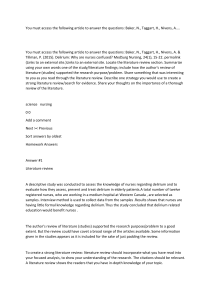
Heart & Lung xxx (2017) 1e5 Contents lists available at ScienceDirect Heart & Lung journal homepage: www.heartandlung.org Delirium prevention in critically ill adults through an automated reorientation intervention e A pilot randomized controlled trial Cindy L. Munro, PhD, NP, RN a, *, Paula Cairns, MSN, RN a, Ming Ji, PhD a, Karel Calero, MD b, W. McDowell Anderson, MD b, Zhan Liang, PhD, RN a a b University of South Florida College of Nursing, 12901 Bruce B. Downs Blvd, MDC 22, Tampa, FL 33612-4766, USA University of South Florida Morsani College of Medicine, 12901 Bruce B. Downs Blvd, MDC 19, Tampa, FL 33612-4766, USA a r t i c l e i n f o a b s t r a c t Article history: Received 26 October 2016 Received in revised form 4 May 2017 Accepted 5 May 2017 Available online xxx Objectives: Explore the effect of an automated reorientation intervention on ICU delirium in a prospective randomized controlled trial. Background: Delirium is common in ICU patients, and negatively affects outcomes. Few prevention strategies have been tested. Methods: Thirty ICU patients were randomized to 3 groups. Ten received hourly recorded messages in a family member’s voice during waking hours over 3 ICU days, 10 received the same messages in a nonfamily voice, and 10 (control) did not receive any automated reorientation messages. The primary outcome was delirium free days during the intervention period (evaluated by CAM-ICU). Groups were compared by Fisher’s Exact Test. Results: The family voice group had more delirium free days than the non-family voice group, and significantly more delirium free days (p ¼ 0.0437) than the control group. Conclusions: Reorientation through automated, scripted messages reduced incidence of delirium. Using identical scripted messages, family voice was more effective than non-family voice. Ó 2017 Elsevier Inc. All rights reserved. Keywords: Delirium Intensive care unit Family Delirium prevention Nursing care Critical illness Delirium intervention Introduction Delirium is an acute disturbance in attention and awareness, with additional change in cognition from the person’s baseline.1 Delirium develops over a short period of time and may fluctuate over the course of the day. Critically ill patients are at high risk for delirium, with 50% of ICU patients and as many as 80% of mechanically ventilated patients experiencing delirium.2 Metaanalyses indicate that patients with delirium have greater incidence of complications including nosocomial pneumonia, longer duration of mechanical ventilation, longer hospital length of stay, and higher hospital mortality than patients without delirium.3 Number of days of delirium has been identified as an independent predictor of mortality in ICU patients.4e6 Delirium in critical illness is estimated to cost $4 to $16 billion annually.2 Importantly, delirium in the ICU not only complicates the hospital course, but it is also associated with lasting sequelae.7e10 Data suggest that 25%e78% of patients who have delirium in the ICU suffer clinically significant declines in cognitive function * Corresponding author. E-mail address: cmunro2@health.usf.edu (C.L. Munro). 0147-9563/$ e see front matter Ó 2017 Elsevier Inc. All rights reserved. http://dx.doi.org/10.1016/j.hrtlng.2017.05.002 following their ICU stay.11,12 Cognitive dysfunction may persist for months or be permanent,9,11,13 and is associated with impairments in daily function.14 In recent studies, increasing duration of delirium was an independent predictor of worse cognition 3 months and 12 months after ICU discharge,11,13 and this remained true even after adjusting for risk factors such as age, severity of illness, severe sepsis, and exposure to sedative medications in the ICU.11 To date, the focus of delirium research has been on detection of existing delirium and on its pharmacologic treatment.15 Prevention of delirium using a non-pharmacologic intervention has not been well examined. Interventions that assist critically ill patients to integrate information more appropriately may decrease delirium and improve outcomes,16 but have not been rigorously tested. We reasoned that providing ongoing orientation to the ICU environment through recorded messages might enable the patient to more accurately interpret the environment and thus reduce risk of delirium, and that cuing patients only during daytime hours might also