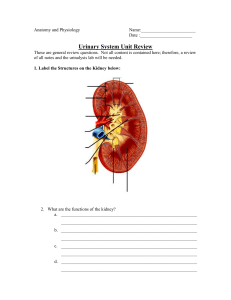
Adult Health II –study guide exam II Renal Lab Values Renal Anatomy Overview o Nephrons, located in parenchyma are composed of glomerulus and tubules. They either secrete or reabsorb ions and filtrates, fluid, waste products and electrolytes, acids, and bases o What does the kidney do? They filter our blood Acid/base balance Excrete waste/toxins Fluid/electrolyte balance Regulate BP –excrete renin RBC production is controlled by erythropoietin, which is secreted by kidney and then it stimulates bone marrow to produce RBCs Synthesize Vit D for calcium absorption/ and regulate parathyroid hormones Water homeostasis Fluid Balance o Urine is produced as blood is filtered through kidneys o Water/waste not reabsorbed = urine o Antidiuretic hormone (ADH) prompts kidneys to reabsorb water Produce in hypothalamus Produce when: 1) pt is dehydrated 2) high sodium intake and 3) decrease in blood volume Potassium o an increase in potassium = increase in aldosterone o aldosterone makes the distal convoluted tubules to secrete potassium, normalizing serum potassium levels o normal k levels: 3.5 -5 o lowered in diuretic use, raised in patients with kidney disease o hemodialysis will lower K level o potassium wasting diuretic: Lasix o potassium sparing diuretics: spironolactone o CBIGKDIE????? Calcium gluconate –stabilizing the membrane and preventing cardiac dysrhythmias Bicarbonate Insulin –moves K into cells Glucose Kayexalate –oral BUN o Normal 8-25 mg/dl o Blood urea nitrogen o Blood test which measure nitrogenous urea (product of protein metabolism) o Tells us how well the kidneys are clearing urea, if pt is dehydrated, amount of protein in diet, muscle breakdown, GI bleed, lack of profusion of the kidneys and this will cause an increase in the BUN o When BUN and creatinine levels increase together = possible renal dysfunction o Might be a little higher in men and in elderly patients o Over dehydrating, not eating enough = decrease in BUN Creatinine o Serum creatinine is useful in renal dysfunction when there is a large number of nephrons destroyed which can increase creatinine levels o normal 0.6 – 1.3 mg/dl o measures creatinine in blood, which is another product of protein and muscle metabolism o increase is seen when 50% of renal function is gone o could be elevated d/t dehydration o Seen as a better indicator of renal function o Also, patient specific, evaluated against the patient’s previous level Creatinine clearance o Evaluates how well the kidneys are working to remove creatinine from the blood o Blood and urine are taken It compares the serum creatinine level which the amount of creatine excreted in the urine that you’ve taken over a specific amount of time o o 24 hours urine collection is done then blood is taken checking to see what the kidneys are doing based on what’s in the blood have to be on ICE this is the best estimate of glomerular filtration rate (GFR) o diminishes as you age, the size and the function of kidney decreases with aging normal GFR: 125 ml/min (95 to 135) why is it important to know what someone’s GFR is? Because of medications, so if they are given to someone whose GFR is decreased and give them the same amount that you would give a normal GFR pt the patient would be at risk of toxicity Specific gravity o urine test o measurement of the kidneys ability to concentrate urine o normal 1.016 -1.022 o increased in poor intake of fluids, decreased kidney profusion, and increased ADH –urine is darker o decreased in high amount of fluid intake, DI, possible kidney disease Urine culture and sensitivity o Culture of urine may reveal bacteria in the urine Goal would be to identify specific bacteria or organisms so it can guide antibiotic therapy Culture results take about 24-48 hours to get them back o Sensitivity will tell us which antibiotics the bacteria are sensitive to o Remember to collect via clean catch: clean meatus/peri-area, collect midstream sample o Do not let sample sit=send it o How to get urine from a foley: o On insertion Clamp it and then use that little area closer up the tube (looter lock port) to get fresh urine from it Try to get a sample before you start them on antibiotics Renal and Urologic Problems –chapter 46 Upper and lower urinary o Defense mechanism against UTI is normal voiding, complete emptying of bladder, urine’s pH of less than 6 (acidic) which makes it bacteriostatic, high urea content and glycoproteins o Who might be at risk for UTI: neuro patients who end up with a neurogenic bladder problem, elderly who may lack a dysfunction bladder tone, enlarged prostate (BPH), probably the number one reason) and obstruction of outflow o What happens to back flow of the urine: hydro nephrosis and kidney stones o UTI comes from the outside in, so enters in the urethra and ascends up into the bladder and kidney o Most infections come via the urethra (cathing, cysto exam, poor hygiene, sexual activity) o S/S of kidney involvement: fever, chills, flank pain, elevated white count Urinary tract infection o Classification: upper or lower; complicated and uncomplicated infections; recurrent Uncomplicated infections: occur in normal urinary tract –like a 25-yr. old who takes meds and it goes away Complicated infections: present with a co-existing condition (obstruction, stones, catheters, DM, have increased risk of kidney damage, immunosuppressed) Recurrent infections: common o Etiology: often caused by gram negative bacteria o Clinical manifestations: LUTS: Emptying problems- weak urinary stream, hesitancy, post void dribbling, urinary retention or incomplete emptying, dysuria, pain on urination. Storage symptoms – urinary frequency, urgency, incontinence, nocturia, and nocturnal enuresis o Elderly is it more common to have systemic manifestations and they are confused Diagnostic studies: dipstick