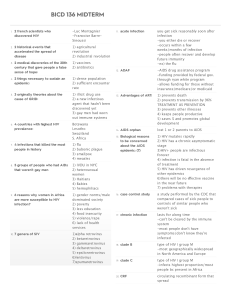
IMMUNE II Autoimmune Diseases • Rheumatoid arthritis • Sjogren syndrome • Systemic Lupus Erythematosus • Systemic sclerosis/ Scleroderma • >Inflammatory myopathies • >Mixed CT disease • >Polyarteritis nodosa Others 1. 2. 3. Inflammatory Myopathies Mixed Connective Tissue Disease 1. High titers of anti U1 RNP 2. Low incidence of renal disease 3. Good response to corticosteroids PAN and other vasculitides 1. Noninfectious necrotizing vasculitis Immunologic Deficiency Syndrome Can be: o o Primary immunodeficiency Secondary immunodeficiency PRIMARY IMMUNODEFICIENCY 1. X linked agammaglobulinemia of Bruton failure of precursor B cells to mature (Btk gene) Males are affected, disease is seen at 6 months Recurrent URTI (bacterial); GI problems (viral); G. lamblia; arthritis B cells are absent or decreased T cell mediated reaction are normal Mutation of Bruton tyrosine kinase (Btk) encoded by gene in the long arm of X chromosome at Xq21.22 Note: Defects in the Bruton tyrosine kinase (BTK) gene cause agammaglobulinemia. Agammaglobulinemia is characterized by failure to produce mature B lymphocyte cells and is associated with a failure of Ig heavy chain rearrangement. Two thirds of cases are familial, and one third of cases are believed to arise from new mutations. Mutations of the BTK gene are found in approximately 80% of patients with agammaglobulinemia. Prepared by: EGBII; 8-19-11 2. Common Variable Immunodeficiency Hypogammaglobulinemia usually affecting all ab classes but sometimes only IgG Both sexes affected Occurs later in childhood/adolescence Similar manifestations Risk of lymphoid malignancy; gastric cancer 3. Isolated IgA deficiency Common; Low levels of IgA in serum and secretion Increase frequency of Autoimmune dse Sinopulmonary infections and diarrhea 4. Hyper-IgM Syndrome T cell disorder; mutation at CD40 IgM is normal to increased but deficiency of IgG, IgA and IgE Reccurent pyogenic infections and Pneumocystis 5. Di George Syndrome T cell deficiency – failure of development rd th of the 3 and 4 pharyngeal pouch Deletion of Chromosome 22q11 Congenital defects: heart, BV, mouth, ears, facies Poor defense against viruses and fungal 6. Severe Combined Immunodeficiency dse Both humoral and cell mediated Infants – thrush, diaper rash and failure to thrive Infections to Candida, P. carinii, pseudomonas etc Most common: x-linked; defect yc of cytokine receptor, others are AR – defect in ADA Histologic: thymus hypoplasia and other lymphoid tissue Treatment: BM transplantation 7. Wiskott Aldrich Syndrome X linked, recessive; Thrombocytopenia, eczema, recurrent infections, early death WASP gene Thymus – normal, secondary T cell depletion in PB and T cell zones Low IgM; N IgG; high IgA and IgE Prone to develop malignant lymphoma 8. Genetic Deficiencies of the Complement System C2 deficiency– SLE like autoimmune dse Most common Properdin and factor D deficiency C3 deficiency – pyogenic infections and IC mediated GN C56789 – neisserial infections C1 – hereditary angioedema d/t release of vasoactive peptides Paroxysmal nocturnal hemoglobinuria SECONDARY IMMUNODEFICIENCY AIDS Caused by retrovirus HIV Signs & siymptoms: Opportunistic infections, secondary neoplasm and neurologic Manifestations Epidemiology Homosexual and bisexual men (>50 %) IV drug abusers (20%) Hemophiliacs (0.5%) Recipients of blood/blood components (1%) Heterosexual contacts (10%) Children under 13: 90% M-I transmission; 10% hemophiliacs etc 3 major ROT: 1. Sexual – 75%; virus is carried in semen, vaginal secretion and cervical cells 2 ways: direct inoculation in BV and into dendritic cells or CD4+ cells Etiology: Properties of HIV Retrovirus – family Lentivirus 2 forms: HIV 1 – US, Europe and Central Africa Most common in Philippines HIV2 – West Africa and India Can be : Male –to-male Male-to-female Female-to-male 2. Parenteral transmission A. IV drug abusers B. hemophiliacs – factor VIII and XI conc. C. random recipients of blood transfusion 3. Mother-Infant transmission