improve day/night orientation, further reducing risk of delirium. We developed a cognitive reorientation intervention which uses automated recorded audio messages, played at hourly intervals during daytime hours, to provide information about the ICU 2 C.L. Munro et al. / Heart & Lung xxx (2017) 1e5 Enrollment Assessed for eligibility (n = 40) Excluded: Did not meet criteria (n = 8) Unable to obtain consent (n = 2) Analysis Allocation Patient enrolled and randomized to group assignment (n = 30) Group 1 - intervention Unknown voice recorded reorientation message (n = 10) Group 2 - intervention Family member voice recorded reorientation message (n = 10) Group 3 - usual care No recorded reorientation message (n = 10) Received all episodes of intervention (n = 5) Received all episodes of intervention (n = 3) Received all episodes of usual care (n = 6) Did not receive full intervention: Early icu discharge (n = 4) Off the unit for testing (n = 1) Transferred to palliative care (n = 0) Death (n = 0) Did not receive full intervention: Early icu discharge (n = 6) Off the unit for testing (n = 0) Transferred to palliative care (n = 1) Death (n = 0) Did not receive full usual care: Early icu discharge (n = 3) Off the unit for testing (n = 0) Transferred to palliative care (n = 0) Death (n = 1) Analyzed (n = 10) Analyzed (n = 10) Analyzed (n = 10) Excluded from analysis (n = 0) Excluded from analysis (n = 0) Excluded from analysis (n = 0) Fig. 1. CONSORT study flow. environment to the patient. We thought that messages delivered in a voice familiar to the patient might result in greater attention to the messages and be comforting. This study tested the hypothesis that providing ongoing orientation to the ICU environment through recorded audio messages would reduce risk of delirium in critically ill adults; both familiar voices (family voice) and an unfamiliar voice (unknown voice) were tested against no recorded voice (control). Methods A three group, prospective, randomized controlled trial (RCT) design was used to examine the effects of the automated reorientation intervention on delirium. Ten subjects were randomized to receive automated reorientation messages in a family member’s voice (family voice group), ten subjects received the same messages in an unfamiliar voice (unknown voice group) and ten subjects (control group) did not receive any automated reorientation messages. The study CONSORT diagram is presented as Fig. 1. Human subjects protection The study was approved by the hospital where data were collected and by the Institutional Review Board of the university. Signed consent was obtained from subjects or their legally authorized representatives. Twelve subjects provided consent for themselves, and consent was obtained from legally authorized representatives for the 18 subjects who were unable to consent for themselves. Sample Subjects were eligible if they were over 18 years old and within 24 h of ICU admission. Exclusion criteria included anticipation by the clinical provider of imminent patient death, medical contraindication to the intervention (for example, psychiatric auditory hallucinations, or profound deafness), or inability to speak either English or Spanish. Subjects were recruited in 5 ICUs in a large urban level I trauma center in the Southeastern United States. A total of 30 subjects were randomized into 3 groups by the biostastician co-investigator (MJ) prior to the first enrollment using a computerized random number generator. Automated reorientation intervention Intervention development A draft script of reorientation messages was developed based on published research by our team and others about patients’ recall of ICU experiences.17e19 The script was refined based on reviews of 3 critical care experts, and further adjustments to message volume, length, and speaker location were made following input from healthy nurse volunteers in the ICU setting. The original script was developed in English; a Spanish version was translated from English by a certified medical translator and back-translated. Message description Each message was scripted, was no longer than 2 min long, included the subject’s name (preferred name as recommended by the subject’s family), and used simple terms at a 5th grade reading level. Other than the subject’s name, the recorded message was not specific to any patient condition, procedure, or family situation. Each