urinalysis, urinalysis, urine culture and sensitivity (C & S), clean catch, IVP, abd CT, renal ultrasound o Collaborative care: antibiotics based on C & S; Bactrim and Macrodantin are common tx for UTI; OTC Pyridium can help to sooth discomfort of painful urination (urine dk. orange) o Fluoroquinolones are used in complicated UTIs Difulcan if fungal Cipro is used frequently as well Nursing management: Relief from LUTS symptoms; prevention of upper urinary tract involvement. Health promotion- emptying bladder, hygiene (wiping front to back), 1800 ml fluid intake/day, limit catheter use (catheters are a HUGE risk factor for UTIs). Acute: fluid intake, local beat for discomfort, urinate every 3-4 hrs. to avoid cystitis. Home care: drug therapy for full course (so don’t stop taking it once you feel better). Evaluate expected outcomes Acute Pyelonephritis o Etiology: Begins in lower urinary track and ascends the urethra; unresolved bacterial infection can cause bacteremia that can lead to urosepsis (can be fatal) o Clinical manifestations: mild fatigue to onset of chills, fever, vomiting, flank pain (hallmark sign), and LUTS characteristics of cystitis, urinary urgency and frequency. Costovertebral angle (CVA) pain in the affected side CVA tenderness is a characteristic sign of polynephritis, a lot of pain the affected side o Diagnostic studies: urinalysis, urine shows pyuria, bacteremia, and hematuria; CBC, urine cultures, IVP later, might do some blood cultures o Collaborative care: severe infections may require hospitalization; mild symptoms can be treated outpatient for 14-21 days of antibiotics, IV fluids o Nursing management: Plan for: 1) return to normal renal function 2) pain relief, and 3) no recurring symptoms; early tx for cystitis to prevent polynephritis, educating on dx process and tx; evaluate expected outcomes. Encourage fluid intake of 8 glasses of fluid per day; encourage rest; educate about antibiotics (huge thing for this infection) o Chronic: kidney that has shrunk, and lost function from scarring from frequent infections. Diagnosed with radiologic imaging. Often progress to end stage renal failure (if chronic and inflamed), can cause sclerosis of the kidney o Can form an abscess can even form in the kidney from pyelonephritis Urethritis o Inflammation of the urethra o Etiology: bacterial or viral infection, trichomonas, chlamydia, gonorrhea In men, this is usually an STI Purulent c/d = gonococcal or chlamydia Clear d/c non-gonococcal o Clinical manifestations: difficult to diagnose in women o Diagnostic studies: urine cultures, you can also swab inside of the urethra o Collaborative care: treatment for organism o Nursing management: STD prevention; education for antibiotics; hygiene and abstention from sexual intercourse during treatment; suggest warm sitz baths; suggest that patient refer their partner for treatment also. Urethral Diverticula o The result of obstruction and rupture of the periurethral glands o Etiology: urethral trauma from childbirth; infections from gonococcal; o Clinical manifestations: dysuria, post void dribbling; urinary frequency and urgency, suprapubic discomfort, feeling of incomplete bladder emptying, o Diagnostic studies: urine, voiding cystourethrography, MRI, ultrasound o Collaborative care: surgical intervention –modifiable would be prevention and treatment of gonorrhea o Nursing management: education and care Interstitial Cystitis/Painful Bladder Syndrome (IC/PBS) o Chronic, painful inflammatory disease of the bladder causing frequency and urgency (Painful bladder syndrome) o Etiology: unknown but could be infection or autoimmune o Clinical manifestations: painful and bothersome LUTS. Suprapubic pain o Diagnostic studies: diagnosis of exclusion- symptoms of a UTI without the presence of a positive urine culture, bacteremia, or pyuria. Cystoscopic exam may show a small bladder capacity and superficial ulcerations called glomerulations in interstitial cystitis. o Collaborative care: avoid foods that are less likely to stimulate the bladder. Take Prelief, reduce stress, Elavil to reduce pain. o Nursing management: encourage bladder log/diary when voids and when pain comes on; eliminate bladder irritating foods i.e.- caffeine, alcohol, citrus, aged cheese, foods with vinegar, hot peppers and curry; avoid high-potency vitamins as they irritate the bladder, want to rule out a UTI, won’t be treating with antibiotics though Glomerulonephritis o affects both kidneys equally, 3rd leading cause or ESRD in the US o caused by: kidney infections, post-strep (d/t antibiotics depositing in the glomeruli, most common), viral infections, SLE, scleroderma, HTN, diabetic nephropathy, cells from lupus o Etiology: Immunologic processes involving the urinary tract predominantly affect the renal glomerulus. Two types of antibody-induced injury: 1) anti-GBM (glomular basement membrane) and 2) antibodies react with circulating nonglomerular antigens and can cause dysfunction of the nephrons o Clinical manifestations: hematuria-ranging from microscopic to gross and urinary secretion of various formed elements, including RBCs, WBCs, proteins, and casts. o Diagnostic studies: urine, CBC o Nursing Management: assess for exposure to drugs, immunizations bacterial and viral infections (hepatitis). Acute Post Streptococcal Glomerulonephritis o Etiology: Most common in children and young adults; develops 5 to 21 days after an infection of the tonsils, pharynx, or skin (e.g., streptococcal sore throat, impetigo) by nephrotoxic strains of group A b-hemolytic streptococci. o Clinical manifestations: generalized body edema, periorbital edema, hypertension, oliguria, hematuria (blood in the urine) with a smoky or rusty appearance, and proteinuria; fluid retention d/t decreased glomerular filtration. o Diagnostic studies: urine, CBC, and complete H & P (any recent sore throats or skin infections) o Collaborative care: encourage early diagnosis and treatment of sore throats and skin lesions. Rest, sodium and fluid restriction, diuretics, anti-hypertensive medication, adjust protein as determined by BUN level; antibiotics and corticosteroids as needed o Nursing management: rest, edema and hypertension management (PRIORITY), and dietary protein restriction when an increase in nitrogenous wastes (e.g. elevated BUN value) is present, strict I&Os, daily weight, monitor their labs Nephrotic Syndrome o Results when the glomerulus is excessively permeable to plasma protein, causing proteinuria that leads to low plasma albumin and tissue edema. o Etiology: glomerular disease, infections, neoplasm, allergens, drugs (NSAIDs), and multisystem diseases (e.g.