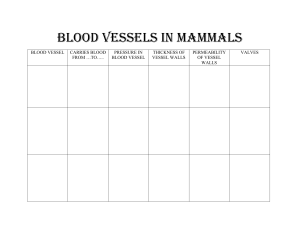
Blood vessels Chapter 10 Blood vessels • Components of circulatory system that transport blood cells, nutrients, and oxygen to tissues of the body. They also take waste and carbon dioxide away from the tissues. • There are five types of blood vessels: 1. Arteries: which carry the blood away from the heart 2. Arterioles (most responsible for BP(Large surface area & sphincters help control BP)—sphincters can divert blood to diff parts of body 3. Capillaries: exchange of water and chemicals (gas exchange) between blood and tissues 4. Venules 5. Veins: which carry blood from capillaries back to heart • Avascular structures: cartilage, epithelium, lens and cornea • Slower healing time d/t less blood & cannot repair (blood always for inflammation—blood carries healing warriors to get in /repair) • Away from heart: arteries, arterioles, capillaries (gas exchange), venules, veinsback to heart (circles back) Structure and function Vascular specialization based on thickeness/composition d/t hemodynamic forces/tissue requirement. • Smooth muscle cells (SMC) • Extracellular matrix (ECM) • Endothelial cells (EC) • Arteries: higher pressure generated from heart so reinforced w/ layers of SMCs ((lose pressure as we come back up towards heart). Most oxygen • Arterioles: the ratio of wall thickness to lumen diameter increases to allow for precise regulation of intravascular pressure. • Capillaries: single-cell lining of EC. On basement membranes ((gas exchange)) • Veins: thin-walled walled • Veins: valvesrely on muscles to squeeze the valves to increase the pressure and push blood upward. • Venules: are not deoxygenated, a little left. • Vessel walls in 3 concentric layers: intima, media, adventitia. (present in all vessels, more apparent in larger vessels=arteries. • Intima: EC monolayer on basement membrane w/ minimal underly ECM • Media: ((muscle layer of vessel)), mostly SMC and ECM, surrounded by loose connective tissue, nerve fibers • Vessel walls in 3 concentric layers: intima, media, adventitia. (present in all vessels, more apparent in larger vessels=arteries) • Intima: EC monolayer on basement membrane w/ minimal underly ECM; separated from media by dense elastic membrane called internal elastic lamina • Media:mostly SMC and ECM, surrounded by loose connective tissue, nerve fibers, and smaller vessels of adventitia. External elastic lamina present in arteries to define transition btw media and adventitia • Adventitia ( tunica externa) Endothelium • Endothelium is a continuous sheet of cells lining entire vascular tree that regulates aspects of blood and blood vessel function • Single cell layer. Endo=inner part that touches blood in the veins/arteries. • Endothelium cells (EC)-line vascular, regulates blood flow/function • EC maintains non-thrombogenic, modulate inflammation, influence growth/behavior of cell (particularly SMCs) • Impermeable, except during hemodynamic stresss (HTN) OR vasoactive (histamine,chemokines-inflammation/immune). • EC’s—active role in recruit of WBC during inflammation • Atherosclerosis- d/t EC damage • Basal state normal BP, laminar flow, stable growth factors & this maintains antithrombosis, surface and SM tone. • Want Laminar flow—want blood straight, NO turbulence OR stagnation • Injury/exposure to mediators endothelial activation(EC develop adhesives, procoagulant surface, factors to contract SM and/or proliferation . Endothelia damage leads to inflammation and can cause hypercoagulable state (triad- vessel damage, hypercoag state, turbulent flow= recipe for clot)). Vascular smooth muscle cells • Smooth muscle cells (SMC) participate in BOTH normal & pathologic process (atherosclerosis) • When stimulated by various factors • Proliferate • Upregulate (proliferate)- ECMincrease collagen, elastin, and proteoglycan production (building blocks, form new cells) • Elaborate growth factors and cytokines • SMC’s mediate vasoconstriction/vasodilation (response in physiology or pharmacologic) • Platelet