message was delivered only during daytime hours (to provide general time orientation), stated that the message was recorded, and reoriented the subject frequently throughout the day to help them understand they were in the ICU. Additional message elements followed in random order, and provided information about the critical care environment, the visual and auditory stimuli to be expected, and the availability of providers and family. Random ordering of elements within the recorded message at each delivery was designed to reduce message repetition. The elements of the reorientation message are presented in Table 1. The script for messages was recorded by a family member of the family’s choice (for the family voice group) or by a bilingual female research staff person (for the unknown voice group). Selection of the English or Spanish script was based on the family’s decision regarding which language would be most meaningful to the subject. The messages were digitally recorded through a sound card and stored as a standard Microsoft wave file. Intervention delivery At predetermined time intervals over 3 days in the ICU (every hour for 8 h during the daytime hours, beginning at 9:00 am and ending at 4:00 p.m.), a recorded message was played back in the patient’s room through the room’s television audio system. The C.L. Munro et al. / Heart & Lung xxx (2017) 1e5 3 Table 1 Family voice reorientation message. The personalized introduction is delivered at the beginning of each message. The order of numbered sentences in the script below are randomly changed for each hourly message. Sentence #8 may be omitted if/when it becomes not applicable due to extubation. Personalized Introduction: Hello _______________________________, (insert name of patient) This is ________________________, your _______________________ , (insert your name and relationship to the patient). This is a recorded message to help you understand what is going on around you. 1) Do not be scared. 2) It is OK. 3) You are a patient at Tampa General Hospital. 4) Your nurses and doctors are here looking after you. 5) It is loud and noisy because of the machines helping you get better. 6) You have some wires and tubes in place to help you recover. 7) You may have something on your wrists to keep you from pulling at the wires and tubes by accident. 8) You can’t talk right now because of your breathing tube, but the nurses know you might be uncomfortable and are giving you medicine for that. 9) Please try to be calm and patient as the nurses and doctors work to get you feeling better. 10) All of our family know you’re here and we are in and out, looking after you too. timeframe chosen for intervention delivery coincided with usual waking hours, so as not to disturb sleep or interrupt family visits in the evening hours. Intervention began at the earliest available daytime hour following completion of family or staff recording. Subjects received a maximum of 24 recorded messages (8 messages per day for 3 days). Instances where the message was not delivered, for example when the subject was off the unit for procedures, were noted. The intervention ended if the subject was discharged from the ICU during the study period. The number of messages delivered was summed for each subject, and group means were calculated. Delirium The primary outcome for the study was delirium free days. Delirium was evaluated twice daily (prior to initiation of and following completion of the intervention administration) using the Confusion Assessment Method (CAM)emodified ICU version.20 For this research study, CAM-ICU determinations were made by the research nurse (PC) who is an experienced critical care RN trained in CAM-ICU administration. The CAM-ICU was developed for use by clinical providers who are not psychiatrists. Four features are evaluated as present or absent using standardized methods: 1) acute onset or fluctuating course, 2) inattention, 3) altered level of consciousness, and 4) disorganized thinking. A patient is assessed to have delirium only if features 1 and 2 are both present with either feature 3 or 4 also present. The CAM-ICU is recognized in the Society for Critical Care Medicine’s Clinical Practice Guidelines for the Management of Pain, Agitation, and Delirium in adult patients in the ICU settings as a valid, reliable, and feasible tool to detect delirium in ICU patients.2 A systematic review of 16 research