-DM). o Clinical manifestations: edema; flank pain that indicates renal vein thrombosis (risk for clots and possible PE) losing proteins also losing clotting factors o Diagnostic studies: urine, CBC. Monitor albumin levels (You will see a decrease in serum albumin and protein causing hypoalbuminemia. This cause fluid to shift out of the vascular system into surrounding tissue causing ascites and anasarca (massive edema). o Decreased plasma oncotic pressure from decreased proteins = increased hepatic lipoprotein synthesis = HLD Collaborative care: Treatment is supportive and symptomatic. Edema- ACE inhibitors for edema, low protein and sodium diet, corticosteroid, lipid-lowering meds. o Nursing management: major nursing interventions for a patient with nephrotic syndrome are related to edema. Edema is assessed by weighing the patient daily, accurately recording intake and output, and measuring abdominal girth or extremity size. Restrict sodium in diet. Skin assessment and prevention of breakdown. Monitor dietary intake. Safety from infection. Urinary tract obstructions o Fluids dilute the urine, so drink plenty of fluids o If the calculi are in the place where it will block the flow from the urine, you can see the backup of the urine and cause pain, it can stretch and make the tissue of the kidney dysfunctional Urinary Tract Calculi o Classification: Five (5) major categories of stones (Lithiasis) are (1) calcium phosphate, (2) calcium oxalate, (3) uric acid, (4) cystine, and (5) struvite. Calcium oxalate is the most common stone and comes from: plant based things and meat, patient should avoid spinach, dark roughage, asparagus, cabbage, tomatoes, chocolate, tea o Etiology: Urinary stones cause clinical manifestations when they obstruct urinary flow. Common sites of complete obstruction are at the UPJ (the point where the ureter crosses the iliac vessels) and at the ureterovesical junction (UVJ). The backup of the urine is what is causing the pain o Clinical manifestations: pain, costovertebral flank pain or colicky terrible renal pain o Diagnostic studies: CBC, Chemistry, urine (make sure there’s no bacteria or WBC in), x-ray, CT, IVP (inject IV dye), metabolic panel to make sure the patient is not dehydrated or any electrolyte imbalances o Collaborative care: treatment of the symptoms of pain, infection, or obstruction. Lithotripsy is used to eliminate calculi from the urinary tract (shock wave treatment). Outcome for lithotripsy is based on stone size, stone location, and stone composition. Open surgery for obese patient to remove stone, stent placement if need. o Nursing management: (1) relief of pain, (2) no urinary tract obstruction, and (3) an understanding of measures to prevent further recurrence of stones. fluids, Dietary modifications based on the stone type (purine, calcium or oxalate) Educate on straining urine at home to return to clinic with stones for evaluation. IVP (intravenous pyelogram) o Dye is injected and an X-ray is taken o Assess for dye allergy Lithotripsy o Simple stones too large to pass though, ultrasound shock waves are delivered externally and they crush stones and then the smaller pieces pass out of body in the urine Kidney Stones o are in the minor and major calyces of the kidney and in the ureter Strictures o A stricture is a narrowing of the lumen of the ureter or urethra. Ureteral strictures can affect the entire length of the ureter. o Etiology: A urethral stricture is the result of fibrosis or inflammation of the urethral lumen. Causes of urethral strictures include scarring, trauma, urethritis, iatrogenic, or a congenital defect. Urethritis after gonococcal infection. o Latrogenic means r/t a medical exam or treatment, repeated catheterization, for example Clinical manifestations: diminished force of the urinary stream, straining to void, sprayed stream, postvoid dribbling, or a split-urine stream. o Diagnostic studies: retrograde urethrography (RUG), voiding cystourethrography (VCUG) o Collaborative care: stent placement to help prevent backflow or outflow obstruction o Nursing management: Post treatment surgical care, monitor I & O, pain management, monitor for bleeding Renal Trauma o Majority occur in men under the age of 30. o Sports injuries, traffic accidents, falls, penetrating wounds from gunshots or stabbing. o Findings: gross hematuria o Diag: UA, IVP with cystography and ultrasound, CT and MRI. Renal arteriography may also be used (try to look at the flow) o Tx: bedrest, fluids, analgesia, prep for surgery if necessary, if bleeding too much might end up hypovolemic o Nsg: Monitor for shock, assess, I & O, monitor urine for hematuria, fluids, comfort and pain mgmt., monitor for nephrotoxic antibiotics or any medications that are impaired due to renal injury. Renal Vascular Problems: Sclerosis, Stenosis, and Thrombosis o Vascular problems involving the kidney include: (1) Nephrosclerosis- treat with antihypertensives aggressively, want to try to relax the vessels and get the flow going (2) Renal artery stenosis- treat with surgery to