derived growth factor & recruit more. SMCs maintenance factors—heparan, NO, growth factors • Smooth muscle—SM cells regulate repair and scar. Production of collagen for scar formation —(scar meansglue genitor) Vascular smooth muscle cells • When Endothelium damage---SM cells will leave spot, may go through endothelium, & producing the extracellular matrix • Elaborate extracellular matrix is NOT good in excessive amts—can cause vessel damage, seeding of atheroscleroma. • Protective and healing but Want to keep this under control. • SM cells also contract Blood pressure Blood pressure- various factors, important to know factors in order to know how to treat BP • Function of cardiac output and vascular resistance • CO = HR x SV (amt of blood pushing out & how quickly) • (BP=CO x VR) • Vascular resistance is primarily a function of arterioles (large surface area & sphincters-help squeeze/shunt blood to areas that need it). Ex: when exercising your muscles need more blood, arterioles help this w/ shunting. When digesting more blood towards digestive organs & arterioles responsible for this) • CO influenced by blood volume. Blood volume influenced by renal sodium excretion /resorption • SV (heart squeeze): filling pressure (regulated Na and its effect on blood volume ) ---Na rolesatrial natriuretic peptides, renin, angio, aldosterone • Second SV factor: HR & myocardial contractility (both regulated by alpha/beta-adrenergic systems) • Peripheral resistance: mainly d/t arterioles by neural & humoral inputs • Balance btw vasoconstriction (Ang II, catecholamines, endothelin, thromboxane, leukotrienes) & vasodilators (kinin, prostaglandins, NO) • Humoral—SNS & PNS work together to regulate peripheral resistance (antagonistic) • Increased blood flow causes vasoconstriction to protect against hyperperfusion • Local BP factors: autoregulation by tissue pH & hypoxia/metabolic demands • Other: inflammation, diseases (also work on vascular as well) Blood pressure Hypertension Hypertensive vascular disease • Genetic and environmental factors that conspire to increase blood volume and/or peripheral resistance • Essential HTN: results from interplay of several genetic factors, that individually may not cause increase. Environmental factors—which increase blood volume and/or peripheral resistance • Age, atherosclerosis, build up of cholesterol, increase blood volume, sluggish blood • HTN: increase risk for atherosclerosis d/t damaging endothelial layer---breaks off—plaque forms Clinically • > 140 mm Hg Systolic (ventricle contraction) • > 90 mm Hg Diastolic (ventricle relaxation) • Increased risk for atherosclerosis (narrows b.v) • High pressure (BP) causes damage to vessel walls d/t turbulence (bc when pressure high & hits something, will not be laminar anymore. • Vessel damage & turbulence = build up extracellular matrix, scarring (which makes blood flow even less) eventually can lead to atherosclerosis(is build up of proteins, fats @ area of vessel damage) • 95% of cases are idiopathic(primary/essential) • Increased CO= increased BP • Increased blood volume & resistance Mechanisms of essential (primary/idiopathic) hypertension Primary (essential/idopathic) vs secondary will have different treatments (so, we need to know this) • Reduced sodium excretion (too much H20=too much blood). **Hydrostatic pressuremajor role in getting blood where it needs go. More Na in b.v & water follows salt • Increased vascular resistance (going to resist flow from capillaries to venules bc there’s backup—bc hard to push through or backup at arterials. Either way hard to squeeze fluid into OR from capillaries= HTN • Genetic/environmental • Primary (essential/idiopathic): unknown cause (probably d/t aging & less flexible vessels) • Ex: reduced Na excretion in presence of normal arterial pressure** • • (incr Na=incr fluid=incr blood vol=incr CO=incr BP) Other ex: increase VR from vasoconstriction /structural changes in vessel walls, genetic factors, environmental –stress, wt, smoking, fitness, diet • Secondary: identifiable underlying condition (renal dx, renal artery stenosis, adrenal disorders, cancer or tx of cancer). HTN is secondary to known cause. Morphology HTN accelerates atherogenesis AND also causes degenerative changes in walls of large/medium-sized arteries that can lead to aortic dissection, cerebrovascular hemorrhage. Silent Killer……but…..Once histology changes--severe • Hyaline arteriosclerosis (benign, long-term longer HTN will eventually lead to hyaline arteriosclerosis) • Benign hypertension (deposits of protein that are normally soluble in blood—get concentric rings/concentric thickening). The pressure so high that soluble proteins (like albumin) are pushed out of solubility and deposit overtime along lumen wall ==narrowing (lead to turbulence & damage) • Arterioles wall thicken w/ deposit of protein over time = narrow lumen • Ex: hyaline arteriosclerosis in kidney = nephrosclerosis (glomerular scarring) • Hyperplastic arteriosclerosis • Severe hypertension (malignant) (above 200’s) • • Can cause Onion skinning unraveling of b.v bc so much pressure (2nd picture) • BP so high is kind of blows out vessel = onion skinning • Ex: fibrinoid—vessel wall necrosis= necrotizing arterioles (mostly in kidney) Autopsy-this is how they know HTN--histology Vascular disorder Vascular wall injury (particular to EC) • Injury to the vessel walls is the fundamental basis for majority of vascular disorders • Injury d/t: biochemical, immunological, hemodynamic (HTN) • Endothelial cells-& underlying SMC critical for vasculature response for homeostasis • Can lead to weakened walls • Can lead to thickened walls (fibrosis of dead cells) and stenosis (hardening & narrowed of lumen) • The smooth muscle cells that are trying to protect you, start adding more matrix, if continued damage then more and more matrix. Builds up and narrows vessel (stenosis) • Weakened stimulates recruitment for to repair damage but this in turn creates more damage and if recurrent insults= thickening (narrowing of vessel) • EC injury/dysfunction=pathologic process including thrombosis, atherosclerosis, HTN vascular lesion, infection, inflammation, immune response, trauma, toxic exposure Vascular wall injury Smooth muscle cells multiple thr mitosis –produce extracelluar matrix and maybe too much of it (if constantly happening) Arteriosclerosis Arteriosclerosis (hardening vessels (arterioles) this is not atherosclerosis* • Literally “hardening of the arteries”; generic term for thickening and loss of elasticity. (less pliable) • Affects small arteries and arterioles and may cause downstream ischemic injury. • Hypoperfusion-hypoxia-ischemia-infarction/necrosis (cell death d/t lack of perfusion=infarction but example of necrosis) • Arterial wall thickening = loss of elasticity • ?class notes?--elastic to pump blood out to body, when small arterioles/capillaries harden difficult to repair. Capillaries-where gas exchange= (this leads to loss of O2 and ischemia). Recruitment of repair factors 1st go to arteries ? • Arteriolosclerosis—affects small arteries/arterioles causing downstream ischemic injury • 2 types: hyaline & hyperplastic arteriolosclerosis Atherosclerosis Atherosclerosis (intimal lesions called atheromas—the fat ball. But if atheroma ruptures & breaks off, travels thr body to small vessel= Embolus) • Characterized by intimal lesions called atheromas that impinge on vascular lumen and can rupture to cause sudden occlusion • Endothelia lesion-- Narrow lumen—Rupture. Could then cause embolus—stuck in lungs or even brain • Ubiquitous (everywhere) among developed nations (put statins in water) • Cause of pathogenesiscoronary,cerebral,PVD • Atheromas-plaque w/ raised lesions, lipid core (cholesterol, necrotic debris), covered by fibrous cap. • Enlarged atherosclerotic plaques—obstruct lumen=stenosis • If rupture thrombosis/occlusion of vessel (ischemia) Atherosclerosis risk factors---aging sucks! • Modifiable=environmental (all diet and also smoking—destroys