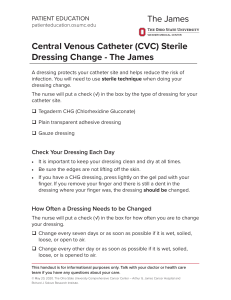
Assessment: specific site of CVAD confirmation of catheter tip location prior to initial use site condition and appearance vital signs including heart rate and rhythm and body temperature daily assessment for the need of central venous access device continuation clear labels on all lines fluid and/or medication infusing at the prescribed rate any indicators of infection (erythema, warmth, swelling, tenderness, discharge) Equipment: 1. Dressing change kit/sterile gloves/sterile drape 2. Chlorhexidine (ChloraPrep): 3 med checks 3. Anti-microbial patch (Biopatch) or Chlorhexidine impregnated dressing 4. Masks for everyone in the room 5. Injection/access cap 6. If PICC line, then catheter securing device (stat lock) shall also be required as per patient size. 7. Clean gloves Patient Education: Educate patients on the signs and symptoms of complications. Educate patients to avoid activities that damage the lines. Educate pt. on care of port procedures prior to discharge. Educate patient/family/caregiver on how to take care of the line: how to change the dressing, flush the line, what to do when the lines are blocked, etc. Concept Map – Connecting the Dots Central Line Dressing Change Description of skill: A central line is a catheter that empties into a central vein. Central lines are more effective than peripheral catheters for administering large volumes of fluid, PN, and medications or fluids that irritate veins, and for repeated and longer durations. Proper care of insertion sites is critical for the prevention of central line–associated bloodstream infection (CLABSI). Sterile dressing changes are done weekly using a maintenance bundle to prevent central line associated bloodstream infection. Potential Complications: Nursing Interventions: Phlebitis: Always assess and palpate the body and extremities. Catheter can float in the right side of the heart: Prior to initial use confirm the location with an X ray and receive “okay to use” order Occlusion or Blockage: do not force anything if it is occluded, immediately inform the HCP. Dysrhythmia-abnormal heart pattern indicated on the electrocardiogram: Notify the HCP Infection: Take vital signs and carefully look for signs and notify the HCP. Indications: Central lines are used when: There is a lack of a peripheral IV site. Extended IV treatment is needed (going home with chemo, IV etc.) Vesicant or irritant solutions are to be used (chemo/PN) Trauma and burn resuscitation High volume flow required very quickly Many different types of fluid required at one as in critical care For frequent draws (PICC lines are often used) Evaluation: The patient will verbalize the importance of reporting insertion site discomfort, pain, burning, throbbing by the end of shift. The patient will verbalize any feeling of malaise the moment he/she feels it. The patient will verbalize understanding care of port at home, if discharged. Delegation/Collaboration: At first, a nurse should know about the hospital policy. A nurse must collaborate with the HCP, the patient, their family and whoever has a role in taking care of the patient. Any abnormalities of discomfort exhibited by the patient should be readily communicated to the HCP. Documentation: Must be done per every shift. Documentation: Catheter type Location Necessity Site assessment Length of catheter outside of skin Patency of all lumens Interventions (dressing change, flushing) Dressing assessment (sterility, integrity, tegaderm off etc.)