restore vascular flow with angioplasty and stent; control HTN; surgical intervention may be possible. (3) Renal vein thrombosis- treat with anticoagulants, may end up on a heparin drip Hereditary Renal Diseases o Etiology: Polycystic kidney disease (PKD) is a life-threatening genetic disease. It is characterized by cysts that enlarge and destroy surrounding tissue by compression. Manifests between 30-40 years, no treatment o Most patients end up with hypertension and it’s possible that this is the first thing they end up with o Nephrectomy may be necessary with dialysis or kidney transplant Polycystic Kidney Disease o Most common life threatening genetic disease in the world. o Etiology: Genetic- autosomal recessive and dominant traits. Offspring have a 50% chance of getting if one parent has. o Clinical manifestations: palpable large kidneys, no early symptoms, HTN, hematuria, UTI, chronic pain o Diagnostic studies: CT Diagnosis is based on clinical manifestations, family history, IVP, ultrasound (best screening measure, can look at the structures of the kidneys), or CT scan. o Collaborative care: prevent infections esp. UTIs; nephrectomy and eventually kidney transplant o Nursing management: diet modification (sodium restriction), fluid restriction, drugs, (ACEs and ARBs) assist with chronic Disease process, counseling because of the Genetic nature of the disease. Urinary Instrumentation Review o Review types of instrumentation: Urethral catheterization- inserted through external meatus, indwelling catheter, foley (always look at how many cc’s the balloon is inflated with) Ureteral catheterization- through renal pelvis Suprapubic catheterization- inserted under general anesthesia Nephrostomy tubes- inserted into the pelvis of the kidney Intermittent catheterization- straight cath or “in-and-out cath”. Used often with patients with neurogenic bladder who have spinal cord injuries and neurologic diseases (or bladder outlet obstruction for men). Procedure for home care: cath 3-5 hours, hand hygiene with soap and water only**, lubricant, dry and place in a pouch and change catheter every 7 days. **Use sterile technique for acute or extended care facilities. Urinary diversion o Diversion to the skin that requires an appliance. Most common is an ileal conduit. Continent urinary diversions and orthotropic bladder reconstruction. o Pre-op mgmt: educate on procedure, fear, and anxiety; living with appliance; sexual activity. o Post-op mgmt: atelectasis, shock, increased risk for thrombosis, SBO, and UTI. Keep NPO, mgmt. of NG, maintain urine output, encourage fluid intake when able to take in clear liquids. Educate on catheterization and pouch and skin care. Male Reproductive Problems –Chapter 55 Benign Prostate Hyperplasia (BPH) o Enlargement of prostate gland resulting from increase in number of epithelial cells and connective tissue o Most common urologic problem in male adults o About 50% of all men will develop BPH in their lifetime. o Etiology and Pathophysiology BPH is not completely understood but is thought to result from hormonal changes from aging process Excessive accumulation of dihydroxytestosterone DHT in the prostate cells that can stimulate overgrowth of prostate tissue o DHT is the principal intraprostatic androgen in the cells of the prostate Increased proportion of estrogen over testosterone in blood so decreased testosterone in the blood Decrease in amount and force of the urinary stream due to compressed urethra. Typically, BPH develops in the inner part of the prostate. Prostate cancer is most likely to develop in the outer part. This enlargement gradually compresses the urethra, eventually leading to partial or complete obstruction. It is the compression of the urethra that ultimately leads to the development of clinical symptoms. o Risk Factors Aging Obesity: Especially increased waist circumference Lack of physical activity o Alcohol consumption Erectile dysfunction Smoking Diabetes Clinical Manifestations Irritative symptoms Symptoms associated with inflammation or infection o Urinary frequency and urgency, Dysuria, Bladder pain, Nocturia, Incontinence Obstructive symptoms Symptoms due to urinary retention o Decrease in caliber and force of urinary stream o Difficulty in initiating urination o Intermittency o o o Starting and stopping stream several times while voiding Dribbling at end of urinating Other findings and complications Nocturia often the first symptom noticed. Acute urinary retention Complication with sudden, painful inability to urinate Treatment involves catheter insertion and possible surgery. UTI and sepsis- Incomplete bladder emptying causes bacterial growth Calculi may develop in bladder Renal failure d/t obstruction Pyelonephritis –kidney infection Potential for bladder damage by having too much urine in the bladder Make sure they can void after you pull out their foley Diagnostic Studies History and physical exam Urinalysis with culture done to determine the presence of infection, the presence of bacteria, white blood cells, or microscopic, hematuria is an indication of infection or inflammation PSA level: blood test may be done to rule out prostate cancer, however they may be slightly elevated in patients with BPH Serum creatinine Neurologic exam Digital rectal exam o to R/O kidney problems abnormal DRE and PSA will require a TRUS Collaborative Care Goals: Restore bladder drainage. Relieve symptoms. Prevent/treat complications. Treatment based on symptoms and presence of complications Conservative Therapy Active surveillance o Lack of presence of symptoms o Mild symptoms (AUA score of 0-7) Symptoms may disappear. Lifestyle changes may result in improvement. American Urological Association (AUA) Symptom Index o Seven questions used to determine severity of prostate problems o Drug Therapy Score: mild 0-7 , moderate 8-19, severe 