A. In utero by transplacental route B. During delivery – infected birth canal C. After birth by ingestion of breast milk Cannot be transmitted by casual personal contact Seroconversion afer needle stick accident (health workers) 0.3% HIV STRUCTURE: Lipid envelope & core Core: o Major capsid protein (p24) Test against this* o Nucleocapsid protein (p7/p9) o 2 copies of genomic RNA (gag, pol, env genes) o 3 viral enzymes (protease, reverse transcriptase, integrase) * Dendritic cells of mucosa express CCR5 HIV life cycle Viral attachment Viral penetration/ fusion Uncoating Reverse transcription Nuclear entry Integration/ RNA transcription Protein Synthesis/ Protease cleavage Viral assembly/ Budding Pathogenesis 2 major targets: 1. Immune system, primarily cell mediated immunity Loss of CD4+T cell and Helper T cells Macrophages and dendritic cells 2. Central Nervous system CNS involvement: o Infects macrophages & microglia o HIV carried by monocytes to the brain o Neurons not infected o Indirectly caused by viral products & sol Fs from infected microglia Life Cycle of HIV CD4 molecules has a high affinity receptor for HIV(gp 120) Gp120 must bind to co-receptors (CCR5 and CXCR4) CCR5 – M tropic strains Macrophages, monocytes and freshly isolated blood T cells but not in vitro propagated T cells Acutely ill patients – 90% of cases are M tropic CXCR4 – T tropic strains Over the course of infection T tropic accumulate More virulent and cause final rapid phase of disease progression Prepared by: EGBII; 8-19-11 Mechanism of T cell Immunodeficiency Productive infection and viral replication in infected cells – cause lysis of CD4+Tcells 1-2 billion T cells die a day How they die 1. Activation induced cell death 2. Loss of immature precursors of CD4+Tcells 3. Fusion of infected and uninfected cells with formation of giant cells 4. Apoptosis of uninfected T cells Hallmark of AIDS – marked reduction in CD4+T cell Latent infection of T cells can remain in cells for months to years (0.05% of resting CD4+T cells in the LN) CD4+T cells produce cytokines: IL2, IL4, Il5, IFN, MCF and hematopoeitic GF. Major abnormalities in immune function – table 6-12 HIV Infection of Non-T Cells Macrophages and monocytes found in tissues Aspects of Macrophage infection Infect/multiply in terminally differentiated Macrophages due to vpr gene reservoir of infection Gatekeepers of infection Dendritic cells – mucosal and follicular Abnormality in B cell function Hypergammaglobulinemia due to polyclonal B cell activation Reinfection with CMV and EBV Gp 41 promotes B cell growth HIV infected macrophages produce IL6 Despite B cell activation – humoral immunity is impaired; disseminated infection by encapsulated bacteria: S pneumonia and H. influenzae CNS Involvement Macrophages and microglia HIV is carried by monocytes to the brain Neurons not infected Damage is caused by viral products produced by infected microglia: IL1, TNF, IL6, Nitric oxide Course of HIV Infection (phases) Acute retroviral syndrome Middle, chronic phase o Most are asymptomatic Clinical AIDS o Breakdown of host defenses Clinical Features Fever, weight loss, diarrhea, lymphadenopathy Opportunistic infections P/jiroveci Candidiasis Mycobacteria cryptococcosis Neurologic disease High incidence of tumors Kaposi sarcoma Non Hodgkins B cell lymphoma Cervical cancer Anal cancer Opportunistic Infection Herpes simplex Pneumocystis Carinii HIV -? Encephalitis CNS Lymphoma Effects of Antiretroviral Drug Therapy on the Clinical Course of HIV new antiretroviral drugs target viral reverse transcriptase, protease, and integrase given in combination to reduce the emergence of mutants that develop resistance Despite dramatic improvements, several complications associated with HIV infection and its treatment emerged antiretroviral therapy develop a paradoxical clinical deterioration Deterioration even if CD4+ T cell increased and viral load decreased Immune reconstitution inflammatory syndrome Prognosis of AIDS remains dismal Rejection of Tissue Transplants Mechanisms