studies involving 1523 participants using five screening tools concluded that the CAM-ICU was the most specific bedside tool for the assessment of delirium in critically ill patients, with pooled sensitivity of 75.5% and specificity of 95.8%.21 When CAM-ICU criteria for delirium were not met (negative result) for either of the assessments for a study day, and no clinical providers had documented intervening delirium, the day was counted as a delirium free day. Mean days of delirium, where at least one assessment indicated that CAM-ICU criteria were met (positive result) on the study day, were also calculated for each group. Sample characteristics In order to assess group equivalence and identify potential covariates, demographic data were collected, including sex, ethnicity, race, and age. In addition, baseline data about severity of illness and comorbidities were collected using the APACHE III scoring system, calculated on the most deranged values during the first 24 h of ICU admission. Analysis All enrolled subjects were analyzed. Descriptive statistics were produced to describe the 3 groups and to compare their characteristics (see Table 2). Groups were equivalent by ANOVA (including positive CAM-ICU at study admission and days in ICU) and no adjustments of covariates were needed. A Fisher’s Exact Test at Table 2 Sample characteristics. Variable Sex % (n) Male Female Ethnicity % (n) Hispanic Non-hispanic Race % (n) White Black Age in years, mean (SD) Positive CAM-ICU at study admission (n) APACHE score, mean (SD) Days on mechanical ventilation, mean (SD) Days in ICU, mean (SD) Total sample (30) Subjects by group Family voice Non-family voice Control 63.3 (19) 36.7 (11) 60 (6) 40 (4) 60 (6) 40 (4) 70 (7) 30 (3) 10 (3) 90 (27) 20 (2) 80 (8) 0 (0) 100 (10) 10 (1) 90 (9) 83.3 (25) 16.7 (5) 59.5 (17.0) 4 63.6 (20.7) 2.1 (5.5) 5.0 (5.9) 100 (10) 0 (0) 58.8 (14.2) 1 68.9 (12.4) 0.8 (0.8) 3.0 (1.6) 70 (7) 30 (3) 57.0 (12.1) 1 59.7 (23.8) 4.1 (9.0) 7.1 (9.4) 80 (8) 20 (2) 62.6 (23.9) 2 62.2 (24.7) 1.2 (2.7) 4.9 (3.5) 4 C.L. Munro et al. / Heart & Lung xxx (2017) 1e5 Table 3 Delirium assessments. Delirium free days, mean (SD) Mean days of delirium (SD) Family voice Unknown voice Control 1.9 (0.99) 0.3 (0.48) 1.6 (1.07) 0.6 (0.84) 1.6 (1.13) 0.9 (1.28) p < 0.05 for the number of delirium free days and the treatment assignment was performed to test the primary hypothesis. We did not make any adjustments for total duration of the intervention; not receiving the full 3 days of intervention attenuates the intervention effect, and we conservatively chose not to adjust in this small sample. Results Sample demographics and clinical characteristics The sample was 63% male, ranged in age from 19 to 92 years old (mean 59.5, SD 17.0), and had a mean APACHE severity of illness score of 64 (SD 20.7). Because we recruited from 5 ICUs (including Medical ICU, Cardiothoracic ICU, Vascular ICU, Surgical Trauma ICU, and Medical Respiratory ICU), there were a wide variety of admitting diagnoses; analysis was not performed for diagnosis or comorbidity subgroups. Eighteen of the 20 intervention subjects received messages in English, and 2 of the 20 intervention subjects received the messages in Spanish. Additional characteristics of the sample by group are presented in Table 2. Intervention delivery The mean number of messages delivered did not differ between the unknown voice group and the family voice group. The mean number of messages received by the unknown voice group was 20.3 (SD 6.25). The mean number of messages received by the family voice group was 19.8 (SD 5.16). Delirium free days and means days of delirium between groups During the three day intervention period, mean delirium free days were 1.9 in the family voice group, 1.6 in the unknown voice group and 1.6 in the control group (Table 3). Mean days of delirium were 0.3 in the family voice group, 0.6 in the unknown voice group, and 0.9 in the control group. To test the association between number of delirium free days and groups, we performed a contingency table analysis which yielded a Fisher’s Exact Test p value of 0.0437, indicating a significant difference among groups on number of delirium free days. Although the descriptive statistic of mean days of delirium showed a decreasing trend across the control, the unknown voice and family voice groups, the differences were not statistically significant. Discussion