20-35 Alternatives to surgical intervention for some patients now include drug therapy and minimally invasive procedures. Drugs include 5α-reductase inhibitors and α-adrenergic receptor blockers. Combination therapy using both types of these drugs has been shown to be more effective in reducing symptoms than using one drug alone. finasteride (Proscar)- risk ortho hypotenstion; pregnant women avoid touch meds o dutasteride (Avodart) o Jalyn (finasteride + tamsulosin) ↓ Size of prostate gland Takes 3 to 6 months for improvement Side effects: decreased libido, decreased volume of ejaculation, ED May lower the risk of prostate cancer Not recommended in the prevention of prostate cancer due to an increased risk of developing an aggressive form of prostate cancer Finasteride is an appropriate treatment option for individuals who have moderate to severe symptom scores on the AUA symptom index. The drug must be taken on a continuous basis to maintain therapeutic results. Serum PSA levels are decreased by almost 50% when taking finasteride. Therefore, PSA levels should be doubled when comparing the patient’s current levels to premedication levels. tamsulosin (Flomax) doxazosin (Cardura) silodosin (Rapaflo) Promotes smooth muscle relaxation in prostate, facilitates urinary flow Improvement in 2 to 3 weeks Offer symptomatic relief but do not treat hyperplasia Erectogenic (erection causing) Drugs o Tadalifil (Cialis) effectively reduces symptoms of both BPH and ED. Herbal Therapy Saw palmetto has been used but no research supporting success Saxifrage, betasitosterol, Pyguem africanum, and Cernilton are also promoted but varied success Collaborative Care Minimally Invasive Therapy Transurethral Microwave Therapy (TUMT) o Outpatient procedure o Delivers microwaves directly to prostate through a transurethral probe o Heat causes death of tissue and relief of obstruction. o Postop urinary retention is common. o Patient sent home with catheter for 2 to 7 days. o Antibiotics, pain medication, and bladder antispasmodic medications given o Not appropriate therapy when rectal problems exist o Side effects: bladder spasm, hematuria, dysuria, and retention o Outpatient 90 min o Monitor for clots, tissue o Meds: Antibiotics, pain meds, antispasmodics Transurethral Needle Ablation (TUNA) o Only prostate tissue in direct contact with the needle is affected, thus allowing greater precision in removal of the target tissue. o The extent of tissue removed by this process is determined by the amount of tissue contact (needle length), amount of energy delivered, and duration of treatment. o Uses needle to ↑ temperature of prostate tissue for localized necrosis o Low-wave frequency used o Only tissue in contact with needle affected o Majority of patients show improvement in symptoms. o Outpatient uses local anesthesia and sedation. o Lasts 30 minutes with little pain and quick recovery o Complications include urinary retention, UTI, and irritative voiding symptoms. o Some patients require a catheter. o Hematuria up to a week Laser Prostatectomy o A variety of laser procedures use different sources, wavelengths, and delivery systems. o Retreatment rates are comparable to those of a transurethral resection of the prostate (TURP). o VLAP uses the laser beam to produce deep coagulation necrosis of the prostate. The affected prostate tissue gradually sloughs in the urinary stream. o Delivers a laser beam transurethrally to cut or destroy parts of the prostate o Common procedure: visual laser ablation of the prostate (VLAP) o o Takes several weeks to reach optimal results Urinary catheter inserted Contact laser techniques Minimal bleeding during and after procedure Fast recovery time Patients may take anticoagulants. Photovaporization of prostate Intraprostatic Urethral Stents o For patients who are poor surgical candidates o Stents are placed directly into prostatic tissue. o Chronic pain, infection, and encrustation are potential complications. Invasive (Surgery) Therapy Invasive therapy is indicated when: o Decrease in urine flow sufficient to cause discomfort o Persistent residual urine o Acute urinary retention o Hydronephrosis- swelling and damage to one or both kidney d/t retention. Not a primary disease; secondary to obstruction. Transurethral Resection (TURP) o Considered the gold standard surgical treatment of obstructing BPH o Removal of obstructing prostate tissue using resectoscope inserted through urethra o Outcome for 80% to 90% is excellent. o Relatively low risk o Performed under spinal or general anesthesia and requires hospital stay o Bladder irrigated for first 24 hours to prevent mucous and blood clots o Complications include bleeding, clot retention, hyponatremia, retrograde ejaculation (goes back into where it came from sometimes) o Patients must stop anticoagulants before surgery o Nursing management: managing the three 3 catheter Transurethral incision of the prostate (TUIP) o Moderate to severe symptoms o For patients with a small or moderately enlarged prostate gland o Local anesthesia Several small incisions made into prostate to expand the urethra improves urine flow. o Medications o o o Estrogen or testosterone supplementation History and teaching: Surgery or previous treatment for BPH Knowledge of condition Voluntary fluid restriction Outpatient procedure Nursing Diagnosis and Planning Acute pain Risk for infection Bleeding post term Make sure they are draining their bladder Goals for patient having invasive procedures Restoration of urinary damage Treatment of UTI Understanding of o Upcoming procedure o Implications for sexual functioning o Urinary control Goals for postoperative care No complications Restoration of urinary control Complete bladder emptying Satisfactory sexual expression Postop care: o Postoperative bladder irrigation to remove blood clots and ensure drainage