small bv like DM—neuropathies=damaged capillaries) • **DM II & smoking **** ************************ • Smoking: internal damage • *(Nutrition)* hyperlipidemia (cholesterol) major risk factor, even if other risk factors were excluded. • ECG heart pattern changes= HIGH risk & harder to treat • Genetic disease called: Hypercholesterolemia so much cholesterol builds under skin, cholesterol even build up under eye lids, knees, elbows (called--xanthomas) Risk factors • Hyperlipidemia—and, more specifically, hypercholesterolemia (LDL,HDL, triglycerides)—is a major risk factor for development of atherosclerosis and is sufficient to induce lesions in the absence of other risk factors • Modifiable risk factors • • • • • Diet (less cholesterol/fat)* Hypertension Cigarette smoking Diabetes mellitus ECG heart pattern changes=high risk/diff to tx Statins • Top 3 prescribed drugs U.S. • Drug that inhibits the rate-limiting enzyme in hepatic cholesterol biosynthesis • • Blocks cholesterol building cells in liverinhibits building of chains=less cholesterol Cholesterols are good in moderation: need for cell membrane-stability, hormone synthesis (cause of severe eating disorders—cannot synthesis hormones—loss of period) Structure of atheroma (not functional tissue) Atheroma---crust w/ gooey center Endothelium displayed d/t increased harden ECM (via smooth muscle cells) Fibrous Cap filled w/ collagen (glue) Macrophages that eaten too much fat Not functional tissue. Center is cholesterol crystals, cell debris, calcium deposits—harder to dissolve (much easier to prevent than treat) • What happens? • If this ruptures & from enough damage—fat lead to emboli (if dislodged) • Narrows lumen • Underneath atheroma---also damage: • Another reason atheroma can break off---bc attachment is damaged Atherosclerosis formation • The currently held view of pathogenesis is embodied in the response-toinjury hypothesis. This model views atherosclerosis as a chronic inflammatory response of the arterial wall to endothelial injury. • Injury-increase ECM, narrow lumen, more turbulent flow, hypercoag state. More river bends=turbulence & w/ each bend, deposit rocks/branches. Same in vessel, too much of a bend (narrow lumen) w/ turbulence = deposit proteins & fats • EC injury-damage blood vessels= atherosclerosis • Vessel injuryinflammationmore pressure/injury d/t recruit brought to endotheliumbuild up plaque • Other 2 top causes= hemodynamic disturbance (HTN, turbulent blood flow) & hypercholesterolemia Correlating inflammation • CRP=inflammation. Risk of atheroma increases in CRP. • Marker synthesized by liver in response to inflammatory cytokines. Atherosclerosis formation (vessel injury = inflammation = fat deposit @ site = turbulent flow = SMC seals off w/ cap) 1. EC injury—and resultant endothelial dysfunction—leading to increased permeability, leukocyte adhesion, and thrombosis (d/t inflammation) 2. Accumulation of lipoproteins in the vessel wall 3. Platelet adhesion (PAF)—narrow lumen 4. Monocyte adhesion to the endothelium, migration into the intima, and differentiation into macrophages and foam cells 5. Lipid accumulation within macrophages, which respond by releasing inflammatory cytokines 6. SMC recruitment due to factors released from activated platelets, macrophages, and vascular wall cells 7. SMC proliferation and ECM production (more fibrin and collagen) Atherosclerosis formation • Endothelia damage—bring inflammatory mediators (army), if consistent damage-build defense force of hardened material • Initial Fatty streak is biggest sign of atheroma/atherosclerosis –runway for all things bad ((fatty streak is a sign)) • Eventually Atheroma Atherosclerosis morphological evolution • Fatty streak- landing site for atheroma. At this pt can still reverse things • Atherosclerotic plaque Atherosclerosis clinical changes • Plaque inflammation increases collagen degradation and reduces collagen synthesis, thereby destabilizing the mechanical integrity of the cap. • Plaque erosion or rupture