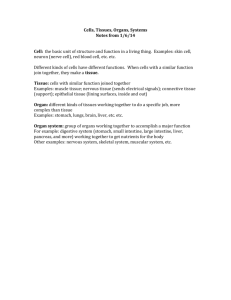
Topic 2:The Digestive Tract MIS505 Reetika G Pillay Learning outcomes 1. Describe the macroscopic and microscope structure and function of the gastrointestinal system. 2. Describe how the above systems function and interact with each other and the rest of the body to maintain homeostasis. 3. Apply the knowledge of anatomy and physiology to medical imaging studies. 4. Be able to label the GIT structures on Barium Study images. 2 ▪ The GI tract (gastrointestinal tract) The muscular alimentary canal ▪ Mouth ▪ Pharynx ▪ Esophagus ▪ Stomach ▪ Small intestine ▪ Large intestine ▪ Anus ▪ The accessory digestive organs Supply secretions contributing to the breakdown of food ▪ Teeth & tongue ▪ Salivary glands ▪ Gallbladder ▪ Liver ▪ Pancreas 3 The Digestive Process ▪ Ingestion ▪ Taking in food through the mouth ▪ Propulsion (movement of food) ▪ Swallowing ▪ Peristalsis – propulsion by alternate contraction &relaxation ▪ Mechanical digestion ▪ Chewing ▪ Churning in stomach ▪ Mixing by segmentation ▪ Chemical digestion ▪ By secreted enzymes: see later ▪ Absorption ▪ Transport of digested end products into blood and lymph in wall of canal ▪ Defecation ▪ Elimination of indigestible substances from body as feces 4 ▪ Chemical digestion ▪ Complex food molecules (carbohydrates, proteins and lipids) broken down into chemical building blocks (simple sugars, amino acids, and fatty acids and glycerol) ▪ Carried out by enzymes secreted by digestive glands into lumen of the alimentary canal 5 Ways to divide…. The more common Plus: epigastric periumbilical suprapubic flank 6 Histology of alimentary canal wall Same four layers from esophagus to anal canal 1. Mucosa 2. Submucosa 3. Muscularis externa 4. Serosa from lumen (inside) out 7 Inner layer: the mucosa* (mucous membrane) Three sub-layers * 1. Lining epithelium 2. Lamina propria 3. Muscularis mucosae 8 More about the mucosa ▪ Epithelium: absorbs nutrients, secretes mucus ▪ Continuous with ducts and secretory cells of intrinsic digestive glands (those within the wall) ▪ Extrinsic (accessory) glands: the larger ones such as liver and pancreas ▪ Lamina propria ▪ Loose connective tissue with nourishing and absorbing capillaries ▪ Contains most of mucosa-associated lymphoid tissue (MALT) ▪ Muscularis mucosae ▪ Thin layer of muscle producing only local movements 9 Second layer: the submucosa* * ▪ Connective tissue containing major blood and lymphatic vessels and nerves ▪ Many elastic fibers so gut can regain shape after food passes 10 Next in, the muscularis externa* (AKA just “muscularis”) Two layers of smooth muscle responsible for peristalsis and segmentation ▪ Inner circular layer (circumferential) * ▪ ▪ ▪ Squeezes In some places forms sphincters (act as valves) Outer longitudinal layer: shortens gut 11 Last (outer), the serosa* (the visceral peritoneum) ▪ Simple squamous epithelium (mesothelium) ▪ Thin layer of areolar connective tissue underneath ▪ Exceptions: * ▪ Parts not in peritoneal cavity have adventitia, lack serosa ▪ Some have both, e.g. retroperitoneal organs 12 Smooth muscle Smooth muscle 6 major locations: •Muscles are spindle-shaped cells •One central nucleus •Grouped into sheets: often running perpendicular to each other •Peristalsis •No striations (no sarcomeres) •Contractions are slow, sustained and resistant to fatigue •Does not always require a nervous signal: can be stimulated by stretching or hormones 1. inside the eye 2. walls of vessels 3. respiratory tubes 4. digestive tubes 5. urinary organs 6. reproductive organs 13 Nerves ▪ Enteric nervous system: the gut’s own ▪ Visceral plexuses within gut wall controlling the muscles, glands and having sensory info ▪ Myenteric: in muscularis ▪ Submucosal ▪ 100 million neurons! (as many as the spinal cord) ▪ Autonomic input: speeds or slows