or urine Administer antispasmodics. Teach Kegel exercises. Preoperative care for TURP o Restore urinary drainage Coude – curved-tip catheter Filiform – rigid catheter Aseptic technique very important in preventing infection Administer antibiotics Treat UTIs Provide patient opportunity to express concerns over alterations in sexual function. Inform patient of possible complications of procedures. Postoperative care for TURP Assess for complications Hemorrhage and clots in urine Bladder spasms Urinary incontinence Infection The plan of care should be adjusted to the type of surgery, the reasons for surgery, and the patient’s response to surgery. o Nursing Implementation TURP Postoperative care for TURP Observe patient for signs of infection. Dietary intervention Stool softeners to prevent straining Straining increases intra-abdominal pressure, which can lead to bleeding at the operative site. A diet high in fiber facilitates the passage of stool. o Instructions after prostate surgery Care of indwelling catheter Managing incontinence Maintaining adequate fluid intake Observing for signs and symptoms of UTI, wound infection Ambulatory and Home Care- TURP Instructions after prostate surgery Preventing constipation Avoiding heavy lifting o Not more than 10 lb or 4.5 kg Refraining from driving, intercourse after surgery as directed Sexual counseling if erectile dysfunction becomes a problem Avoiding bladder irritants Yearly digital rectal examination (DRE) if they are over the age they will need their PSA level checked PROSTATITIS o Inflammatory and non-inflammatory conditions affecting the prostate. o Could be caused by an STI in younger men and in older patient’s its usually bacterial and chronic o Can be acute or chronic o Most common urological disorder o 12% of men will get and 2 million get annually o Bacterial or viral o Clinical Manifestations: o o o o Fever Chills Back pain Perineal pain Dysuria Urinary frequency, urgency, and cloudy Prostate might feel tender and warm to touch And a white d/c from the penis Diagnostics UA and culture CBC –to see if there's a white count infection PSA Nursing and Collaborative Management Antibiotics: trimethoprim/sulfamethoxozole, ciprofloxin, carbachol, carbenicillin, cephalexin, doxycycline Anti-inflammatory (help with the pain): NSAIDs, indomethacin Possible urinary catheter Encourage fluids Manage fever Can be in a warm sitz water tub Problems of the Penis: Congenital Problems Hydrospadias- urethra is located on the ventral side of the penis. Surgical repair may be necessary with chordee (downward curvature of penis during erection) Prepuce (foreskin) problems Phimosis- tightening or constriction off the foreskin; cause by poor hygiene. Ice pack for edema, topical corticosteroid 2-3 x day. Paraphimosis- tightening of the foreskin in the retracted position. Warm soaks, cleaning glans and foreskin, antibiotics, and possible circumcision o Problems with Erectile Mechanism Priapism A painful erection that lasts more than 6 hours. Is a medical emergency Risks/causes: DM, sickle cell, spinal cord trauma, medications, sildenafil (Viagra) Tissue necrosis: worried about getting adequate oxygen flow to the penis Peyronie’s disease Curved or crooked penis cause by plaque formation of the cavernosa of the penis or possible trauma. May have pain. o Not dangerous Can cause pain during erections, ED, or embarrassment Tx: med- collagenase Clostridium histolyticum to break down collagen Surgical correction may be scheduled after 1 year of med tx. Problems of the Scrotum and Testes Epididymitis Acute, painful inflammation of the epididymis Men under 40 cause oftwwen gonorrhea or chlamydial infection; older men often UTI and prostatitis Antibiotics both partners (gonorrhea) Tx: Elevate scrotum, ice packs, and analgesics. Ambulation increases pain May end up with fever and chills Orchitis Acute inflammation of the testis Painful, swollen, and tender Can be bacterial or viral infection (mumps, pneumonia, TB, syphilis. Also trauma, influenza, complicate UTI, and catheterization o o Mumps orchitis could cause sterility if contracted as a child; encourage immunizations Tx: antibiotics specific to bacteria, pain meds, and elevate scrotum Problems of the Scrotum Congenital Bilaterally or unilaterally Increases risk for testicular CA if not corrected by age 2 Surgery to correct by locating testes to the scrotum Acquired problems of scrotum and testes o Hydrocele Non-tender, fluid filled mass. Lumph interference Diagnosis: Transillumination with a flashlight can display mass Tx: none unless scrotum becomes large and uncomfortable then aspiration or surgical drainage Spermatocele Sperm filled cyst in epididymis Diagnosis: Transillumination Unknown cause Tx: surgical removal Monitor for scrotal lumps that could indicate testicular CA Varicocele Dilation of veins that drain testes Scrotum feels wormlike with palpation Tx: Surgery if patient is sterile Testicular Torsion Twisting of the spermatic cord that supplies blood to testes and epididytimis Common in men < age 20; trauma, or anatomic abnormalities S/S: pain, tender, swelling, N/V Diag: scan of testes or Doppler US Surgical emergency within 4-6 hours or ischemia to testes Sexual function Vasectomy Bilateral surgical or ligation of the vas deferens to cause sterility. Some reversal has been successful. Outpatient: 15-30 min under local anesthesia Monitor for hematoma and swelling Total of 10 ejaculations or 6 weeks to evacuate sperm. Advise contraception Erectile Dysfunction (ED) Inability to maintain erection Can occur in 50% of men between 40-70 for numerous causes see Table 55-10 Dx: self-report, IIEF, and through history and physical exam Labs: Glucose, lipids, BMP, PSA, and CBC to rule out or determine other underlying problems Function: Erectogenic drugs taken 30-60 min before intended sexual