Nursing Practical Exam Guide: Suctioning, ABG, ECG, Ventilation
advertisement

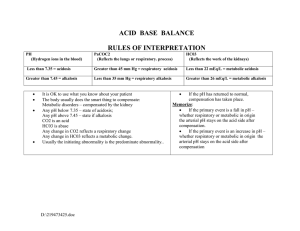
Practical Exam Suctioning (Oral, ET) Hemoglucose test Electrocardiogram Nasogastric Tube Arterial Blood Gas Tracheostomy Tube Care Suctioning Tracheostomy tube care Materials - - Tracheostomy care kit (hydrogen peroxide, sterile water, q tips, buckets, and cannula cleaners, fenestrated tissue,) There are cuffed or uncuffed cannulas Sizes for adults are 6-8 Procedure - Prepare your equipment Wash hands Don sterile gloves Establish sterile field Put sterile water into the three buckets Remove mask Remove inner cannula and put the mask back to oxygenate the patient Clean the cannula with cannula cleaners and sterile water (hydrogen peroxide) Put the inner cannula back Clean the mask and the outer cannula with the tissues if there are mess Use q tips to clean the outer part of the cannula Apply the fenestrated gauze underneath the canula patient can still breathe even without the oxygen mask. Mechanical Ventilation - It is a life sustaining therapy in which a ventilator provides partial or full support for patients with respiratory failure Main goals: maintain adequate gas exchange, to rest respiratory muscles, and to decrease the oxygen cost of breathing. Mechanical Ventilator - it is a positive- or negative- pressure breathing device that can maintain ventilation and oxygen delivery for a prolonged period. Indications: Laboratory Values PaO2 <55 mmHg PaCO2 >50mmHG and pH <7.32 Vital Capacity <10 ml/kg Negative inspiratory force <25 cm H20 FEV1 <10 mL/kg or respiratory rate of >35/min Clinical Manifestations Apnea or bradypnea Respiratory distress with confusion Increased work of breathing not relieved by other interventions Confusion with need for airway protection Circulatory shockcontrolled hyperventilation (e.g., patient with a severe head injury Classification of Ventilators Negative pressure Positive pressure o Most widely used approach to mechanical ventilation is to deliver gas to the lung with positive-pressure ventilation (PPV) applied through an endotracheal tube, a tracheostomy, or a tight-fitting mask. Volume-cycled Ventilators Pressure-Cycled Ventilators High-frequency oscillatory support ventilators Noninvasive positive-pressure ventilation Questions: What is a mechanical ventilation’s purpose? What are the types of mechanical ventilators ABG (Arterial Blood Gas) Analysis Is used to evaluate respiratory function and provide a measure for determining acid-base balance. An acid-base balance must be maintained in the body because alterations can result in alkalosis or acidosis. Why does acid-base imbalance occur? they occur because there is an underlying problem that causes homeostatic problems. This then causes the kidney and/or the lungs to compensate. Hysteria Pain Blood Gas pH PaCO2 HCO3Pa02 Ranges 7.35 – 7.45 35 – 45 mmHg 22 – 26 mEq/L 75 – 100 mmHg Neurological injuries Embolism or edema in the lungs Asthma due to hyperventilation What is the S/Sx of Respiratory Alkalosis? Respiratory Acidosis This occurs when the lungs cannot excrete carbon dioxide from the body and causes the excess CO2 in the lungs to merge with the water in the blood to form acid (common in Emphysema). This causes the blood pH to become acidic and causes the kidney to release more bicarbonate acid through urine to heighten the pH level of the blood. 2 types of respiratory acidosis, Acute and Chronic What causes Respiratory Acidosis? Hypoventilation, COPD, Respiratory conditions, Drug intake (opium) Muscle cramps (due to lack of calcium) Tetany, involuntary muscle contractions (due to lack of calcium) Palpitations (fast heart rate) Positive Chvostek Sign (twitching of cheek muscles when touched near the ear) How to manage Respiratory Alkalosis? Give paper bag, Control Anxiety, medications for lowering respirations, manage underlying conditions What is the S/Sx of Respiratory Acidosis? Confusion, Altered LOC, muscle jerking, Coma Potassium levels rise (>5.0) How to manage Respiratory Acidosis? Bronchodilators, Weightloss, Kayexalate, Adequate hydration, and Mechanical ventilation Respiratory Alkalosis Happens when the body excretes too much carbon dioxide (hyperventilation) What causes Respiratory Alkalosis? Metabolic Acidosis What causes Metabolic Acidosis? Addition of large amounts of fixed acids to body fluids. Lactic acidosis (circulatory failure), Ketoacidosis (diabetes, starvation), Phosphates and sulfates (renal disease), Acid ingestion (salicylates), Secondary to respiratory alkalosis, Adrenal insufficiency What is the S/Sx of Metabolic Acidosis? Hyperventilation Confusion, Altered LOC, muscle jerking, Coma TACHYPNEA Potassium levels rise Temperature increase Kussmaul breathing (heavy fast