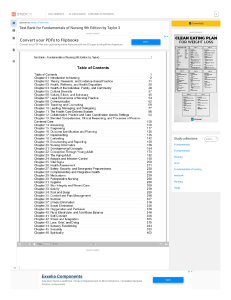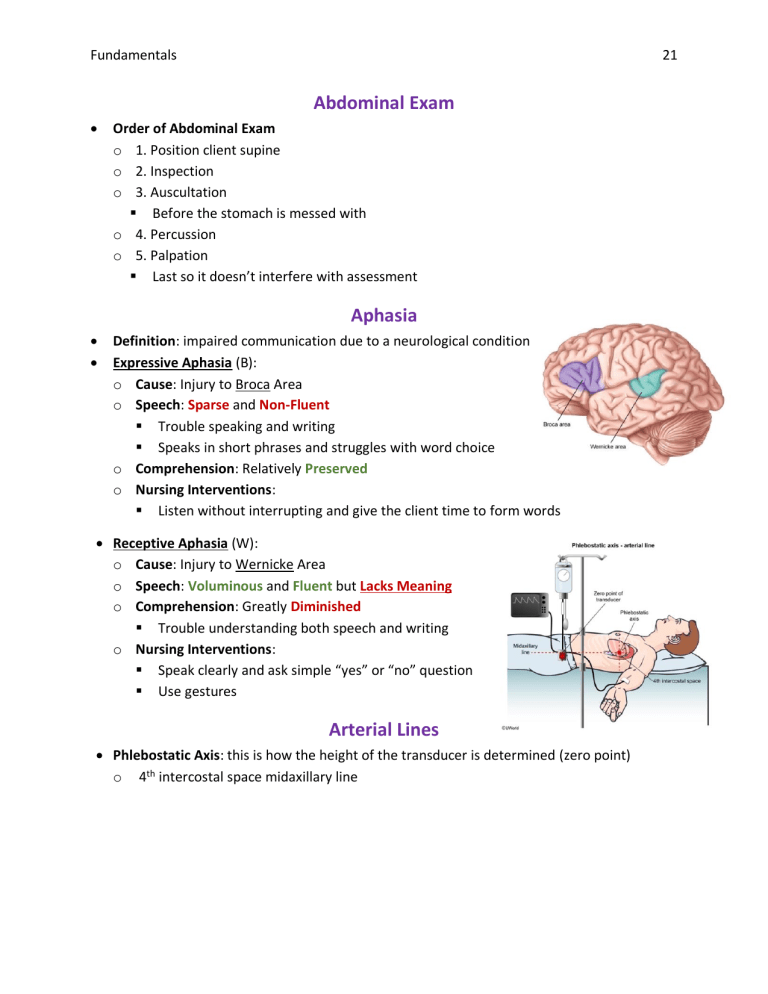
Fundamentals 21 Abdominal Exam • Order of Abdominal Exam o 1. Position client supine o 2. Inspection o 3. Auscultation ▪ Before the stomach is messed with o 4. Percussion o 5. Palpation ▪ Last so it doesn’t interfere with assessment Aphasia • • Definition: impaired communication due to a neurological condition Expressive Aphasia (B): o Cause: Injury to Broca Area o Speech: Sparse and Non-Fluent ▪ Trouble speaking and writing ▪ Speaks in short phrases and struggles with word choice o Comprehension: Relatively Preserved o Nursing Interventions: ▪ Listen without interrupting and give the client time to form words • Receptive Aphasia (W): o Cause: Injury to Wernicke Area o Speech: Voluminous and Fluent but Lacks Meaning o Comprehension: Greatly Diminished ▪ Trouble understanding both speech and writing o Nursing Interventions: ▪ Speak clearly and ask simple “yes” or “no” question ▪ Use gestures Arterial Lines • Phlebostatic Axis: this is how the height of the transducer is determined (zero point) o 4th intercostal space midaxillary line Fundamentals 22 Barium Enema • • • • • Purpose: o Uses fluoroscopy to visualize the colon with contrast ▪ Can detect polyps, ulcers, tumors, and diverticula Contraindications: o Acute Diverticulitis ▪ Risk of Rupture Side Effects: o Abdominal Cramping o Urge to Defecate Pre-Op Teaching: o Take a cathartic to empty stool from the colon ▪ Magnesium Citrate or Polyethylene Glycol o Clear Liquid Diet the day before o NPO 8 hours before Post-Op Teaching: o Expect passage of chalky, white stool from barium contrast o Take a laxative to help expel the barium and prevent fecal impaction ▪ Magnesium Hydroxide o Drink lots of fluid to promote hydrate and eat high-fiber diet Beck’s Triad • Cardiac Tamponade (Three Most Prominent Signs): o Hypotension / Narrow Pulse Pressure o Muffled Heart Sounds o Neck Vein Distension Blood Products • • Nursing Considerations: o Ensure that the blood isn’t more than a week old o Two RN’s must verify compatibility o Use filtered Y tubing for blood transfusions (infuse one unit at a time) o Prime tubing with 0.9% sodium chloride ▪ Clamp this side of the tubing during the infusion, open to flush after o The RN must take the first vital signs after 15 minutes o The blood must be started in 30 minutes, or it should be returned to the bank Transfusion Reaction o Manifestations: Fundamentals 23 ▪ Shortness of Breath ▪ Chest Tightness ▪ Fever ▪ Lower Back Pain ▪ Anxiety ▪ Tachycardia and Hypotension o Treatment: ▪ Discontinue Blood Products and Call HCP ▪ Administer 0.9% NS through a different port ▪ Monitor Breath Sounds Brachytherapy • • • • Definition: Internal radiation treatment that is ingested, injected, or implanted Indications: Cancer treatment Permanent Brachytherapy: Only emits low doses of radiation that does not affect others Temporary Brachytherapy: Require safety precautions because it poses a risk to other o Example: Sealed Cervical Radium Implants o Nursing Care: ▪ Use Appropriate Shielding to Limit Exposure • Place client in a lead room and use lead shields / aprons ▪ Limit Each Person’s Exposure to the Client • Cluster care to limit exposure to 30 minutes per shift ▪ All Assigned Staff Need a Dosimeter Badge • This measures the radiation exposure ▪ Place Client on Bedrest and Prevent Repositioning • Necessary to avoid device dislodgement ▪ Maximize Distance from Client • 6 feet is recommended Bronchoscopy • • • Purpose: used to visualize larynx, trachea, bronchi, obtain tissue biopsy Indications: o Diagnosis o Remove Foreign Object Nursing Considerations: o Requires informed consent o Provide local anesthetic throat spray o Administer medications as prescribed: Fundamentals • • 24 ▪ Atropine to reduce oral secretions ▪ Sedation or Anti-Anxiety medications o Keep patient upright for procedure Patient Education: o Remain NPO 8-12 hours beforehand ▪ To reduce risk of aspiration Post-Procedure Care: o Assess for Return of Gag Reflex ▪ This is a priority to decrease the risk of aspiration o Monitor for Bleeding o Monitor Respiratory Status, Vital Signs, and LOC Cane • • • • • • Cane Size: o From greater trochanter to the floor (wearing shoes) Cane Positioning: o Always hold cane on the stronger side o 6-10 inches to the side of the body Cane Advancing: o Move cane forward 6-10 inches forward, then move affected leg o Last, move stronger leg PAST the cane o May also have the client move the affected leg and cane at the SAME TIME ▪ This is for clients needing minimal support Climbing Stairs with Cane: o First, step with stronger leg o Next, move the cane while bearing weight on strong leg o Last, bring up the weaker leg Descending Stairs with Cane: o First, lead with the cane o Next, bring down the weaker leg o Last, step down the stronger leg Pneumonic: “up with the good and down with the bad” o The cane always moves before the weaker leg Cardiac Catheterization • • Definition: a catheter is advanced to the heart through a vein Indications: o Diagnosis of Coronary Artery Disease o Treatment of Aortic Stenosis Fundamentals • • • • • • 25 Complications: o Arterial Bleeds (Hypovolemic Shock and Death) ▪ Watch for reduced warmth in the lower extremity of insertion site Contrast Contraindications: o Allergy o Metformin Use (hold 24-48 hours before IV contrast) o Renal Impairment Side Effects: o Flushing o Metallic Taste Patient Education: o NPO for 6 hours before the procedure o Lie flat with leg straight for several hours following the procedure o Engage in quiet activities for 24 hours o Drink plenty of fluids to flush out contrast dye and prevent dehydration Pre-Op Care: o Verify informed consent o Shave the area before the procedure o Mark the distal (baseline) pulses – pedal and radial o Ensure adequate renal function for safe contrast dye use o Verify that the client doesn’t have an allergy to dye or shellfish Post-Op Care: o Apply a pressure dressing to the wound ▪ Monitor for signs of bleeding or hematoma at the insertion site o Monitor vital signs, lower pulses, sensation, and capillary refill ▪ Every 15 minutes for the first 2 to 4 hours ▪ Report any chest pain o Have client keep the leg straight for 4 to 6 hours o Maintain bed rest (immobilization) with no sitting or hip flexion o Increase fluid intake to flush out the dye o If bleeding occurs, apply direct manual