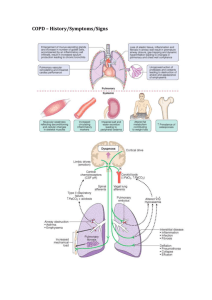
Chronic Obstructive pulmonary Disease Madina Mohmmed Eljack Saadia yousif Mohmmed Makkia Hassan Noury by the end of this seminar students will be able to:= *define COPD? *explain patho physiology *recognize Causes of COPD * out line Symptoms of COPD *Know stages of COPD *differen tiate between COPD and asthma? *Identify Diagnostic tests needed for COPD *know Medical management of COPD &Preventive measures *Know how to assess patient with COPD *Nursing intervention *Complication of COPD COPD as a disease state is characterized by chronic airflow limitation due to chronic bronchitis and emphysema. . Chronic bronchitis has been defined in clinical terms: the presence of chronic productive cough for at least 3 consecutive months in 2 consecutive years Emphysema, on the other hand, has been defined by its pathologic description an abnormal enlargement of the ◦ air spaces distal to the terminal bronchioles accompanied by destruction of their walls and without obvious fibrosis 30% of smokers develop COPD 20% of adult males have COPD 15% of COPD patients are severely symptomatic 4 th leading cause of death (USA) Mortality rate still rising prevalence in low birth weight and low socioeconomic status Tuberculosis in smokers predisposes to COPD COPD Prevalence, by Sex, in US, 1980–2000 (Self-Reported Emphysema or Chronic Bronchitis) Millions of adults aged 25 and older 8 7 6 5 4 3 2 1 0 1980 1985 1990 Men Mannino DM, et al. MMWR. 2002; 51(SS-6):1–20. 1995 Women 2000 70 60 50 40 30 20 10 0 1980 1985 1990 Men Women 1995 2000 5.5% Asthma 3.2% Chronic bronchitis 1.5% Emphysema 1.6% Airflow obstruction int. 3.1% Airflow obstruction ext. NHANES III NHANES III Current Diseases as a Proportional Venn Diagram. Soriano et al. Chest. 2003;124:474-481. In COPD, less air flows in and out of the airways because of one or more of the following: The airways and air sacs lose their elastic quality. The walls between many of the air sacs are destroyed. The walls of the airways become thick and inflamed. The airways make more mucus than usual, which tends to clog them. (tobacco smoke, pollutants, occupational agent) NOXIOUS AGENT Genetic factors Respiratory infection Other Causes of COPD •Smoking •Air pollution •genetic (hereditary) risk Smoking is the leading cause of COPD History of childhood respiratory infection Genatic Increasing age Productive cough Breathlessness Chest infection Other symptoms of COPD can be more vague, weight loss, tiredness and ankle swelling. Chronic bronchitis Chronic cough Shortness of breath Increase mucus Frequant clearining of throat Simple chronic bronchitis Chronic muco purulent bronchitis Chronic bronchitis with obstruction Chronic bronchitis with obstruction and airway hyper reactivity primary symptom of Emphysema Chronic cough Shortness of breath Limited activity level Centri acinar ( centri lobular) emphysema Pan acinar emphysema Para septal emphysema Senile emphysema Symptoms Physical examination Sample of sputum Chest x-ray High-resolution CT (HRCT scan) Pulmonary function test (spirometery) Arterial blood gases test Pulse oximeter Type ◦ dry, moist, wet, productive, hoarse, hacking, barking, whooping Onset Duration Pattern ◦ activities, time of day, weather Severity ◦ effect on ADLs Wheezing Associated symptoms Treatment and effectiveness amount color presence of blood (hemoptysis) odor consistency pattern of production 0 FEV1 Normal COPD 1 Liter 2 FVC FEV1/ FVC 4.150 5.200 80 % 2.350 3.900 60 % FEV1 3 COPD 4 FVC FEV1 Normal 5 1 2 3 FVC 4 5 6 Seconds Diagnosis of COPD EXPOSURE TO RISK FACTORS SYMPTOMS cough sputum dyspnea tobacco occupation indoor/outdoor pollution SPIROMETRY Stage(0) at risk Stage (1) mild COPD Stage(2) modarate COPD Stage (3 ) sever COPD The stages of COPD are defined primarily by lung function . This emphasises the important clinical message that the diagnosis of COPD requires the measurement of lung function. The stages of COPD suggested in the GOLD Guidelines are as follows. * . Stage 0: At risk, cough or sputum present but lung function normal Stage 1: Mild COPD, FEV1/forced vital capacity (FVC) <70%, with an FEV1 80% predicted, with or without chronic symptoms. *Stage 