activity; monitor for hypotension Other options: Vacuum constriction devices- suction device Intraurethral devices- topical gel injected into the urethra of the penis; papaverine, alprostadil or phetolamine; massage, 10 min to take effect Penile implants- surgical impants; for severe ED, small pump in scrotum to inflate, could have mechanical failure Sexual counseling- before, during, and after treatments; focus on psychological and interpersonal Nursing Management: Emotional support, ensure confidentiality; routine health assessments Andropause Gradual decline in male hormone with aging Can begin as early as age 40 S/S: loss of libido, fatigue, ED, depressions, mood swings, sleep disturbances Labs: Testosterone; normal 280-1000 ng/dL; replacement at 200 Replacement: gel (Testim, Androderm), injections (cypoinate); oral can cause liver damage; underarm (Axiron), and buccal (Striant) Avoid contact with pregnant, childbearing age women and children Handwashing with soap and water after gel or cream application Infertility Inability to conceive after 1 year of frequent, unprotected sex. Most common cause of male infertility is varicocele First test: semen analysis for concentration, motility, and morphology Other labs: plasma testosterone, LH and FSH Nursing and collaborative management: concern and tactful; lifestyle changes, in vitro, and counseling ACUTE RENAL INJURY AND CHRONIC KIDNEY DISEASE ACUTE KIDNEY INJURY o THE RAPID LOSS OF KIDNEY FUNCTION FROM RENAL CELL DAMAGE o CAN BE REVERSIBLE BUT HAS A HIGH MORTALITY RATE o CAN DEVELOP OVER HOURS OR DAYS o INCREASES IN BLOOD UREA NITROGEN (BUN), CREATININE, AND POTASSIUM o MORTALITY RATE HOSPITALIZED- 1 IN 5; CRITICAL CARE 70-80% o AZOTEMIA: ACCUMULATION OF WASTE PRODUCTS IN BLOOD o CAUSES OF AKI PRERENAL HYPOVOLEMIA DECREASED CARDIAC OUTPUT: SOMEONE WITH A HEART DISEASE DECREASED PERIPHERAL VASCULAR RESISTANCE: SHOCK DECREASED RENOVASCULAR BLOOD FLOW: STENOSIS OF THE RENAL ARTERIES, BLOOD CLOTS, ACUTE TUBULAR NECROSIS CAN HAPPEN Intrarenal Nephrotoxic injury: drugs (contrast dye, aminoglycosides) ischemia Interstitial nephritis Other causes POSTRENAL BPH: can have an obstruction that causes black up to the kidney Bladder CA Prostate CA Calculi Neuromuscular disorders: MS, Parkinson's disease, Spinal cord disease Strictures Trauma PRERENAL Prerenal is an issue with systemic circulation and decreased renal blood flow. This is an issue with volume depletion and reduced blood flow to the kidneys, which means nephrons aren’t getting oxygen. This occurs before damage to kidney and giving the patient fluid to increase volume could o reverse the AKI or stop CKD from happening. CAN BE CAUSED BY: SHOCK ⇣ PROFUSION OF THE KIDNEYS (DECREASED CO, SUCH AS MI) HYPOVOLEMIA LIVER FAILURE ARTERY STENOSIS, THROMBUS INTRARENAL Intrarenal is direct damage to kidney tissue resulting in impaired nephron function, which could be due to ischemia, drugs (aminoglycosides, other abx, contrast dye, etc.) ATN: is the most common type of intrarenal problem where drugs or ischemia cause destruction of the epithelium (sepsis, blood tx reaction). In these causes, damage to kidney is caused by lack of oxygen and acute tubular necrosis TRAUMA TO THE KIDNEY VENOUS STENOSIS OR THROMBOSIS NEPHROTOXIC DRUGS CONTRAST DYE BLOOD TRANSFUSION REACTION INFECTION VASCULITIS: COULD BE AUTOIMMUNE OR COULD BE CAUSED BY AN REACTION ACUTE GLOMERULONEPHRITIS: COMMON REASON WE HAVE THIS IS POST STREP POSTRENAL Postrenal: mechanical obstruction in the outflow of urine. If untreated, could have hydronephrosis, tubular atrophy and irreversible kidney fibrosis NEUROGENIC BLADDER: SPINAL CORD PT, STONES TUMORS BPH URETHRAL STRICTURE: COME ON DUE TO LONG TERM INFECTIONS SCI THIS IS AN OUTFLOW PROBLEM PATIENT TEACHING Drink plenty of fluids (up to 2 L per day). If needed, talk with provider regarding any needed restriction (CKD, HF) Decreased the risk of UTI and kidney stones Smoking Cessation Number one reason why we end up with bladder cancer Healthy BMI Use NSAIDs with caution o o Take this with food, and do not go over the max. daily dose Major complicating co-morbid conditions include HTN and DM Antibiotic usage-complete course, report s/s of UTI/Pyelonephritis Monitor their renal function, labs CLINICAL MANIFESTATIONS PRE AND POSTRENAL AKI ARE OFTEN RESOLVED BY TREATING THE CAUSE IF INTRARENAL IS DAMAGED, AKI HAS A LONGER RECOVERY PERIOD PATIENTS WITH AKI PROGRESS THROUGH PHASES: OLIGURIC, DIURETIC, AND RECOVERY. IF RECOVERY PHASE DOES NOT OCCUR, CKD MAY DEVELOP PHASES OF ACUTE KIDNEY INJURY o o o ASSESSMENT AND LABS Can obtain a 24-hour urine, creatinine clearance, to assess GFR This patient could have tachyypnea HISTORY AND PHYSICAL TO DETERMINE CAUSE DECLINE IN URINE OUTPUT (SEE RIFLE) HYPOVOLEMIA: H&H RISE, BP DROP, EDEMA HYPERTENSION URINE PROTEINURIA IF DAMAGE TO GLOMERULUS (INTRA) CBC (MONITOR FOR SIGNS OF INFECTION) SERUM INCREASES CREATININE (BEST INDICATOR) AND BUN BASIC METABOLIC PANEL: HYPERKALEMIA OR HYPOKALEMIA, HYPONATREMIA, HYPOCALCEMIA, HYPERPHOSPHATEMIA MORE ASSESSMENT FINDINGS Fluid and Electrolyte Imbalance Fluid overload or fluid deficit Hyperkalemia or hypokalemia Hyponatremia Hypocalcemia Hyperphosphatemia Metabolic acidosis Inability to excrete waste Uremia Neuro---fatigue and difficulty concentrating all the way to seizures, stupor, and coma, change in their LOC Wave changes Kidneys normally excrete 80-90% of the body’s potassium. o o o o In kidney injury, there can be increase potassium retained, or hyperkalemia. Metabolic acidosis worsens in hyperkalemia. An increase in potassium= peaked T waves, a widening QRS and ST depression PUT THIS PATIENT ON TELE Cardio wise, the patient can have fluid overload, edema, dysrhythmias COLLABORATIVE CARE REMOVE AND TREAT PRECIPITATING CAUSE POSSIBLE FLUID CHALLENGE WITH DIURETICS FLUID RESTRICTION RESTRICT EXCESS