pressure 1 inch above the puncture ▪ Notify HCP after pressure is applied Central Venous Access • Maintenance: o Ensure correct placement with chest x-ray o Monitor insertion site for infection o Use strict surgical asepsis for dressing changes (every 72 hours) Fundamentals • • 26 o To draw blood, discard first collection of blood for good results o Flush line prior to specimen collection Infection: o Signs of Infection: Fever, Chills, Redness o Complications: Sepsis o Treatment: ▪ Remove CVC as soon as possible ▪ Obtain Blood Cultures ▪ Begin Antibiotics Removal: o Goal = Prevent Air Embolism o Have the client lie supine to increase pressure and decrease the possibility of air getting into the vessel o Instruct the client to bear down or exhale ▪ NEVER inhale because it would suck air into the blood vessel o Apply an air occlusive dressing to help prevent a delayed air embolism ▪ Ex. Tegaderm o NEVER pull harder if you are met with resistance pulling out the catheter ▪ This could cause it to break and become dislodged in the vessel Chest Physiotherapy • • • • • • Definition: a technique of airway clearance o Can be done manually with a cupped hand or with a HFCWO vest Indications: o Cystic Fibrosis Manual Percussion: o Use a cupped hand to clap onto the chest o This is sometimes followed by vibration on the same spot o Have the client cough / deep breathe, as well as reposition HFCWO Vest: o This vest inflates and deflates rapidly to cause vibration over the chest wall Side Effects: o Nausea and Vomiting (vest) Patient Education: o Avoid snacks 1 hour before – 2 hours after ▪ This helps prevent GI side effects o Have the child watch a movie or TV show / read a story during PT o Give bronchodilators before or during to increase secretion mobilization Fundamentals 27 o Perform chest PT at least twice a day, or more if necessary Chest Tubes • • • • • Action: reestablishes negative pressure and facilitates lung expansion Insertion: o Have client raise arm above the head on the affected sign Indications: o Pneumothorax (re-expand lung) o Following Procedures ▪ Draining Fluid / Blood / Air Expected Drainage After Surgery: o Expect 50 – 500 mL in the first 24 hours ▪ Blood will start bright red, then turn pink, and lastly a serous yellow over the course of a few days o Report more than 100 mL/hr of bright red blood to the doctor ▪ > 3 mL/kg/hr for 3 consecutive ours OR > 5-10 mL/kg in 1 hour ▪ Look for changes in vital signs that could indicate bleeding / hemorrhage ▪ Client may require a return to surgery or a transfusion of blood products Complications: o Air Leak ▪ Manifestations: • Continuous bubbling in the water seal chamber ▪ Nursing Interventions: • Start at chest tube and move down tubing to locate leak • Tighten connection or replace drainage system o Keep connection taped securely o No Tidaling in Water Seal Chamber: ▪ Nursing Interventions: • Check for kinks in the tubing • Check for breath sounds (are the lungs re-expanded?) o No Bubbling in Suction Control Chamber: ▪ Nursing Interventions: • Verify that tubing is attached • Verify that water is filled to the prescribed level • Check the wall suction regulator o Chest Tube Disconnected from System: ▪ Nursing Interventions: Fundamentals 28 • Insert open end of the chest tube into sterile water until the system can be replaced o Chest Tube Dislodgement (Pulled Out of Patient) ▪ Manifestations: • Air leaking is audible ▪ Nursing Interventions: • Priority = Firmly Cover Insertion Site w/ Palm of Gloved Hand • Apply sterile occlusive dressing taped on three sides o Example: Petroleum Jelly Dressing o Taping 4 sides would risk pneumothorax • Call HCP and anticipate insertion of new chest tube • Stay with client to assess lung sounds and monitor vital signs Colonoscopy • Pre-Procedure Education: o Day Before = Clear Liquid Diet ▪ Bowel Cleaning Agent (Polyethylene Glycol or Cathartic Enema) o NPO 8-12 hours before o Antibiotics are NOT required prophylactically in healthy patients Colostomy Care • • Nursing Care: o Monitor the ostomy site and output ▪ Dusky, Pale, or Purple Stoma = Lack of Perfusion ▪ We want the stoma to be a shiny red / pink o Monitor for Complications ▪ Fluid / Electrolyte Imbalances, Ischemia of Ostomy, Bleeding, Infection, Peristomal Skin Irritation o Emotional Support / Support Group o Clarify enteric coated medications (may not properly be absorbed Patient Education: o The colostomy should begin to function in 2 to 4 days o Empty the bag when ¼ to ½ full (best practice is 1/3) o Change the appliance bag every 5-10 days o Avoid foods that are hard to digest or have a peel / husk ▪ Nuts, Popcorn, Celery, Seeds, Coconut o Avoid High Fiber Foods in Immediate Post-Op Period: ▪ Brown Rice ▪ Multigrain Bread Fundamentals 29 o o o o o o o o o Increase Fluid Intake Avoid moisturizing soaps because it makes it hard for the bag to stick Use stoma powder for raw skin Clip the hair around the stoma before bag placement Reintroduce foods one at a time Use the knee-to-chest position for abdominal cramping Burp the Bag Chew Foods Well Do NOT put aspirin in the pouch ▪ Can result in stoma ulceration o Controlling Odor / Gas ▪ Avoid Gas Producing Foods: • Broccoli, Cauliflower, Brussel Sprouts, Asparagus • Fish and Eggs • Garlic • Beans • Onions • Chewing Gum ▪ Eat More Gas Prevention Foods: • Cranberry Juice • Yogurt • Crackers • Toast Continuous Bladder Irrigation (CBI) • • • Definition: A 3-way catheter is used to continuously infuse the solution by gravity o Rate is determined by how much is needed to keep the catheter patent Indications: o Prescribed following surgical transurethral resection of the prostate ▪ Prevents the obstruction of urine flow by blood clots Expected Results: o Light-Pink Drainage w/ Few Clots Crutches • Measuring: o Begin measurement 3 fingers (1-1.5 inches) down from axillary fold to a point lateral and in front of the foot (tripod position) o Have hand bar around top-of-hip level, where elbows flexed at 30 degrees o Fundamentals • • • • • Proper Use: o The person should NOT rest their weight on their axillae ▪ Hand and wrist weakness means the client is using it wrong Stairs: o Hold railing with one hand and crutches with other (push down on both) o Up with the GOOD, down with the BAD ▪ The crutches always move with the affected (bad) leg Gaits: o Two Point Gait: ▪ Right Crutch and Left Foot AT SAME TIME ▪ Left Crutch and