triggers thrombosis, leading to partial or complete vascular obstruction and often tissue infarction • Rupture/thrombus • Hemorrhage into plaque • Atheroembolism • Aneurysm formation • Certain cells/enzymes to degrade some of the plaque but if already fatty center—cannot do this bc destabilizes the cap. Deposit more cap but body has balance system bc doesn’t want too much scar tissue = Destabilizing mechanical cap (high risk of rupturing) • Plaques are unstable-- leak out fat =thrombus, if moves then embolism (atheroembolism) • This can also weaken vessel---increase risk for aneurysm formation. Aneurysm= blown out vessel—too large and ruins laminal flow, risks for dissection (complete rupture of vessel) • Dissection: separating layers of vessel this weakens vessel risk for compete blow out of vessel. Atherosclerosis clinical changes If occlude coronary—no O2 supply to myocardium = infarction Atherosclerosis clinical changes Types of plaques • Certain types of plaques are believed to be at particularly high risk of rupturing. • Stable plaque ischemia • Vulnerable plaque thrombosis and embolization • Stable plaque—underneath plaque can get necrosis bc endothelial cells also need O2 O2 comes from blood but if endothelium cell covered d/t atheroma or EC get damaged bc of atheroma ==not receiving much O2 • Everything under has potential to die (necrosis) = death d/t lack of blood = ischemia Atherosclerosis clinical consequences • Myocardial infarction (heart attack) • Cerebral infarction (stroke)—occlusion in brain (FAST) • Aortic aneurysm • Peripheral vascular disease (gangrene of extremities) • Many plaques are asymptomatic until rupturing Aneurysms and dissections Aneurysms and dissections • Aneurysms are congenital or acquired dilations of blood vessels or the heart (outpouching of b.v) • “True” aneurysms involve all three layers of the artery—intima, media, and adventitia or the attenuated wall of the heart= dissection. (risk for hemorrhage)*** • Two most important predisposing conditions for aortic aneurysms are atherosclerosis and hypertension Aneurysms and dissections Aneurysms and dissections • Abdominal aortic aneurysm (AAA)- not good, can burst. Under most pressure in body, diseasesMarfan’s syndrome-flexible bc problem w/ connective tissue/fibrin—increased risk. • Thoracic aortic aneurysm • Aortic dissection Vasculitis Vasculitis • Vasculitis is a general term for vessel wall inflammation. The two most common pathogenic mechanisms of vasculitis are immune-mediated inflammation and direct vascular invasion by pathogens. Immune complex-mediated hypersensitivity • Type III • Immune complexes formed in the circulation deposit in vessels, leading to complement activation and acute inflammation. • IgG and IgM • Neutrophils • Macrophages hard time eating small immune complexes, deposit vessel walls. Neutrophils destroys area Vasculitis Blood vessel hyperactivity Reynaud phenomenon • Vasoconstriction of arteries and arterioles in extremities, particularly the fingers and toes • Restricted blood flow induces paroxysmal pallor or cyanosis • Cold temperatures or emotional stress • Females > Males • Extreme loss of blood flow—emotional stress=SNS clamps down vessels Varicose veins • Abnormally dilated tortuous veins produced by chronically increased intraluminal pressures and weakened vessel walls • Valves- catch gravity fallen blood, continue to push blood up (push up,catch, repeat). Valves destroyed— blown out & not returning blood to heart. • Small risk for DVT d/t varicose veins. Varicosities of other Sites • Esophageal varices • Liver cirrhosis causes portal venous hypertension (too much back up of blood=too much pressure) • Esophageal varices are prone to ruptures that can lead to massive (even fatal) upper GI hemorrhage • Hemorrhoids • Varicose dilations of venous plexus at anorectal junction from prolonged vascular congestion associated with pregnancy or straining to defecate • Source of bleeding and are prone to thrombosis and painful ulceration