The major finding of our study was that patients in the family voice group had significantly more delirium free days than the control group. Mean delirium days were less in the family voice group than the unknown voice group or the control group, although the differences were not significant in this small sample. Our study is the first randomized controlled trial to examine the effects of using an automated reorientation intervention to prevent delirium among ICU patients. Delirium is a common manifestation of cognitive dysfunction in critically ill patients which is associated with substantial negative outcomes both during and following hospitalization. A recent meta-analysis concluded that compared to patients without delirium, patients with delirium were six times more likely to experience complications, had longer duration of mechanical ventilation, longer ICU length of stay, and longer hospital length of stay.3 Furthermore, patients who experience delirium have problems with cognitive function and health status after hospital discharge, which have been documented at 3 and 12 months and may persist indefinitely.13,22,23 Because of the extensive incidence and significant negative outcomes associated with delirium, identification of effective interventions to prevent or reduce delirium is critically important. The Society of Critical Care Medicine, in its most recent guidelines for managing pain, agitation, and delirium in the critically ill adult,2 recommended routine assessment for delirium in the ICU. As a result of trends toward lighter sedation, most patients are aware of the ICU surroundings and require consistent and frequent reorientation to all aspects of their care. Reorientation may enhance patients’ feelings of security and comfort, allow them to more accurately interpret these stimuli, and ultimately reduce delirium. However, communication with sedated or nonresponsive critically ill patients is often not optimal24e26 and is often considered to be a low priority in the ICU setting.27 A review of nurse-patient communication in the ICU found that nurses communicate poorly with patients, despite a high level of knowledge and skill with respect to communication. High stress levels and preoccupation with physical care and technology are potential explanations.26 Although most critically ill patients are sedated and many appear nonresponsive, several studies have documented that patients hear, understand and respond emotionally to what is being said even when healthcare providers assumed they were not aware.28,29 In interviews 48 h after ICU discharge, patients were not able to recall their nurse’s name, but did recall detailed explanations given to them by nurses.28 Automated messages about the ICU environment can provide consistency of information, augment the communication provided by nurses at the bedside, and may enhance the critically ill patient’s feelings of comfort. Inclusion of the patient’s name in the automated reorientation message may create greater attention to the message. Providing reorientation through scripted, automated, recorded messages may mitigate the reduction of orientation to the environment, which is a central feature of delirium, and reduce the occurrence of delirium. In our study, messages recorded in a family member voice familiar to the critically ill subject were particularly effective. Several small studies have evaluated the safety of messages recorded by family on head injured comatose patients.30e32 Walker and associates31 investigated the effects of taped messages by a family member on physiological functioning in a convenience sample of 10 comatose patients. The findings support family interaction via family voice taped messages was safe, even though no significant differences were observed. Tavangar and colleagues32 examined the effects of family members’ voice on level of consciousness in 40 comatose patients. There was a significant difference between the mean daily GCS scores in two groups (p ¼ 0.003), indicating that family members’ voice can increase level of consciousness of comatose patients. However, none of these studies have assessed delirium and non-comatose patients. Our study using recorded family voice to improve orientation and reduce delirium is a novel approach which has not been previously described in the research literature nor considered in recent clinical guidelines; the data in our