Right Foots AT SAME TIME ▪ Used with both feet partial weight bearing • This is used for milder, less advanced bilateral weakness ▪ This most resembles normal walking and requires weight on both legs ▪ (Even Number of Legs – Kind of Weak) o Three Point Gait: ▪ Both Crutches and Affected (in air) at Same Time • Then the unaffected foot advances ▪ Good for non-weight bearing on one affected leg • The non-affected leg bears weight ▪ (Odd Number of Legs Affected) o Four Point Gait: ▪ Right Crutch, THEN Left Foot ▪ Left Crutch, THEN Right Foot ▪ Used with both feet partial weight bearing • This is for more severe, advanced bilateral weakness ▪ (Even Number of Legs – Very Weak) Sitting with Crutches o Back up to the chair o Both crutches held on bad side o Hold armrest on good side o Lower themselves using both supports Standing Up with Crutches o Both crutches held on bad side o Move to edge of chair o Hold armrest on good side o Rise with support of good leg, armrest, and crutches 30 Fundamentals 31 Constipation • • Prevention: o Drink at least 1.5 L of water a day (2 - 3 L preferred) o Consume whole grains and coarse fibers, rather than refined grains o Increase consumption of raw fruits and vegetables o Exercise to improve peristalsis Management: o Avoid laxative use since they hinder natural defecation habits o Sit on the toilet for 30 minutes after meals CT Scan • Nursing Considerations: o Discontinue Metformin 24-48 hours before IV contrast ▪ Restart after 48 hours when stable renal function is confirmed Cushing’s Triad • • Indicators of Increased ICP o Bradycardia o Increased SBP / Widened Blood Pressure o Slowed, Irregular Respirations (Cheyenne-Strokes) These are late signs of increased ICP that indicate brain stem compression Delirium • • Signs of Delirium: o Reduced LOC o Sudden Memory Impairment o Illogical Thinking o Sleep Disturbances How is it Different from Dementia? o Sudden in Onset o An anti-anxiety med can help delirium, but not dementia Dialysis • • Goal = remove waste from client’s blood o Maintains safe concentration of electrolytes o Corrects acidosis o Removes excess fluid Hemodialysis: cleansing of the blood in ESRD or acutely ill clients o Nursing Interventions: ▪ Weight client before and after the procedure Fundamentals 32 ▪ ▪ ▪ • Hold regular morning medications until procedure is complete Continuously monitor BP Assess for presence of thrill and bruit (ensures fistula is good) • No BP readings or venipuncture on affected arm ▪ Maintain fluid restrictions ▪ Monitor the fistula for signs of distal extremity ischemia • Pale Skin • Pain • Numbness and Tingling • Diminished Pulses • Poor Capillary Refill ▪ Encourage hand exercises after the placement of a fistula • This promotes fistula maturation • Surgical site pain is OK, pain below it is not ▪ Edema of the AVF arm is OK unless it goes on for more than 2 weeks Peritoneal Dialysis: o Procedure: ▪ Warm the dialysate ▪ Allow it to flow in by gravity ▪ 5 – 10 minutes in, stays in for 30 minutes, 10 – 20 minutes of drainage • Drainage should be clear or pale yellow ▪ Monitor for Complications • Peritonitis • Bleeding • Respiratory Difficulty • Abdominal Pain • Bladder or Bowel Perforation ▪ If dialysate doesn’t flow out, position client on their side • The majority of what was put in should come out o Nursing Interventions: ▪ Have client void before the procedure ▪ Weigh the client daily ▪ Maintain asepsis ▪ Monitor vital signs throughout procedure and following ▪ Requires sterile dressing changes regularly ▪ Keep and accurate record of the client’s fluid balance ▪ Report any cloudy / opaque effluent drainage Fundamentals 33 • This could indicate a developing peritonitis EEG Procedure (Brain) • Patient Education: o Hold Certain Medications Prior to Procedure ▪ Depressants, Stimulants, Antiseizure Medications o Avoid Caffeine 8 Hours Prior o Have Client Wash Hair Before Procedure ▪ Must be free of oils, sprays, and conditioners Emergency Care • Order of Emergency Assessment: o Airway ▪ Clear Airway ▪ Stabilize Cervical Spine o Breathing ▪ Give Oxygen ▪ Prepare to Intubate o Circulation ▪ Check Pulse & Heart Rate ▪ Control Bleeding o Disability ▪ Check LOC ▪ Assess Using Glasgow Coma Scale o Exposure ▪ Remove Clothing ▪ Prevent Heat Loss o Full Set of Vital Signs + Focused Interventions ▪ Monitor ECG ▪ Place Tubes and Drains o Give Comfort ▪ Assess and Treat Pain o Head to Toe Assessment + History (SAMPLE) ▪ Signs and Symptoms ▪ Allergies ▪ Medications ▪ Past Medical History ▪ Last Meal ▪ Events Preceding Fundamentals 34 o Inspect Posterior ▪ Logroll and Palpate Endotracheal Suctioning • • • Indications for Suctioning: o Restlessness, Tachypnea, Tachycardia, Decreased O2 Sat, Adventitious Breath Sounds, Visualization of Secretions, Absence of Spontaneous Cough Procedure: o Semi or High Fowler’s Position o Obtain baseline vitals o Pre-oxygenate o Surgical Aseptic Technique o Do NOT suction on the way in o Suctioning 10-15 seconds per pass in rotating motion o Limit suctioning to 2 – 3 attempts o Allow recovery time between attempts (20 – 30 seconds in between passes) o Document secretion characteristics and client response Nursing Considerations: o NEVER suction routinely, only when indicated Enemas • • • Nursing Care: o Cramping ▪ If cramping occurs, stop the infusion with the roller until pain subsides ▪ After cramping subsides, resume at a slower rate Procedure for Cleansing Enema: o Assist the client into the left lateral position with right knee flexed (Sims) o Hang the enema bag no more than 12 inches above the rectum ▪ Make sure the enema is room temperature or warmed • Put the solution in a basin of hot water ▪ Cold enemas cause abdominal cramping o Insert the tube with the tip directed towards the umbilicus ▪ Use lubrication and only insert 3 - 4 inches o Encourage the client to retain the enema for as long as possible Barium Enema: o Purpose: to visualize the colon for diagnosis o Contraindications: ▪ Acute Diverticulitis (Could Rupture and Cause Peritonitis) o Patient Education: Fundamentals 35 ▪ Clear Liquid Diet Day before test ▪ NPO 8 hours before o Nursing Considerations: ▪ Chalky, White Stool is Normal • Laxatives and fluids help expel the barium Enteral Feedings • Nursing Interventions: o Assess gastric pH before each feeding (every 4 hours for continuous) ▪ Should be < or equal to 5 o Assess for symptoms of intolerance every 4 