the system ▪ Parasympathetic ▪ Stimulates digestive functions ▪ Sympathetic ▪ Inhibits digestion ▪ Largely automatic 14 Review of some definitions…. ▪ Peritoneum: serous membranes of the abdominopelvic cavity ▪ Visceral peritoneum: covers external surfaces of most digestive organs ▪ Parietal peritoneum: lines body wall ▪ Peritoneal cavity: slit-like potential space between visceral and parietal peritoneum ▪ Serous fluid – lubricating 15 New definitions ▪ Mesentery ▪ ▪ ▪ ▪ ▪ Double layer of peritoneum Extends to digestive organs from body wall Hold organs in place Sites of fat storage Route by which circulatory vessels and nerves reach organs ▪ Most are dorsal ▪ Extend dorsally from gut to posterior abdominal wall ▪ Ventral mesentery – from stomach and liver to anterior abdominal wall ▪ Some mesenteries are called “ligaments” though not technically such 16 Mesenteries ▪ Note dorsal, ventral and formation of retroperitoneal position 17 Mesenteries ▪ Two ventral mesenteries ▪ Falciform “ligament” * ▪ Binds anterior aspect of liver to anterior abdominal wall and diaphragm ▪ Lesser omentum (=“fatty skin”) – see diagram* ▪ All other mesenteries are dorsal (posterior) 18 Mesenteries continued (all these are dorsal) ▪ Greater omentum ▪ ▪ ▪ ▪ ▪ Connects stomach to posterior abdominal wall – very roundabout Wraps around spleen: gastrosplenic ligament Continues dorsally as splenorenal ligament A lot of fat Limits spread of infection by wrapping around inflamed e.g. appendix ▪ “Mesentery” or mesentery proper ▪ Supports long coils of jejunum and ileum (parts of small intestine) ▪ Transverse mesocolon ▪ Transverse colon held to posterior abdominal wall ▪ Nearly horizontal sheet fused to underside of greater omentum ▪ Sigmoid mesocolon ▪ Connects sigmoid colon to posterior abdominal wall see next slides for pics… 19 Note mesenteries: falciform ligament, lesser omentum, greater omentum 20 Note: greater omentum, lesser omentum, falciform ligament, transverse mesocolon, mesentery, sigmoid mesocolon 21 Some organs are “retroperitoneal” ▪ ▪ ▪ ▪ Are “behind the peritoneum” Fused to posterior (dorsal) abdominal wall Lack a mesentery Include: ▪ ▪ ▪ ▪ ▪ Most of duodenum (1st part of small intestine) Ascending colon Descending colon Rectum Pancreas ▪ Tend to cause back pain, instead of abdominal pain (This is as opposed to the organs which are intraperitoneal, or just “peritoneal”) 22 The Mouth ▪ Mouth = oral cavity ▪ Lining: thick stratified squamous epithelium ▪ Lips- orbicularis oris muscle ▪ Cheeks – buccinator muscle 23 ▪ “Vermillion border” or red border ▪ Between highly keratinized skin of face and mucosa of mouth ▪ Needs moisture ▪ Note frenulums (folds of mucosa) ▪ Palate – roof of mouth ▪ Hard plate anteriorly ▪ Soft palate posterioly ▪ Uvula 24 ▪ Tongue Mostly muscles ▪ ▪ ▪ ▪ ▪ ▪ ▪ Grip and reposition food Forms “bolus” of food (lump) Help in swallowing Speech – help form some consonants Note frenulum on previous slide: can be too tight Taste buds contained by circumvallate and fungiform papillae Lingual tonsil – back of tongue 25 Teeth ▪ Called “dentition” (like dentist) ▪ Teeth live in sockets (alveoli) in the gumcovered margins of the mandible and maxilla ▪ Chewing: raising and lowering the mandible and moving it from side to side while tongue positions food between teeth 26 Teeth ▪ Two sets ▪ Primary or deciduous ▪ “Baby” teeth ▪ Start at 6 months ▪ 20 are out by about 2 years ▪ Fall out between 2-6 years ▪ Permanent: 32 total ▪ All but 3rd set of molars by end of adolescence ▪ 3rd set = “wisdom teeth” – Variable ▪ Some can be “impacted” (imbedded in bone) 27 Teeth are classified according to shape and function incisor canine premolar molar ▪ Incisors: chisel-shaped for chopping off pieces ▪ Canines: cone shaped to tear and pierce ▪ Premolars (bicuspids) and ▪ Molars - broad crowns