small randomized trial of 30 subjects supports beneficial effects of the intervention on reducing delirium occurrence. C.L. Munro et al. / Heart & Lung xxx (2017) 1e5 Limitations The sample size of this study was small. The small sample size precluded subgroup analysis to identify potential moderating factors However, the automated voice reorientation intervention demonstrated a statistically significant effect, and these data provided preliminary results for a larger randomized controlled trial (NIH R01 NR016702; ClinicalTrials.org identifier NCT03128671). Not all subjects in the intervention groups received the maximum 3 days of intervention. The primary reason for not receiving 3 days of intervention was improvement in clinical condition resulting in discharge from the ICU, which potentially attenuated the intervention effect. Implications for future research and clinical practice While the results of this small study are promising, additional research is needed. Replication in a larger sample is required to confirm the effect of the intervention. The mechanisms underlying the intervention effect have not been elucidated, nor have mediating factors such as age and gender been explored. Since ICU delirium is associated with persistent disability,7e14 future research should investigate whether the intervention mitigates long term problems experienced by ICU survivors. Although no recommendation for changes in clinical practice can be made without additional research, the potential to augment information provided by clinical providers with automated messages is intriguing. Such messages might be helpful in reducing other symptoms experienced by patients in the ICU, including anxiety about the unfamiliar ICU environment. The differential effect of family voice supports the importance of involving family members in care of ICU patients. Finding meaningful ways to engage families may result in better outcomes for both patients and families. Conclusion Reorientation through automated, scripted messages reduced incidence of delirium in critically ill adults. Using identical scripted messages, family voice was more effective in reducing delirium than an unknown voice. While promising, a more robust examination of the effects of this intervention, using rigorous methods in larger samples, is warranted. The automated reorientation intervention we report here is a simple but potentially powerful strategy to provide structured information to patients on a regular basis, and its effectiveness is enhanced when the message is delivered in the voice of a family member. Because the intervention has a strong nursing care focus, it has the potential to affect delirium in ways that are distinct from but synergistic with medical care, which has focused primarily on pharmacologic management of delirium. The ease of implementation of this intervention combined with its low cost make it an attractive strategy to reduce risk of delirium in critically ill adults. References 1. APA. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Publishing; 2013. DSM-5. 2. Barr J, Fraser GL, Puntillo K, Ely EW, Gelinas C, Dasta JF, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41(1):263e306. 3. Zhang Z, Pan L, Ni H. Impact of delirium on clinical outcome in critically ill patients: a meta-analysis. Gen Hosp Psychiatry. 2013;35(2):105e111. 4. Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell Jr FE, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291(14):1753e1762. 5 5. Pisani MA, Kong SY, Kasl SV, Murphy TE, Araujo KL, Van Ness PH. Days of delirium are associated with 1-year mortality in an older intensive care unit population. Am J Respir Crit Care Med. 2009;180(11):1092e1097. 6. Shehabi Y, Riker RR, Bokesch PM, Wisemandle W, Shintani A, Ely EW. Delirium duration and mortality in lightly sedated, mechanically ventilated intensive care patients. Crit Care Med. 2010;38(12):2311e2318. 7. Gunther ML, Morandi A, Krauskopf E, Pandharipande P, Girard TD, Jackson JC, et al. The association between brain volumes, delirium duration, and cognitive outcomes in intensive care unit survivors: the VISIONS cohort magnetic resonance imaging study*. Crit Care Med. 2012;40(7): 2022e2032. 8. Morandi A, Rogers BP, Gunther ML, Merkle K, Pandharipande P, Girard TD, et al. The relationship between delirium duration, white matter integrity, and cognitive impairment in intensive care unit survivors as determined by diffusion tensor imaging: the VISIONS prospective cohort magnetic resonance imaging study*. Crit Care Med. 2012;40(7):2182e2189. 