hours ▪ Abdominal Distention, Nausea and Vomiting o Assess bowel function before each feed ▪ Bowel Sounds o Assess residual before each feed (every 4 hours for continuous) ▪ Refeed the residual UNLESS it is more than 100 mL • This poses a risk of aspiration • Stop Feed / Hold Feed and Call HCP • Metoclopramide may be prescribed ( gastric emptying) o Maintain Semi-Fowler’s while feeding is infusing (> 30 degrees) ▪ Keep the bed up for 30-60 minutes after the feeding ▪ Hold feeding if the client must be supine o Flush the tube before and after feedings / medications o Change the bag and tubing every 24 hours • The Intubated Client: o Keep tube inflated at appropriate pressure ▪ Low cuff pressure puts client at risk of aspirations ▪ Only awake clients feeding themselves can lower cuff pressure o Use caution when administering sedatives ▪ Over sedation delays gastric emptying and reduces the gag reflex o Avoid bolus feedings ▪ This client is already at high risk of aspiration • Complications & Treatments: o Nausea, Vomiting, Diarrhea ▪ Can occur with hypertonic formulas or too fast of a feed ▪ Slow the rate of administration o Electrolyte Imbalances ▪ Hyponatremia and Hyperkalemia are common Fundamentals 36 o Tube Misplacement / Dislodgement ▪ Immediately remove any tube that may be dislodged or misplaced o Bleeding and Infection o Dehydration Fall Precautions • • • • • Risk Factors: o Old Age o Impaired Mobility o Cognitive / Sensory Impairment o Bowel / Bladder Dysfunction o Adverse Effects of Medications o History of Falls Environmental Changes: o Keep the floor free of clutter with clear path to the bathroom o Remove area rugs or secure with double sided tape o Provide adequate lighting (nightlights to get to the bathroom) o Clean up any puddles o Use grab bars and non-skid mats in the bathroom o Never walk around in just normal socks, need non-skid slippers Nursing Interventions: o Complete a fall assessment on admission o Assign clients at risk of falls close to the nursing station o Provide the client with non-skid footwear o Orient the client to the room and how to locate / use all necessary items ▪ Ex. Call Bells, Grab Bars, etc. o Maintain the lowest possible bed position o Instruct a client who is unsteady to use the call bell when they need the toilet o Answer call lights promptly to stop clients from getting up on their own o Determine the client’s ability to use assistive devices and keep them nearby o Use bed alarms and chair sensors to prevent at risk clients from getting up alone o Lock wheels on beds, wheelchairs, and gurneys o Round hourly to decrease call-light use and falls Patient Education: o Exercise regularly to increase strength, balance, and coordination o Get regular vision exams Helping the Client Fall: o Put out foot and let them slide down your leg Fundamentals 37 Fire Safety • • RACE o o o o PASS o o o o Rescue Patients Activate Alarm Contain the Fire Extinguish Pull Out Pin Aim at Base of Fire Squeeze the Nozzle Sweep Back and Forth Fluid Volume Deficit vs Fluid Volume Excess • • Fluid Volume Deficit (FVD) o Weight o Pulse (weak and thready) o Blood Pressure o Urine Output o Level of Consciousness o Neurological Changes Fluid Volume Excess (FVE) o Weight o Edema o Blood Pressure o Pulse (bounding) o Urine Output o Level of Consciousness (due to hyponatremia) o Moist Crackles and Dyspnea o Jugular Vein Distension (JVD) Foley Catheter • Insertion: o Cleansing: ▪ Use nondominant hand to spread the labia ▪ Wipe Order = 1. Labia Majora 2. Labia Minora 3. Urinary Meatus • Clean from front to back and out to in o Advancing Catheter: ▪ Insert to catheter until urine is observed, then another 1 – 2 inches Fundamentals 38 ▪ ▪ • • • For males, the catheter is inserted until it reaches the bifurcation If the catheter is inserted into the vagina, leave it in place to mark the whole until the catheter is correctly inserted Maintenance: o Measure client’s output every shift o Provide meticulous perineal care with soap and water (not antimicrobials) ▪ Each shift and after bowel movements o Keep drainage bag below the level of the client’s bladder ▪ Also prevent dependent loops and kinking in the tubing o Increase daily fluid intake o Decrease as soon as possible due to increased risk for UTI In Case of Obstruction o Assess for mechanical obstruction when there is leaking ▪ Remove kinking or compression of the catheter ▪ Milk to tube to dislodge a visible obstruction o Notify HCP if these methods are failed ▪ We try to avoid irrigation since infectious material can be washed back into the bladder Withdrawing a Specimen: o Scrub the collection port with alcohol for 15 seconds before withdrawing o Never take a specimen from the collection bag o Clamp the tubing below the collection port when taking a specimen Glasgow Coma Scale Eye Opening Verbal Response Motor Response 4 – Spontaneous (open with blinking at baseline) 3 – Open to Speech 2 – Open to Pain Only 1 – None 5 – Oriented 4 – Confused (converses but is disoriented) 3 – Inappropriate Words 2 – Incomprehensible 1 – None 6 – Obeys Commands for Movement 5 – Localizes to Pain 4 – Withdraws from Pain 3 – Flexion in Response to Pain (decorticate posturing) 2 – Extension in Response to Pain (decerebrate posturing) Fundamentals Interpretation 39 1 – None • Range: 3-15 • Coma: no eye opening, does not follow commands, and doesn’t utter understandable words (3-8) • Mild = 13-15, not a priority concern Glycemic Agents • • • • • Action: Promotes breakdown of glycogen in the liver, resulting in increased blood sugar Indications: Emergency treatment of severe hypoglycemia Example: Glucagon Side Effects: o Nausea and Vomiting o Rebound Hypoglycemia Nursing Considerations: o This is for use in unresponsive, hypoglycemic clients o Provide carbohydrates once the client awakens Heart Auscultation Ileostomy Care • Same as Colostomy Except: o Ileostomy produces liquid stool since it doesn’t go through the colon Fundamentals • 40 Immediate Post-Op Period Diet: o LOW RESIDUE! ▪ After the ileostomy is healed, the client can reintroduce fibrous foods one at a time o Low Fiber / Residue Carbohydrates are OK: ▪ White Rice, Refined Grains, Pasts Injections • Safest IM Injection Site in Adults = Ventrogluteal (lots of muscles, few nerves) Incident Reports • Do NOT document that an incident report was filed or refer to it in the EMR Increased ICP • Causes: o Head injury