with 4-5 rounded cusps for grinding Cusps are surface bumps 28 Tooth structure ▪ Two main regions A. Crown (exposed) B. Root (in socket) C. Meet at neck ▪ Enamel ▪ ▪ ▪ ▪ 99% calcium crystals Hardest substance in body Dentin – bulk of the tooth (bone-like but harder than bone, with collagen and mineral) Pulp cavity with vessels and nerves ▪ Root canal: the part of the pulp in the root A C B 29 Tooth structure ▪ Cementum – bone layer of tooth root ▪ ▪ C Periodontal ligament ▪ ▪ ▪ ▪ Attaches tooth to periodontal ligament A Anchors tooth in boney socket of the jaw Continuous with gingiva (gums) B Cavities or caries - rot Plaque – film of sugar, bacteria and debris 30 Salivary glands (tuboalveolar glands) ▪ Intrinsic salivary glands – within mucosa ▪ Secrete saliva all the time to keep mouth moist ▪ Extrinsic salivary glands ▪ Paired (2 each) ▪ Parotid ▪ Submandibular ▪ Sublingual Saliva: mixture of water, ions, mucus, enzymes keep mouth moist dissolves food so can be tasted moistens food starts enzymatic digestion buffers acid antibacterial and antiviral ▪ External to mouth ▪ Ducts to mouth ▪ Secrete saliva only right before or during eating 31 Extrinsic salivary glands ▪ Parotids* - largest (think mumps) ▪ Facial nerve branch at risk during surgery here ▪ Submandibular # - medial surface mandible ▪ Sublingual + - under tongue; floor of mouth * + # Compound = duct branches Tubo = tubes Alveolar = sacs 32 Pharynx ___oropharynx ___laryngopharynx ▪ Oropharynx and laryngopharynx ▪ Stratified squamous epithelium ▪ Three constrictor muscles* ▪ Sequentially squeeze bolus of food into esophagus ▪ Are skeletal muscles * * ▪ Voluntary action ▪ Vagus nerve (X) * 33 Esophagus ▪ Continuation of pharynx in mid neck ▪ Muscular tube collapsed when lumen empty Esophagus___________ ▪ Descends through thorax ▪ On anterior surface of vertebral column ▪ Behind (posterior to) trachea * 34 Esophagus continued ▪ Passes through “esophageal hiatus” in the diaphragm to enter the abdomen ▪ Abdominal part only 2 cm long ▪ Joins stomach at cardiac orifice* ▪ Cardiac sphincter at cardiac orifice to prevent regurgitation (food coming back up into esophagus) ▪ Gastroesophageal junction and GERD ___________________esophageal hiatus (hiatus means opening) * 35 Microscopic anatomy of esophagus Contains all 4 layers (see right) ▪ Epithelium: nonkeratinized stratified squamous epithelium ▪ At GE junction – thin simple columnar epithelium ▪ ▪ Mucus glands in wall Muscle (muscularis externa) changes as it goes down ▪ Superior 1/3 of esophagus: skeletal muscle (like pharynx) ▪ Middle 1/3 mixture of skeletal and smooth muscle ▪ Inferior 1/3 smooth muscle (as in stomach and intestines) ▪ When empty, mucosa and submucosa lie in longitudinal folds 36 Esophagus histology 37 Stomach ▪ J-shaped; widest part of alimentary canal ▪ Temporary storage and mixing – 4 hours ▪ Into “chyme” ▪ Starts food breakdown ▪ Pepsin (protein-digesting enzyme needing acid environment) ▪ HCl (hydrochloric acid) helps kill bacteria ▪ Stomach tolerates high acid content but esophagus doesn’t – why it hurts so much when stomach contents refluxes into esophagus (heartburn; GERD) ▪ Most nutrients wait until get to small intestine to be absorbed; exceptions are: ▪ Water, electrolytes, some drugs like aspirin and alcohol (absorbed through stomach) 38 Stomach ▪ Lies mostly in LUQ epigastrium ▪ But pain can be epigastric or lower ▪ Just inferior to (below) diaphragm ▪ Anterior (in front of) spleen and pancreas ▪ Tucked under left lower margin of liver junction with ▪ Anchored at both ends but esophagus mobile in between contains pyloric ▪ Main regions in drawing to sphincter right-------------------------------▪ Capacity: 1.5 L food; max funnel shaped capacity 4L (1 gallon) dome 39 40 Stomach Regions ▪ Cardiac region ▪ Fundus (dome shaped) ▪ Body ▪ Greater curvature ▪ Lesser curvature ▪ Pyloric region ▪ Antrum ▪ Canal ▪ Sphincter dome junction with esophagus contains pyloric sphincter funnel shaped 41 ▪ Rugae: longitudinal folds on internal surface (helps distensibility) ▪ Muscularis: additional innermost oblique layer (along with circular and longitudinal layers) 42 Histology of stomach ▪ Simple columnar epithelium: secrete bicarbonate-buffered mucus ▪ Gastric pits opening into gastric glands ▪ Mucus neck cells ▪ Parietal cells ▪ HCL ▪ Intrinsic factor (for B12 absorption) ▪ Chief cells ▪ Pepsinogen (activated to pepsin with HCL) ▪ Stimulated by gastrin: a stomach hormone 43 Small intestine ▪ Longest part of alimentary canal (2.7-5 m) ▪ Most enzymatic digestion occurs here ▪ Most enzymes secreted by pancreas, not small intestine ▪ Almost all absorption of nutrients ▪ 3-6 hour process ▪ Runs from pyloric sphincter to RLQ Small intestine___________ 44 ▪ Small intestine has 3 subdivisions ▪ Duodenum – 5% of length ▪ Jejunum – almost 40% ▪ Ileum – almost 60% Blood supply: superior mesenteric artery; Veins drain into hepatic portal vein Duodenum is retroperitoneal (stuck down under peritoneum); others are loose Duodenum receives bile from liver and gallbladder via bile duct* enzymes from pancreas via main pancreatic duct* * * 45 ▪ Small intestine designed for absorption ▪ Huge surface area because of great length ▪ Structural modifications also increase absorptive area ▪ Circular folds (plicae circulares) ▪ Villi (fingerlike projections) 1 mm high – simple columnar epithelium: velvety ▪ Microvilli * Absorptivie cell with microvilli to increase surface area & many mitochondria: nutrient uptake is energydemanding Lacteal*: network of blood and lymph capillaries -Carbs and proteins into blood to liver via hepatic portal vein -Fat into lymph: fat-soluble toxins e.g. pesticides circulate systemically before going to liver for detoxification 46 ▪ Intestinal crypts * (of Lieberkuhn) inbetween villi ▪ Cells here divide every 3-6 days to renew epithelium (most rapidly dividing cells of the body) ▪ Secrete watery intestinal juice which mixes with chyme (the paste that food becomes after stomach churns it) ▪ Intestinal flora – the permanent normal bacteria ▪ Manufacture some vitamins, e.g. K, which get absorbed * Duodenal glands •Mucus to counteract acidity from stomach •Hormones: Cholecystokinin (stimulates GB to release stored bile, also pancreas) Secretin (stimulates pancreatic ducts to release acid neutralizer) * * -have many mitochondria: nutrient uptake is energydemanding -produce mucus 47 General histology of digestive tract 48 49 Large intestine Digested residue reaches it Main function: to absorb water and electrolytes Subdivisions Cecum Appendix Colon Rectum Anal canal 50 Three special features 1. Teniae coli (3 longitudinal muscle strips) 2. Haustra (puckering into sacs) 3. Epiploic appendages (omental or fat pouches) 3. 2. 1. 51 Colon has segments: ascending, transverse and descending colon; then sigmoid colon Right angle turns: hepatic flexure* in RUQ and splenic flexure* in LUQ * * Between ileum and cecum S-shaped 1st part Blind tube Movement sluggish and weak except for a few “mass peristaltic movements” per day to force feces toward rectum powerfully 52 ▪ Rectum ▪ In pelvis ▪ No teniae ▪ Strong longitudinal muscle layer ▪ Has valves ▪ Anal canal ▪ Pectinate line* ▪ Inferior to it: sensitive to pain ▪ Hemorrhoids (enlarged veins) ▪ Superior to pectinate line: internal ▪ Inferior to pectinate line: external * * ▪ Sphincters (close opening) ▪ Internal* – smooth muscle – involuntary * ▪ External* – skeletal muscle – voluntary 53 ▪ Defecation 1. Triggered by stretching of wall, mediated by spinal cord parasympathetic reflex 2. Stimulates contraction of smooth muscle in wall and relaxation of internal anal sphincter 3. If