2: Moderate COPD, FEV1/FVC <70% and FEV1 % pred>30% and <80%. Stage 2 is split at an FEV1 of 50% pred since the existing data support the value of inhaled corticosteroids below an FEV1 of 50% pred but not above. * Stage 3: Severe COPD, FEV1 <30% pred and FEV1/FVC <70%. FEV1/FVC • <0.70 FEV1 ≥80% • predicted I: Mild FEV1/FVC <0.70 • 50% ≤FEV1 <80% • predicted II: Moderate FEV1/FVC <0.70 • 30% ≤FEV1 <50% • predicted III: Severe FEV1/FVC <0.70 • FEV1 <30% • predicted or FEV1 <50% predicted plus chronic respiratory failure IV: Very Severe Active reduction of risk factor(s): influenza vaccination Add short-acting bronchodilator (when needed) Add regular treatment with one or more long-acting bronchodilators (when needed): Add pulmonary rehabilitation Add inhaled glucocorticosteroids if repeated exacerbations Add long-term oxygen if chronic respiratory failure Consider surgical treatments Global Initiative for Chronic Obstructive Lung Disease (GOLD). NHLBI/WHO Workshop report. www.goldcopd.com antibiotics to treat infection bronchodilators to relieve bronchospasm, reduce airway obstruction, mucosal edema and liquefy secretions. Chest physiotherapy and postural drainage to improve pulmonary ventilation. Proper hydration helps to cough up secretions or tracheal suctioning when the patient is unable to cough. Steroid therapy if the patient fails to respond to more conservative treatment. BRONCHODILATORS Adrenergic agents (ventoline) Beta-agonists bind to B2 receptors on airway and result in smooth muscle relaxation and bronchodilation Inhaled route is preferred Acute relief of symptoms Anti-cholinergic agents(ipatropium) Bind to acetylcholine receptors and result in bronchodilation (of mostly larger airways) Reduces sputum production Inhaled route is preferred Methylxanthines (i.e. theophylline) Weak bronchodilator Delays respiratory muscle fatigue Reduces trapped lung gas Improves respiratory muscle mechanics Corticosteroids (hydrocortison) Reduce airway inflammation Mucolytic Alter viscosity of sputum May reduce symptoms in some patients Must be used carefully (i.e. avoiding hypotension) Increase exercise tolerance Increase quality of life Improve co-ordination and efficiency of movement Improve strength particularly respiratory muscles Encourage relaxation Confidence in physical abilities Flexibility Exacerbations of COPD can be caused by many factors, including environmental irritants, heart failure or noncompliance with medication use Most often, however, exacerbations are the result of bacterial or viral infection. Bacterial infection is a factor in 70 to 75 percent of exacerbations. oxgination Bronchodilators Anticholingerics Antibiotics Corticosteroids To prevent irritation and infection of the airways, instruct the patient to: Avoid exposure to cigarette, pipe, and cigar smoke as well as to dusts and powders. Avoid use of aerosol sprays. Stay indoors when the pollen count is high. Stay indoors when temperature and humidity are both high Use air conditioning to help pollutants and control temperature Avoid exposure to persons known to have colds or other respiratory tract infection Avoid enclosed, crowded areas during cold and flu season. decrease Obtain immunization against influenza and streptococcal pneumonia To ensure prompt, effective treatment of a developing respiratory infection, instruct the patient to do the following:Report any change in sputum color character, increased tightness of the chest, increased dyspnea, or fatigue. Call the physician if ordered antibiotics do not relieve symptoms within 24 hours In COPD there is permanent damage to the airways. The narrowed airways are fixed, and so symptoms are chronic (persistent). Treatment to open up the airways, is therefore limited. In asthma there is inflammation in the airways which makes the muscles in the airways constrict. This causes the airways to narrow. The symptoms tend to come and go, and vary in severity from time to time. Treatment to reduce inflammation and to open up the airways usually works well. COPD is more likely than asthma to cause a chronic (ongoing) cough with sputum. Night time waking with breathlessness or wheeze is common in asthma and uncommon in