with bleeding o Stroke Fundamentals • • • • 41 o Brain tumor o Hydrocephalus o Ruptured Aneurysm or Subarachnoid Hemorrhage o Meningitis or Encephalitis Manifestations: o Earlies Signs: ▪ Changes in LOC • Restlessness, Confusion, Drowsiness, Lethargy, Stupor o Subsequent Signs ▪ Headache and Irritability ▪ Nausea and Vomiting (often projectile) ▪ Pupil Changes ▪ Beck’s Triad (hypertension + widened PP, bradycardia, irregular RR) ▪ Ineffective thermoregulation Contraindications: o Opioids and Sedative Use (makes it hard to do neurological assessment) o Flat HOB Treatment: o Treat the cause o Medications: ▪ Barbiturates – put client into coma with ventilator support ▪ Acetaminophen – fever ▪ Mannitol – decreases cerebral edema ▪ Steroids – decreases cerebral edema (dexamethasone) o Hypothermia may be used Nursing Interventions: o Monitor vital signs and neurological function o Keep HOB 30 to 45 degrees ▪ Keep head in a neutral position to enhance drainage o Avoid things that further increase ICP ▪ Coughing, sneezing, straining, suctioning o Maintain adequate respiratory exchange o Monitor I & O’s ▪ May restrict fluid to decrease cerebral edema o Decrease environmental stimuli Insulin Fundamentals • • • • Rapid-Acting Insulin: o Examples: ▪ Aspart ▪ Lispro ▪ Glulisine o Onset: 15 – 30 minutes Peak: 0.5 - 2.5 hours Duration: 3-6 hours o Nursing Considerations: ▪ This is given right before meals Regular Insulin o Onset: 0.5 – 1 hour Peak: 1-5 hours Duration: 6-10 hours o Nursing Considerations: ▪ This is given right before meals ▪ Only insulin that can be given IV Intermediate Insulin: o Onset: 1 – 2 hours Peak: 6 – 14 hours Duration: 16 – 24 hours o Examples: ▪ NPH (cloudy insulin) o Nursing Considerations: ▪ Given twice daily ▪ Have a bedside snack of a protein and a complex carb to prevent nighttime hypoglycemia Basal Long-Acting o Examples: ▪ Glargine ▪ Detemir ▪ Degludec o Onset: 1 hour Peak: NONE Duration: 24 hours o Nursing Considerations: 42 Fundamentals • • 43 ▪ Give once daily at bedtime Mixing Regular and NPH Insulin o Mnemonic: Nancy Raegan RN ▪ Inject air into NPH and then Regular ▪ Draw up Regular and then NPH ▪ Overdraw of NPH = Waste Whole Syringe ▪ Don’t want to contaminate clear with cloudy Insulin Teaching: o Roll insulin, don’t shake it o Rotate injection sites o Educate about diet, exercise, and glucose monitoring IV Insertion and IV Care • • Insertion: o Choose an unaffected arm (no mastectomy) o Insert the catheter at the most distal site as possible o Involves use of clean gloves o Use non-porous tape for the elderly Maintenance: o Do NOT change IV sites more frequently than 72-96 hours unless complications o Flush saline locks every 8-12 hours to maintain patency o Change IV tubing every 72 hours (unless TPN) IV Complications • • Infection: o Manifestations: ▪ Redness ▪ Drainage ▪ Edema ▪ Discomfort ▪ Warmth / Coolness ▪ Hardness o Nursing Interventions: ▪ Removal and Antibiotics Infiltration: o Definition: a complication that occurs when solution infuses into the surrounding tissues of the infusion site o Cause: ▪ A dislodged IV catheter Fundamentals • • • o Manifestations: ▪ Pallor ▪ Coolness ▪ Edema o Nursing Interventions: ▪ Discontinue the IV immediately and switch arms for site ▪ Elevate the arm to alleviate swelling ▪ Apply a cold compress ▪ Notify HCP if any other complications develop (cellulitis, necrosis, etc.) Extravasation: o Definition: infiltration of a drug into the tissue surrounding the vein ▪ Some drugs can cause skin breakdown or necrosis in the tissue o Manifestations: ▪ Pain ▪ Blanching ▪ Swelling ▪ Redness o Nursing Interventions: ▪ Stop the infusion and disconnect IV tubing ▪ Use a syringe to aspirate the drug from the IV catheter ▪ Remove the IV catheter after aspirating ▪ Elevate the extremity to reduce edema ▪ Apply a cold compress ▪ Notify HCP and obtain any antidote ▪ Do NOT flush since more drugs will be pushed in ▪ Any subsequent IV should be placed on the unaffected arm ▪ Avoid heat with drugs that can cause tissue necrosis Catheter Embolus: o Nursing Interventions: ▪ Apply a tourniquet ▪ Do NOT reinsert stylet into catheter Phlebitis o Definition: inflammation of the vein ▪ Can lead to thrombophlebitis, emboli, or a bloodstream infection o Causes: ▪ Irritating Drugs • Vancomycin ▪ Catheter Movement 44 Fundamentals 45 • Inadequate Stabilization ▪ Bacteria • Poor Aseptic Technique o Manifestations: ▪ Erythema (along the vein) ▪ Edema ▪ Warmth ▪ Pain ▪ Palpable Venous Cord o Nursing Interventions: ▪ Remove catheter immediately ▪ Apply a warm compress IV Solutions • • Isotonic Solutions o Examples: ▪ 0.9% NS ▪ Lactated Ringer (LR) ▪ 5% Dextrose in Water o Characteristics: ▪ Same concentration as plasma and extracellular fluid o Give to These Patients: ▪ Blood Loss ▪ Dehydration (Vomiting and Diarrhea) ▪ Surgery Hypotonic Crystalloid Solutions: o Examples: ▪ 0.45% NaCl ▪ 2.5% Dextrose in Water o Characteristics: ▪ Solution less concentrated than extracellular fluid ▪ Body fluid moves out of vascular system and into tissues • Depletes circulatory fluid ▪ Can cause cell lysis o Give to These Patients: ▪ Patients that need to hydrate the cell • DKA and Hyperosmolar Hyperglycemia o AVOID: ▪ Patients with increased ICP – will cause further cerebral edema Fundamentals • 46 ▪ Burns and Trauma – they need more fluid in the vascular system! Hypertonic Solutions: o Examples: ▪ 3% Saline and 5% Saline ▪ 10% Dextrose in Water ▪ 5% Dextrose in 0.9% NaCl or 0.45% NaCL ▪ 5% Dextrose in LR ▪ Colloid Solutions • Dextran • Albumin o Characteristics: ▪ Higher concentration than extracellular fluid ▪ Body fluids move from the cells into the vascular system ▪ Causes cells to shrink and fluid to move into vascular system o Give to These Patients: ▪ Hyponatremia – pulls sodium back into the intravascular spaces ▪ Cerebral Edema – decreases brain swelling o Nursing Considerations: ▪ Given via a central line since it can cause phlebitis ▪ Risk of fluid overload and pulmonary edema Lab Specimen Collection • Sputum Collection o Collect sputum in the morning since secretions accumulate overnight o Assume upright position o Rinse your mouth out with water beforehand o Do NOT touch the inside of the specimen cup o Inhale a few times and then cough forcefully Liver Biopsy • • Procedure: o Lay supine for procedure Post-Op Care: o Lay on right side for 2 hours following the procedure (puts