convenient to defecate voluntary motor neurons stimulate relaxation of external anal sphincter (aided by diaphragm and abdominal wall muscles called Valsalva maneuver) 54 Histology – large intestine ▪ No villi ▪ Fewer nutrients absorbed ▪ “Columnar cells” in pic = absorptive cells ▪ Take in water and electrolytes ▪ A lot of goblet cells for mucus ▪ Lubricates stool ▪ More lymphoid tissue ▪ A lot of bacteria in stool 55 The Liver ▪ Largest gland in the body (about 3 pounds) ▪ Over 500 functions ▪ Inferior to diaphragm in RUQ and epigastric area protected by ribs ▪ R and L lobes ▪ Plus 2 smaller lobes ▪ Falciform ligament ▪ Mesentery binding liver to anterior abdominal wall ▪ 2 surfaces ▪ Diaphragmatic ▪ Visceral ▪ Covered by peritoneum ▪ Except “bare area” fused to diaphragm 56 posterior Fissure on visceral surface Porta hepatis: major vessels and nerves enter and leave - see pics Ligamentum teres: remnant of umbilical vein in fetus, attaches to navel – see next slide anterior 57 Fetal circulation Umbilical vein ___________ Ligamentum teres__________ Navel_______ 58 59 Just some of the liver’s repertoire ▪ ▪ ▪ ▪ ▪ ▪ ▪ Produces bile Picks up glucose from blood Stores glucose as glycogen Processes fats and amino acids Stores some vitamins Detoxifies poisons and drugs Makes the blood proteins 60 Liver histology ▪ Liver lobules (about one million of them) ▪ Hexagonal solid made of sheets of hepatocytes (liver cells) around a central vein ▪ Corners of lobules have “portal triads” (see next pic) 61 ▪ Portal triad ▪ Portal arteriole ▪ Portal venule ▪ Branch of hepatic portal vein ▪ Delivers substances from intestines for processing by hepatocytes ▪ Bile duct ▪ Carries bile away ▪ Liver sinusoids ▪ Large capillaries between plates of hepatocytes ▪ Contribute to central vein and ultimately to hepatic veins and IVC ▪ Kupffer cells ▪ Liver macrophages ▪ Old blood cells and microorganisms removed 62 63 Hepatocytes (liver cells) ▪ Many organelles ▪ Rough ER – manufactures blood proteins ▪ Smooth ER – help produce bile salts and detoxifies blood-borne poisons ▪ Peroxisomes – detoxify other poisons, including alcohol ▪ Golgi apparatus – packages ▪ Mitochondria – a lot of energy needed for all this ▪ Glycosomes - role in storing sugar and regulation of blood glucose (sugar) levels ▪ Produce 500-1000 ml bile each day ▪ Secrete into bile canaliculi (little channels) then ducts ▪ Regeneration capacity through liver stem cells 64 Gallbladder* ▪ ▪ ▪ ▪ ▪ Bile is produced in the liver Bile is stored in the gallbladder Bile is excreted into the duodenum when needed (fatty meal) Bile helps dissolve fat and cholesterol If bile salts crystallize, gall stones are formed ▪ Intermittent pain: ball valve effect causing intermittent obstruction ▪ Or infection and a lot of pain, fever, vomiting, etc. * 65 Lies in LUQ kind of behind stomach Is retroperitoneal Has a head, body and tail Head is in C-shaped curve of duodenum Tail extends left to touch spleen Main pancreatic duct runs the length of the pancreas, joins bile duct Pancreas (exocrine and endocrine) 66 67 one acinus Pancreatic exocrine function ▪ Compound acinar (saclike) glands opening into large ducts (therefore exocrine) ▪ Acinar cells make 22 kinds of enzymes ▪ Stored in zymogen granules ▪ Grape-like arrangement ▪ Enzymes to duodenum, where activated 68 Pancreatic endocrine function (hormones released into blood) ▪ Islets of Langerhans (AKA “islet cells”) are the hormone secreting cells ▪ Insulin (from beta cells) ▪ Lowers blood glucose (sugar) ▪ Glucagon (from from alpha cells) ▪ Raises blood glucose (sugar) (more later) 69 Endocrine cells: 70 Review ▪ Complete the topic study guide questions. 71 Reference: ▪ Chapter 24 - Gerard J. Tortora & Bryan H. Derrickson (2014), Principles of Anatomy and Physiology. (14th ed.), John Wiley & Sons, USA 72