost sensation Position or Kinesthetic sensation Normal findings Can readily determine the position of fingers and toes Deviation from normal Unable to determine the position of one or more fingers or toes Assessment of the Musculo-Skeletal System Nursing Assessment Health history Pain Bone – dull, deep ache “boring” in nature Fx-sharp and piercing relieved by immobility Muscle-soreness Paresthesia Burning, tingling sensation or numbness Diet High purine diet Family history Allergy Physical Exam Gait Smoothness and rhythm Shuffling gait Ataxic gait is an unsteady, uncoordinated walk with a wide base of support and the feet thrown outward. Festinating gait Antalgic gait an abnormal pattern of walking secondary to pain that ultimately causes a limp, whereby the stance phase is shortened relative to the swing phase. Posture Kyphosis - an increased front-to-back curve of the spine Lordosis - the inward curve of the lumbar spine (just above the buttocks) Scoliosis - abnormal lateral curvature of the spine. Bone integrity Deformities and alignment Joint function Range of motion Effusion (presence of fluid) Crepitus (abnormal sound) Neurovascular function Assessment of the CNS Circulation Motion Sensation Indicators of Peripheral Neurovascular Dysfunction Circulation Color: pale or cyanotic Temperature: cool Capillary refill: more than 3 seconds Sensation Paresthesia Pain Pain on passive stretch Absence of feeling Motion Weakness Paralysis Assessing Joints Inspect size, shape, color, and symmetry. Note any masses, deformities, or muscle atrophy Palpate for edema, heat, tenderness, pain, nodules, or crepitus Test each joint’s range of motion (ROM) Assessing Muscles Test muscle strength by asking the client to move each extremity through its full ROM against reference Rating 5 4 3 2 1 0 Explanation Active motion against full resistance Active motion against some resistance Active motion against gravity Passive ROM (gravity removed and assisted by examiner) Slight flicker of contraction No muscular contraction Strength classification Normal Slight weakness Average weakness Poor ROM Severe weakness paralysis