pressure on liver) ▪ Then lie for supine for another 12 hours o Monitor for s/s of hemorrhage ▪ Tachycardia, Hypotension, Pallor Lobe Functions • Parietal: Fundamentals • • • o Function: ▪ Sensation o Injury Causes: ▪ Impaired Sensation Frontal Lobe: o Function: ▪ Higher Order Processing ▪ Executive Function and Personality o Injury Causes: ▪ Behavioral Changes Temporal Lobe: o Function: ▪ Integration of Visual and Auditory Input o Injury Causes: ▪ Inability to Understand Verbal or Written Language Occipital Lobe o Function: ▪ Registers Visual Images o Injury Causes: ▪ Vision Deficits Lumbar Puncture • • • Pre-procedure: o Empty bladder o Increased ICP = Contraindication Procedure: o Lie side lying with head, back, and knees flexed (fetal position) o Can also sit and lean forward o Patient may feel pain radiating down the leg temporarily o Put bandage over the site when completed Post-Procedure: o Lie supine???? with no pillows after the procedure to prevent a headache o Watch for leaking fluid which would require a blood patch to stop Lung Sounds • Normal Breath Sounds: o Bronchial: only heard anteriorly over tracheal area ▪ High pitched and loud ▪ Shorter inspiration than expiration 47 Fundamentals • 48 o Bronchovesicular: heard anteriorly and posteriorly ▪ 1st and 2nd ICS and between scapulae ▪ Medium pitched with equal inspiration + expiration ▪ Equal expiration and inspiration o Vesicular: heard anteriorly and posteriorly in peripheral lung fields ▪ Low pitch ▪ Shorter expiration than inspiration Abnormal Breath Sounds: o Coarse Crackles: ▪ Low pitched, wet bubbling ▪ Mainly heard on inspiration ▪ Causes = fluid in the lungs due to HF, pneumonia, pulmonary edema o Fine Crackles: ▪ High pitched, crackling sounds • Almost sounds like a fire ▪ Mainly heard on inspiration ▪ Doesn’t clear with coughs o High Pitched Wheeze: ▪ Musical in nature ▪ A lot of different sounds ▪ Usually heard in expiration ▪ Causes = Asthma, COPD o Low Pitched Wheeze: ▪ Sounds like a low-pitched whistle ▪ Made up of one sound quality ▪ Usually heard in expiration ▪ Causes = Asthma, COPD o Stridor: ▪ High pitched whistle ▪ Heard on inspiration ▪ Causes = Airway Obstruction, Croup, Epiglottitis ▪ This is an emergency o Pleural Friction Rub: ▪ Rubbing together due to inflammation ▪ Heard on inspiration and expiration ▪ Have the client hold their breath to tell difference between heart + lungs Mechanical Ventilation • Definition: provides respiratory support during surgery, respiratory distress / failure Fundamentals • • • 49 Nursing Care: o Ensure advanced airway is secured o Assess position of tube and length of exposed tube o Wrist restraints may be required to prevent accidental intubation o Suction oral and tracheal secretions as indicated (not on a schedule) o Assess respiratory status ever 1 to 2 hours (there should be BS in both lungs) o Monitor ventilator settings and alarms ▪ Never just silence alarm o If client’s respiratory status declines, manually ventilate with a bag o Maintain Medications as Prescribed ▪ Analgesics, Sedations, and Neuromuscular Blocking Agents o Reposition ET tube every 24 hours to prevent break down o Drop in O2 = Auscultate Lungs (ensure tube is in place) Ventilator Settings o TOO HIGH = Respiratory Alkalosis ▪ Overventilation = Over pH o TOO LOW = Respiratory Acidosis ▪ Underventilation = Under pH ▪ Don’t take this patient off ventilation Alarms and Meaning: o High Pressure Alarm: indicates increase pressure, something is blocking the tube ▪ Causes: • Increased Secretions o Turn, Cough, Deep Breathe o Suction if this does not work • Kinking of Tubing o Unkink the tube • Pulmonary Edema o Diuretics • Client Coughing or Biting the Tube • Water Condensation o Empty ▪ Order of Intervention: • Always check the system first o 1. Unkink o 2. Empty any collected water • Then Turn, Cough, Deep Breathe (TCBD) • Suction is last resort Fundamentals • 50 o Low Pressure Alarm: indicates decreases pressure ▪ Causes: • Cuff Leak • Tube Disconnection o Main Tubing or O2 Sensor o Solve by reconnecting • Tube Dislodgement o Mechanical Ventilation (until reinsertion) o Apnea Alarm: no spontaneous breath within a preset time Preventing Ventilator Associated Complications o Pneumonia: ▪ Hand Hygiene ▪ Oral Hygiene • Chlorhexidine Followed by Suctioning ▪ Maintain Closed System ▪ Maintain Semi Fowler’s (30 – 45 degrees) o Pneumothorax: ▪ Caused by high ventilation pressures • Auscultate Lung Sounds Frequently • Monitor for Sudden Respiratory Distress ▪ Requires immediate chest tube insertion o Sedation and Weaning: ▪ Monitor client’s level of sedation ▪ Use the minimum amount of sedation needed for comfort ▪ Perform daily sedation vacations to determine readiness for weaning o GI Complications: ▪ Initiate Enteral Feedings (High Calorie + High Protein) ▪ Monitor Gastric Residuals (Prevent Aspiration) Nasogastric Tube Insertion and Maintenance • Insertion Procedure: o Measure from the tip of the nose to the earlobe, then the xiphoid process ▪ Mark this with tape o Lubricate the tip and insert into a clear nostril o Once the tube gets past the nasopharynx, have the client flex their head forward ▪ Swallow small sips of water o If the client begins to cough and gag, pull back the tube slightly ▪ Give the client time to breath, and then begin again Fundamentals • • • 51 o Advance the tube to the marked point o Very tube placement initially with x-ray ▪ Once it is verified, anchor it in place with tape ▪ Watch the tube to make sure it isn’t pulled out Tube Maintenance: o Replace the tube every 4 weeks o Routinely assess the length of exposed tubing Suction Following GI Surgery: o Bright red bloody drainage is a red flag (medical emergency) ▪ Drainage should be yellow/green in color or clear Nursing Considerations: o Monitor Skin Integrity ▪ Risk of nose breakdown Ophthalmic Medication Administration • Steps to Administer Eye Drops: 1. Remove Dried Secretions a. Moistened sterile gauze pads b. Wipe from inner to outer canthus 2. Place Client in Supine / Sitting Position a. Head tilted back toward the side of the affected eyes 3. Rest Hand on Client's Forehead a. Hold dropper 1-2 cm above conjunctival sac b. This avoids contamination 4. Pull Lower Eyelid Down Gently a. Use thumb or forefinger against the bony orbit 5. Instruct Client to Look Upward a. Minimizes blink reflex b. Retracts the cornea up 6. Instruct Client to Close the