COPD. COPD is rare before the age of 35 whilst asthma is common in under-35. History Patient's environment(at both home&work) Work history, exercise pattern, smoking habits The onset & development of symptoms Sleeping positions Cyanosis Nasal flaring Dyspnea Decreased respiratory effort Decreased LOC Accessory muscle use Decreased breath sounds Decreased oxygen saturation Signs of heavy smokers Observe for clubbing Distended neck vein on expiration The presence of barrel chest Observe for abdominal breathing The use of pursed lips breathing and chest movement Auscultate the chest& listen for musical wheezes characteristics of chronic bronchitis review the results of diagnostic procedure: Arterial blood gases Pulmonary function tests X-ray films Gas exchange Impaired R\T decrease ventilation and mucus plug P\E\O The client will maintain adequate gasexchange as evidanced by blood gas values Reguler monitering of RR ABG result Sign of hypoxia and hypercapnia administer low flow oxygin(1to3l\min Assist client in to high fowlers position Administer bronchodialater Use caution when adminster sedatives”(because it can affect respiratory (center and lead to respiratory failure Airway clearance ineffective R\T excessive secretion and in effective coughing P\E\O client will have improved airway Clearance as evidence by Effective coughing technique and minimum sacretion Maintain adequate hydration Increase humidity of enviromental air Coughing technique Chest physical therapy Assess breath sound befor and after coughing Activity Intolerance R\T inadequate Oxygination and dyspnea P\E\O the client will have improved activity tolerance Avoid conditions increase oxygen demand eg Smoking .excess wt . Stress Energy conservation technique Rest periods . Schedule gradual increase in daily activity Maintain supplemental oxygen as needed Anxiety R/T acute breathing defficulties and fear ofsuffocation P\E\O client will express an increase in psychological comfort Use of effective cooping machanism Remain with client during acute episodes of breathing difficulty provide care in a calm reassuring manner Provide quiet calm environment During acute episode limit number of people and un necessary equipment with caution Use of sedative as order Nutrition altered less than body requirment R\Treduce appetite, decrease energy level and dyspnea P\E\O The clientwill maintain body wt ,HB with in normal range Promote mouth care before meal and as needed Advise client to eat small frequent meals Advise pt to avoid gas production foods Instruct pt to use high calorie liquid supplement Sleep pattern disturbance R\T dyspnea and external stemuli P\E\O client will report feeling adequitly rest Promote relaxation Dark , quiet ,ventlated room Follow bed time rotine Schedule care activity Physical exercise during the day Use relaxation techneque (worm bath , music Family processes altered R\T chronic illness of afamily member P\E \O the family veralize their feeling , Participate in the care Seek external resources as needed Incourage participation in planing process Assess family communication Incourage social support system Encourage group support Sexual dys function R\T dyspnea ,reduce energy and change in relationship P\E\O client report increase satisfaction with sexual function Provide opportunity for discuss concern Incourage partener other form of sexual expression Persons with COPD should not get the live attenuated nasal spray flu vaccines (i.e., Flu Mist). The inactivated 2009 H1N1 influenza vaccine can be administered at the same visit as any other vaccine, including the PPSV. Pneumonia vaccine ◦ Reduces risk of common cause of pneumonia Annual flu vaccine ◦ Reduces risk of flu and its complications *Atelectasis. *Pneumothorax. *Respiratory failure. *Cor-pulmonale American Lung Association. Chronic obstructive pulmonary disease (COPD) Fact Sheet, 2003 www.lungusa.org National Heart, Lung, and Blood Institute, NIH. COPD-Key points and How is COPD treated? January, 2006 http://www.nhlbi.nih.gov/health Luckmmans Core principles and practical of Medical surgical nursing Global Initiative for Chronic Obstructive Lung Disease (GOLD). NHLBI/WHO Workshop report. www.goldcopd.com