9. van den Boogaard M, Schoonhoven L, Evers AW, van der Hoeven JG, van Achterberg T, Pickkers P. Delirium in critically ill patients: impact on long-term health-related quality of life and cognitive functioning. Crit Care Med. 2012;40(1):112e118. 10. Jackson JC, Ely EW. Cognitive impairment after critical illness: etiologies, risk factors, and future directions. Semin Respir Crit Care Med. 2013;34(2): 216e222. 11. Girard TD, Jackson JC, Pandharipande PP, Pun BT, Thompson JL, Shintani AK, et al. Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Crit Care Med. 2010;38(7):1513e1520. 12. Wolters AE, van Dijk D, Pasma W, Cremer OL, Looije MF, de Lange DW, et al. Long-term outcome of delirium during intensive care unit stay in survivors of critical illness: a prospective cohort study. Crit Care. 2014;18(3):R125. 13. Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, et al. Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369(14):1306e1316. 14. Brummel NE, Jackson JC, Pandharipande PP, Thompson JL, Shintani AK, Dittus RS, et al. Delirium in the ICU and subsequent long-term disability among survivors of mechanical ventilation*. Crit Care Med. 2014;42(2):369e377. 15. Al-Qadheeb NS, Balk EM, Fraser GL, Skrobik Y, Riker RR, Kress JP, et al. Randomized ICU trials do not demonstrate an association between interventions that reduce delirium duration and short-term mortality: a systematic review and meta-analysis. Crit Care Med. 2014;42(6):1442e1454. 16. Hsieh SJ, Ely EW, Gong MN. Can intensive care unit delirium be prevented and reduced? Lessons learned and future directions. Ann Am Thorac Soc. 2013;10(6):648e656. 17. Grap MJ, Blecha T, Munro C. A description of patients’ report of endotracheal tube discomfort 6034. Intensive Crit Care Nurs. 2002;18(4):244e249. 18. Granja C, Lopes A, Moreira S, Dias C, Costa-Pereira A, Carneiro A. Patients’ recollections of experiences in the intensive care unit may affect their quality of life. Crit Care. 2005;9(2):R96eR109. 19. Roberts BL, Rickard CM, Rajbhandari D, Reynolds P. Factual memories of ICU: recall at two years post-discharge and comparison with delirium status during ICU admissionea multicentre cohort study. J Clin Nurs. 2007;16(9):1669e1677. 20. Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. 2001;286(21): 2703e2710. 21. Neto AS, Nassar Jr AP, Cardoso SO, Manetta JA, Pereira VG, Espósito DC, et al. Delirium screening in critically ill patients: a systematic review and metaanalysis. Crit Care Med. 2012;40(6):1946e1951. 22. Jackson JC, et al. A prospective investigation of long-term cognitive impairment and psychological distress in moderately versus severely injured trauma intensive care unit survivors without intracranial hemorrhage. J Trauma. 2011;71(4):860e866. 23. Saczynski JS, Marcantonio ER, Quach L, Fong TG, Gross A, Inouye SK, et al. Cognitive trajectories after postoperative delirium. N Engl J Med. 2012;367(1): 30e39. 24. Elliott R, Wright L. Verbal communication: what do critical care nurses say to their unconscious or sedated patients? J Adv Nurs. 1999;29(6):1412e1420. 25. Finke EH, Light J, Kitko L. A systematic review of the effectiveness of nurse communication with patients with complex communication needs with a focus on the use of augmentative and alternative communication. J Clin Nurs. 2008;17(16):2102e2115. 26. Llenore E, Ogle KR. Nurse-patient communication in the intensive care unit: a review of the literature. Aust Crit Care. 1999;12(4):142e145. 27. Hagland MR. Nurse-patient communication in intensive care: a low priority? Intensive Crit Care Nurs. 1995;11(2):111e115. 28. Green A. An exploratory study of patients’ memory recall of their stay in an adult intensive therapy unit. Intensive Crit Care Nurs. 1996;12(3):131e137. 29. Lawrence M. The unconscious experience. Am J Crit Care. 1995;4(3):227e232. 30. Treolar DM, Nalli BJ, Guin P, Gary R. The effect of familiar and unfamiliar voice treatments on intracranial pressure in head-injured patients. J Neurosci Nurs. 1991;23(5):295e299. 31. Walker JS, Eakes GG, Siebelink E. The effects of familial voice interventions on comatose head-injured patients. J Trauma Nurs. 1998;5(2):41e45. 32. Tavangar H, Shahriary-Kalantary M, Salimi T, Jarahzadeh M, Sarebanhassanabadi M. Journal of Immunology; 2000.