Eyelid a. Move around the eye if able 7. Apply Pressure to Lacrimal Duct If Medication Has Systemic Effects a. For 30-60 seconds b. Distributes medication and prevents overflow into the lacrimal duct c. Reduces possible systemic absorption 8. Remove Excess Medication from Each Eye a. Use a new tissue or gauze pad to prevent cross contamination 9. Additional Ophthalmic Medication a. Wait 5 minutes if putting a different medication into the same time Fundamentals 52 Oral Hypoglycemics • • • Indications: used in combination with diet and exercise to control glucose levels in clients with Type II Diabetes o Teach these clients about signs of hypoglycemia ( < 70 mg/dL) ▪ Sweating, Pallor, Irritability, Tremors + Weakness, Shakiness, Tachycardia, Drowsiness, Fatigue, Headache, Difficulty Thinking, and Hunger ▪ Nursing Intervention: • Give 15 g of a simple carbohydrate o glucose tablets o 4 ounces of fruit juice o 6 to 10 hard candies o 2 to 3 teaspoons of sugar or honey • Give 15 g more in 15 minutes if blood sugar still low o Follow with 7 g of protein (cheese, crackers, etc) • Glucagon is given for unconscious clients Biguanides: o Action: reduces formation of glucose & makes cells more sensitive to insulin o Examples: ▪ Metformin o Nursing Considerations: ▪ Withhold for 48 hours prior to and 48 hours following CT with contrast Sulfonylureas: o Action: release of insulin from the pancreas o Examples: ▪ Glipizide ▪ Glyburide o Nursing Considerations: ▪ There is a high risk of hypoglycemia in clients with renal, hepatic, or adrenal disorders ▪ Can cause severe reaction when taken with alcohol Oral Mucositis • • • Cause: Chemotherapy Prevention: Palifermin Patient Education to Promote Comfort: o Clean the mouth with normal saline after meals and at bedtime o Use a soft-bristled toothbrush to decrease gum irritation o Application of prescribed viscous lidocaine HCl to alleviate oral pain Fundamentals 53 o Use of water-soluble lubricating agents to moisten mouth tissues o Avoid: ▪ Hot liquids and spicy / acid foods (cold is better) ▪ Antiseptic mouthwashes that irritate mucous membranes Oropharyngeal Airways (OPAs) • • Definition: temporary artificial airway for those who are sedated or unconscious Purpose: o Prevent Tongue Displacement Prevent Tracheal Obstruction o • Sizing: o Measure with flange next to client’s cheek o The OPA curve should reach the jaw angle • Insertion: o Insert with the distal end pointing up ▪ Towards the roof of the mouth o When the OPA reaches the soft palate, rotate the tip downwards ▪ Towards the esophagus • Nursing Considerations o DO NOT USE TAPE ▪ The client may independently expel the device when conscious, so make it easy to remove ▪ Coughing and gagging is a sign that it is time to remove the OPA Oxygen Safety • S Pain Relief • S Paracentesis • • • • Purpose: o Remove ascitic fluid from the peritoneal cavity due to cirrhosis Positioning: o High Fowler’s Patient Education: o Void before the procedure to avoid puncture of the bladder Nursing Considerations: o Monitor for signs of hypovolemia (treated with IV albumin) Fundamentals 54 ▪ Vital Signs monitored frequently for the first 4 hours Percutaneous Coronary Intervention (PIC) • • • Indications: o Stent Placement Procedure: o Anti-thrombolytics will be used for the procedure Complications: o Retroperitoneal Hemorrhage (Femoral) ▪ Hypotension ▪ Grey Turner Sign (Flank Ecchymosis) ▪ Back Pain ▪ Diminished Distal Pulses Phalen’s Maneuver • • Used to diagnose carpal tunnel Pain and numbness when pushing wrists down and together Postmortem Care • • Nursing Considerations: o Provide opportunity for family participation o Accommodate religious and cultural rituals Nursing Care: o Wash the body o Change linens and gowns o Place a pad under the perineum o Remove lines, tubes, and dressing o Replace dentures / leave them in place o Close the eyes o Place a pillow under the head o Fold a towel under the chin to close the mouth o Straighten the body and limbs Isolation Precautions • Contact: o Indications: ▪ Scabies ▪ Staph Infections • MRSA ▪ Multidrug Resistant Organisms Fundamentals 55 ▪ ▪ • Enterococcal Bacteremia C. Diff • Soap and Water ONLY Enteric Conditions Pressure Ulcer Prevention • • • Skin Care: o Barriers for Incontinence o Hydration o Remove Moisture Repositioning: o Pad Bony Prominences o Pad Medical Devices o Lift, Do NOT Pull (Risk of Sheer) o Limit Chair Time o Turn every 2-4 hours Nutrition: o Calorie Counting (30 – 35 kcal / kg / day) o Enteral Nutrition PRN o High Protein Fundamentals • 56 o Assess for Deficiencies Support Surfaces: o Alternate Pressure with Pillow Propping o AVOID Donut Devices and Synthetic Sheepskins o Heel Protection o Special Mattresses PPE Donning and Removal • Mark Klimek Rapid Response Criteria • • Activate the Rapid Response If: o There is an acute change in any of the following: ▪ Heart Rate < 40 or > 130 BPM ▪ SBP < 90 mmHg ▪ Respiratory Rate < 8 or > 28 / min ▪ O2 < 90% with oxygen ▪ Urine Output < 50 mL in 4 hours ▪ Severely Altered LOC Early Signs of Deterioration: o Dyspnea o Confusion o Restlessness Renal Biopsy • • Pre-Op Care: o NPO 4 – 8 hours prior to procedure o Preliminary Coagulation Labs (Risk of Bleeding) ▪ Platelets, PT Time, Anemia Testing Post-Op Care: o Patient on bed rest following the procedure for 2 to 24 hours ▪ Supine Position ▪ Back Roll for Support Restraints • • Preventing the Use of Restraints: o Implement distraction, frequent observation, etc. first Nursing Considerations: o Use the least-restrictive method possible o Never use restraints for convenience, punishment, etc. Fundamentals • • 57 Nursing Care: o Remove the restraints every 2 hours to assess the client o Assess neurovascular status every 2 hours o Leave restraints loose enough to prevent injury ▪ At least two finger widths between restraint and skin o Always tie the restraint to a moveable part of bed frame ▪ Not the immobile legs or the side rails o Use loose knots that are easily removed o Reassess need for continued use every 4 hours for up to 24 hours ▪ Must have a renewed prescription at this point Documentation: o Behaviors making the restraints necessary o Alternatives attempted and the client’s behavior while in restraints o Type and location of the restraints + time applied o Frequency and type of care ▪ ROM, Removal, Assessment of the Skin, Neurovascular Status) Romberg Sign • Definition: Component