SODIUM, PHOSPHATE, AND POTASSIUM MONITOR ELECTROLYTES (ESPECIALLY K+) Treat hyperkalemia as needed Calcium supplements or phosphate-binding agents NUTRITIONAL THERAPY: PARENTERAL, ENTERAL TO MAINTAIN CALORIC AND PROTEIN INTAKE DIALYSIS INITIATION IF INDICATED Diet: adequate calories to prevent catabolism; energy should be from high carb and fat sources; protein based upon clinical condition—could be restricted, normal; potassium and sodium usually restricted Acute I/O-STRICT Daily wt with same scale, same time each day If on abx, monitor renal function Diet will be low sodium, low potassium, low protein. TREATING HYPERKALEMIA* REGULAR INSULIN IV- HELPS TO MOVE K+ INTO CELLS SODIUM BICARB IV- CORRECTS ACIDOSIS AND MOVES K+ INTO CELLS CALCIUM GLUCONATE IV- RAISES THE THRESHOLD FOR EXCITATION FROM K+, CARDIAC STABILIZING HEMODIALYSIS- MOST EFFECTIVE WAY TO REMOVE K+, WOULD BE THE LAST STEP FOR THIS SODIUM POLYSTYRENE SULFONATE (KAYEXALATE)- EXCHANGE OF NA FOR K+; ORAL OR RETENTION ENEMA CREATES DIARRHEA AND REMOVES K+ DIETARY RESTRICTION- LIMIT INTAKE TO 40 MEQ DAY OF POTASSIUM RICH FOODS AND DRINK Greens, bananas, potatoes, EXAMPLE NURSING DIAGNOSIS AND COLLABORATIVE PROBLEMS EXCESSIVE FLUID VOLUME RISK FOR INFECTION Getting a central line for dialysis FATIGUE ANXIETY POTENTIAL COMPLICATION: DYSRHYTHMIAS GERIATRIC CONSIDERATIONS MORE SUSCEPTIBLE TO AKI DEHYDRATION MORE FREQUENT HYPOTENSION NEED FOR DIURETIC THERAPY, RISK FOR HYPOTENSION URINARY OBSTRUCTIVE PROBLEMS (BPH, STRICTURES, ETC.) MORE DIFFICULT TO RECOVER FROM AKI THE OLDER YOU ARE Decrease in renal function as the patient ages=changes in GFR=possible changes in drug dosing At risk for build up for drug metabolites, and might be more sensitive to insulin/opioids/etc CHRONIC KIDNEY DISEASE o o o o o o o o o PROGRESSIVE, IRREVERSIBLE LOSS OF KIDNEY FUNCTION DIABETES AND HYPERTENSION ARE THE LEADING CAUSES WITH VASCULAR AND CARDIAC IMPLICATIONS PROGNOSIS DEPENDS ON ETIOLOGY, CONDITION, AGE, AND FOLLOW-UP INCREASED RISK WITH AFRICAN AMERICANS AND AMERICAN INDIANS MOST COMMON CAUSE OF DEATH IS CARDIAC RELATED CLINICAL MANIFESTATIONS ANEMIA DYSRHTHMIAS HTN KUSSMAUL BREATHING DYSPNEA ULCERATIONS IN THE GI TRACT; POSSIBLE GI BLEED LETHARGY MALNUTRITION CONSTIPATION PERIPHERAL NEUOPATHY LEG CRAMPS OSTEOMALACIA CALCIUM DEPOSITS IN THE EYE PRURITUS INFERTILITY AND DECREASED LIBIDO FATIGUE DEPRESSION PERSONALITY AND BEHAVIOR CHANGES GLOMERULAR FILTRATION RATE (GFR) GFR , 60 ML/MIN FOR > 3 MONTHS (NORMAL GFR IS ABOUT 125 ML/MIN) CKD STAGES: Stage1: GFR ³ 90 Diag and treat Stage 2: GFR 60-89 Treat and monitor progress Stage 3: GFR 30-59 Eval and treat complications Stage 4: GFR 15-29 (dialysis, kidney transplant) Stage 5: < 15 (for dialysis) Uremia is a syndrome when the body systems become affected due to decreased kidney fx. This is dangerous and will usually occur in the final stages of CKD. Pt may have fatigue, nausea, anorexia, and confusion A decrease in GFR=an increase in BUN and Creatinine, defective carb metabolism, insulin insensitivity, hyperinsulnemia, Also, insulin isn’t excreted, so increased insulin = increased hepaticproduction of triglycerides CKD ASSESSMENT AND LABS H&P DIPSTICK URINALYSIS TO DETECT FOR EXCESS PROTEIN IN URINE-MICROALBUMINURIA RENAL ULTRASOUND TO MEASURE KIDNEY AND RULE OUT OBSTRUCTIONS RENAL SCAN CT LABS: BUN/CREAT, CREATININE CLEARANCE, URINALYSIS, ELECTROLYTES, CBC- DECREASED RBC (DECREASED KIDNEY PRODUCTION OF ERYTHROPOIETIN) AND HG/HCT RENAL BIOPSY COLLABORATIVE CARE Goal to preserve kidney function, reduce the risks of CV, and prevent future damage DRUG THERAPY: TX FOR ELEVATED K+ LEVELS ANTIHYPERTENSIVES, ANTI-LIPID, DIURETICS, CALCIUM AND PHOSPHATE BINDERS FOR CKD-MBD VIT D, ERYTHROPOIETIN (LOW DOSE) FOR ANEMIA 2-3 TIMES A WEEK NUTRITIONAL THERAPY: TABLE 47-10 Restrict K+ rich foods for hyperkalemia; protein, water, sodium, potassium, calcium, and phosphate Caloric intake: 1.2 g/kg/day o CKD- NURSING MANAGEMENT ASSESS- HISTORY AND FAMILY HX, MEDICATION USE, DIETARY HABITS, HEIGHT, WEIGHT, VS NSG DIAG: 10 EXCESS FLUID VOLUMES, 2) RISK FOR ELECTROLYTE IMBALANCE, 3) IMBALANCED NUTRITION: LESS THAN BODY PLAN: 1) DEMONSTRATE KNOWLEDGE OF THERAPEUTIC REGIMEN, 2) PARTICIPATE IN DECISION MAKING, 3) DEMONSTRATIVE EFFECTIVE COPING, 4) CONTINUE ADLS WITHIN LIMITS IMPLEMENT: ACUTE MGMT.; EDUCATION FOR AMBULATORY AND HOME CARE; AND HEALTH PROMOTIONONGOING MONITORING TO PREVENT FURTHER INJURY EVAL: FLUID AND ELECTROLYTES WNL, ACCEPTABLE WEIGHT ESRD-WHAT TO DO? o DIALYSIS MOVEMENT OF FLUID/MOLECULES ACROSS A SEMIPERMEABLE MEMBRANE FROM ONE COMPARTMENT TO ANOTHER USED TO CORRECT FLUID/ELECTROLYTE IMBALANCES AND TO REMOVE WASTE PRODUCTS IN RENAL FAILURE TREAT DRUG OVERDOSES ESKD ARE TREATED WITH DIALYSIS; KIDNEY DONORS LIMITED PERITONEAL DIALYSIS o COMPLICATIONS OF PERITONEAL DIALYSIS Exit site infection Peritonitis Hernias Lower back problems Bleeding Pulmonary complications Protein loss as much as 40 g/day o HEMODIALYSIS COMPLICATIONS OF HEMODIALYSIS Hypotension- rapid removal of vascular volume (tx: decrease the fluid being removed) Muscle cramps- reduce the rate of fluid removal Hepatitis- prevalent in dialysis pts EFFECTIVENESS OF HEMODIALYSIS IS POSITIVE FOR TREATING SYMPTOMS o KIDNEY TRANSPLANT TISSUE MUST BE MATCHED TO A DONOR CAN BE FROM CADAVER OR FAMILY MEMBER FAMILY TRANSPLANT FROM LIVING DONOR HAVE BEST OUTCOMES AVERAGE WAIT TIME 3-5 YEARS PATIENT IS IMMUNOSUPPRESSED RISK FOR INFECTION ANTI-REJECTION DRUGS SUCH AS TACROLIMUS (PROGRAF) ARE USED-RISK FOR INFECTION, LYMPHOMAS NEPHROTOXIC MEDICATION REVIEW o AMINOGLYCOSIDES o AMPHOTERICIN B o NSAIDS o ACE INHIBITORS o ARBS o IV CONTRAST DYE RENAL MEDICATION o PHOSPHATE BINDERS o CALCIUM CARBONATE (TUMS) o SEVELAMER (RENVELA) o FOSRENOL o PHOSLO o PHOSPHORUS LEVEL (3-5.5 NORMAL RANGE) o DIET MODIFICATION o TAKE BINDERS WITH FOOD RENAL DIET