of Recognition and Rejection of Allografts complex process both cell-mediated immunity and circulating antibodies play a role recipient’s immune system recognizes the graft as foreign & attacks it 2 mechanisms: T-cell mediated mreactions Antibody mediated reactions T-cell mediated reactions Cellular rejection Destruction of graft cells by CD8+ CTLs & delayed hypersensitivity (CD$+ helper cells) 2 pathways of recognition o Direct o Indirect DIRECT o T4 cells of recipient recognize allogenic (donor) MHC molecules on APCs in the graft INDIRECT o Recipient T4 lymphos recognize MHC antigens of graft donor thru the recipient’s own APC Antibody mediated reactions Humoral rejection 2 forms o Hyperactue (+) preformed antidonor antibody in recipient’s circulation o Acute Unsensitized recipient “Rejection vasculitis” RENAL TRANSPLANT REJECTION 3 modes: Hyperacute (minutes to hours) o Preformed antidonors antibodies o Endothelial damage, fibrinoid necrosis Acute (w/in days to months/ years) o Humoral (vasculitis) o Cellular (mononuclear infiltrates) Chronic o Progressive renal failure, vascular changes LIVER TRANSPLANT REJECTION Acute rejection o Within 2 months, mixed inflammation in portal & central veins Chronic rejection o Inflammation, portal fibrosis, arteriolar thickening, bile ductular necrosis HEART TRANSPLANT REJECTION Acute cellular rejection o Lymphos, fiber necrosis Acute vascular rejection o Ig deposition in small arteries o Vasculitis BONE MARROW TRANSPLANT W problems: Immunodeficiency Graft versus Host disease (GVHD) o Donor lymphocytes attack recipient HLA antigens (deficient lymphos) o ACUTE – affects immune system, skin epithelia, liver, intestine o CHRONIC – extensive cutaneous injury Amyloidosis Amyloid – proteinaceous substance deposited between cells Amyloidosis – group of diseases having in common deposition of similar appearing proteins. Physical nature – continuous non branching fibrils Chemical nature – 95% fibril protein; 5% P component and glycoprotein; AL, AA, AB 3 most common 1. Amyloid light chain (AL) – 1. from PC contains Ig light chains from plasma cells; 2. deposition is associated with monoclonal B cell proliferation 2. Amyloid fibril protein (AA) – 1. non Ig, derived from liver; 2. circulates with HDL3, 3. Beta-amyloid (AB) – 1. found in Alzheimer disease Other proteins found transthyretin B2-microglobulin Prepared by: EGBII; 8-19-11 Prion protein – misfolded (CNS) *Classification (Table 6-15: Systemic and Localized) 2 general categories of CHONs: NORMAL CHONs o Within inferent tendency to fold improperly & form fibrils when production is increased MUTANT CHONs o Prone to misfolding & aggregation Classification Systemic o Primary o Secondary Localized SYSTEMIC – PRIMARY Immunocyte dyscrasias with amyloidosis o Most common form (some forms of plasma cells dyscrasias eg. Multiple myeloma) Reactive o Rheumatoid arthritis, heroin abuses, renal cell CA, hodgkin’s lymphoma Hemodialysis associated o Deposition of B2 microglobulin in synovium joints or tendon sheaths (carpal tunnel syndrome) Heredofamilial o Rare, most common AR, familial mediterreanea fever, elevated IL-1, gene for pyrin o AD – deposits on peripheral & autonomic nerves (polyneuropahies) LOCALIZED Involves single organ or tissue ENDOCRINE o Thyroid – medullary CA o Pancreas – islet tumors o Pheochromocytoma o Undifferentiated stomach CA AGING o Senile systemic amyloidosis (elderly) o Senile cardiac amyloidosis o Restrictive CMP & arrhythmias Common ORGANS involved Kidney – most common, most serious Spleen – “sago spleen”; lardaceous spleen Liver – total parenchymal replacement Heart – major organ involved in senile cases Others o Adrenal, thyroid, pituitary, GIT (macroglossia) PATHOGENESIS Related to abnormal CHON folding Systemic disease that may involve components of the immune system (only some forms of amyloidosis) Clinical recognition – appropriate biopsy specimen o H&E stain – amorphous hyaline extracellular o Differential stain: Congo red Greenish bifrengence with polarizing microspore)