of the neurological exam to assess vestibular function, proprioception, and vision Fundamentals • Rule of Nines (Burns) 58 Fundamentals • 59 Total Area Burned = Sum of Percentages Parkland Formula 24-hr fluid requirement calculation 4 mL × body weight (kg) × total body surface area burned (% / decimal) First 8-hr fluid administration 50% total fluid requirement Remaining 16-hr fluid administration 50% total fluid requirement Fundamentals 60 Seizure Precautions • • • • • Nursing Interventions Before Seizures: o Bed Rest and Decreased Environmental Stimuli o Padded Side Rails o Ensure Immediate Access to Oxygen and Suction Equipment Nursing Intervention During and After Seizures: o Side Lying Position – maintain patent airway ▪ Assist the client to lay down if they were standing (protect the head) o Monitor Respiratory Status ▪ You may administer O2 during if the client becomes pale or cyanotic o Loosen Clothing o Do NOT Restrain Client o Do NOT put anything in their mouth o Document observations (before, during, and after the seizure) ▪ How long is the client unconscious? o Teach client to report auras o Monitor client in postcoital stage o Don’t put any kind of airway or suctioning in the mouth until after the seizure Patient Prevention Education: o Get adequate rest o Avoid alcohol o Wear a medical alert bracelet o Identify seizure triggers Medications to Stop Seizures: o Lorazepam and Diazepam o Phenytoin (given slowly) Anticonvulsants to Manage Seizures: o Phenytoin, Carbamazepine, Valproic Acid, Phenobarbital, Levetiracetam Scope of Practice Fundamentals • • 61 Other Considerations: o RNs must handle all unstable patients o RNs must deal with blood transfusions and IV medications Five Rights of Delegation: o Right Task: ▪ Within scope of practice ▪ Routine tasks with very little risk o Right Circumstances: ▪ Stable Client ▪ Adequate resources, supervision, and staffing o Right Person: ▪ Correct Patient ▪ Performer must have competency o Right Direction and Communication: ▪ Clear instructions with specific things to report back ▪ Ability to ask questions o Right Supervision: ▪ Monitor, evaluate, and intervene as needed ▪ Delegator is ultimately responsible for the task Shock (Early vs Late) • Signs of Early Shock: o Tachycardia (130 or less) o Normal BP (BP drops in late shock) o Pallor o Tachypnea Fundamentals • • 62 o Confusion Signs of Late Shock: o Hypotension o Weak, Thready Pulse o Anuria o Metabolic Acidosis (lack of perfusion to muscles) If given the BP, go off that Stool Characteristics • Appearance and Cause o Clay Colored Stool = Biliary Obstruction o Mucus / Pus Visible = Ulcerative Colitis or Infectious Colitis o Greasy, Fatty, Foul Smelling = Chronic Pancreatitis o Black Tarry = Upper GI Bleed o Bright Red and Blood = Lower GI Bleed o Blood on Stool’s Surface = Hemorrhoids Thoracentesis • • • Definition: removal of fluid from the pleural space to remove fluid for diagnosis Procedure: o Have client sitting and leaning forward over the bed side table o Use needle tom draw out fluid from the middle back Complications: o Pneumothorax TPN Administration • Nursing Considerations: o Must be administered through a central venous access point ▪ Also requires an infusion pump for exact dosage ▪ Follow the procedure of changing a central line dressing (q 48-72 hours) o Change tubing and bag every 24 hours o Monitor glucose q 6 hrs., electrolytes, and fluid balance o Prevent air embolism o Keep 10% dextrose in water available in case of loss of TPN o Weight the client daily and keep track of I&Os o Monitor for signs of hyperglycemia: ▪ Polydipsia ▪ Polyuria ▪ Headaches / Blurred Vision ▪ (Risk of seizures, coma, or death) Fundamentals 63 Tracheostomy Care • • • • Indications: o Provide tracheostomy care every 8 hours and as needed ▪ Change tracheostomy tubes as prescribed Nursing Considerations: o ALWAYS keep two extra tracheostomy tubes at the bedside ▪ This is in case of accidental decannulation ▪ One the clients size and one a size smaller (swelling) Procedure: 1. Gather supplies to the beside a. New Cannula b. Sterile, PRECUT Dressing (if you cut it, the client can aspirate fibers) c. Non-Sterile Gloves AND Sterile Gloves 2. Place Client in Semi-Fowler’s or Fowler’s Position 3. Don Appropriate PPE a. Mask b. Goggles c. Clean Gloves 4. Auscultate Lungs a. Suction secretions if necessary 5. Use CLEAN Gloves to Remove Soiled Dressing a. Then remove the gloves and dispose of them 6. Use STERILE Gloves for the Rest of the Procedure a. Prevents infection of the lower airway 7. Remove Old Cannula and Replace with a New One a. Stabilize back plate with nondominant hand and unclip the cannula with other b. Touch only the outer locking portion of the new cannula c. Insert and lock into place 8. Clean Around the Stoma a. Sterile Water / Saline 9. Dry Around the Stoma Well a. Prevents growth of microorganisms 10. Replace Sterile Gauze Pad Trach Ties: o When changing trach ties, have someone hold the trach in place o Replace one trach tie at a time Triage in Mass Casualties Fundamentals • • • • 64 Emergent: life-threatening with high probability of survival if immediate treatment o Shock, Compromised Airway, Unstable Wounds, Chest Trauma Urgent: serious injuries requiring treatment within 30 minutes – 2 hours o Open Fractures w/ Palpable Distal Pulses, Large Wounds Non-Urgent: injuries requiring treatment but can wait 2+ hours o Infections, Minor Burns, Closed Fractures Expectant: extensive injuries with poor prognosis regardless of treatment o Severe Neurological Trauma (Agonal Respirations) o Full Thickness Burns >60% of body surface o Pulselessness and Apnea Trousseau’s Sign • • This is a sign of hypocalcemia Spasm of the hand and wrist when the client wears an inflated BP cuff for 2-3 minutes Unliteral Weakness / Neglect • • Causes: o Stroke on the opposite side of the affected limbs o Clients ignore input from the affected side and only care for affected Patient Education: o Clothe the affected side first o Scan the environment to reduce the risk of injury o Patient should be approached from the unaffected side Urinary Assessment • • Order: o Empty Bladder o Inspect o Auscultate o Percussion o Palpation Purpose: o Prevent manipulation of bowels from interfering with sound Walker • Steps for Walking: o 1. Walker moves forward a foot o 2. Affected leg moves next o 3. Unaffected leg moves next Fundamentals 65