breathing) Aspirin toxicity Controlled ventilation (hyperventilates) Hyperventilation How to manage Metabolic Acidosis? Bronchodilators, Weightloss, Kayexalate, Adequate hydration, and Mechanical ventilation Metabolic Alkalosis What causes Metabolic Alkalosis? Retention of base or removal of acid from body fluids Vomiting, excessive gastric drainage, potassium depletion (diuretic therapy), burns, excessive NAHCO3 administration What is the S/Sx of Metabolic Alkalosis? Confusion, How to manage Metabolic Alkalosis? Bronchodilators, ABG procedure Equipment Cotton wool and tape Arterial blood gas syringe, Tray with sharps bin gloves (sterile and unsterile), skin preparation solution (2% chlorhexidine in 70% isopropyl alcohol), A patient label, and pen to write down their details including the inspired oxygen concentration. Apron Steps to follow 1. Give a full explanation to the patient in simple terms and ensure that they consent to the procedure 2. Set up your trolley 3. Prepare your trolley as a sterile field. Wear a plastic disposable apron and non-sterile gloves and take alcohol hand rub with you. 4. Attach a 21G or 23G needle to the syringe. A 21G needle is likely to be required for femoral access. Radial Site Collection 1. Conduct Allen test 2. Position the wrist; you can use a towel, pillow, or bag of fluid to extend the wrist (20 – 30 degrees) 3. Feel for the pulse just proximal to the traverse skin crease at the wrist. 4. Clean the skin with antiseptic solution (2% chlorhexidine in 70% isopropyl alcohol) and put on sterile gloves. 5. With the pulp of your fingers, assess the size, depth, direction and point of maximum pulsation. 6. Holding the syringe like a pen bevel upwards at 45 degrees aim at the point of maximum pulsation, in a proximal direction Advantages – lies close to the surface, easily accessible, easy aseptic approach Disadvantages – end artery, pulse may be hard to feel in shut down patients or in patients with atrial fibrillation Brachial Site Collection 1. Position the arm so the medial aspect of the antecubital fossa is easily accessible. 2. Clean the skin with antiseptic solution and don sterile gloves. 3. Feel for the pulse assessing size, depth, direction and point of maximum pulsation. 4. Holding the syringe at 45 degrees aim at the point of maximum pulsation in a proximal direction. Advantages – can lie close to the surface, easy aseptic approach, easily compressible Disadvantages – end artery, quite mobile, close proximity to the nerve. Femoral Site collection 1. Make sure the patient is lying flat. 2. Clean the skin with antiseptic solution and don sterile gloves. 3. Place fingers on the femoral pulse. 4. Aim the needle at the point of maximum pulsation, distal to your fingers at almost 90 degrees to skin. 5. Slowly advance the needle whilst pulling back on the plunger until flashback is achieved. Advantages – reliable position, good landmarks, can take other bloods at the same time, can be found in shut down patients with poor or no pulses Disadvantages – Dirtier area of the body, may dislodge plaque in PVD All site considerations 1. When you enter the artery, the needle should self-fill; if not keep the needle still and pull back on the plunger. 2. Collect 1-2 ml of blood. 3. Withdraw needle and compress with cotton wool. 4. Discard needle (into sharps bin), expel the air and place the cap on the end. 5. Invert several times and take swiftly to the ABG analyser. Results interfering factors Drugs that cause an increase in HCO3Drugs that cause an increase in PaCO2 Drugs that cause a decrease in HCO3Drugs that cause a decrease in PaCO2 Bleeding disorders Recent blood transfusion Specimens with extreme high WBCs Specimens after change in inspired O2 Specimens after suctioning Excessive difference in actual body temperature Falsely increased O2 saturation Excessive heparin amount Used of citrates as anticoagulant Air bubbles or blood clots in specimen Delayed ice slurry placement Teach breathing exercises Administer O2 Teach about incentive spirometer Instruct to breathe deeply Water balance needs to be monitored Reinforce information regarding further testing Electrocardiogram A standard 12-lead ECG uses a series of electrodes placed on the extremities and the chest wall to assess a patient’s heart from 12 different views (leads) P wave and PR interval The p wave represents atrial depolarization. The PR interval represents the time it takes an impulse to travel from the atria through the atrioventricular nodes and the bundle of His Nursing Responsibilities Pre-procedure Inform patient about the test Obtain history of complains History of respiratory function Note recent procedures Obtain lists of medications Record temperature Indicate type of O2 used Perform allen test if site is radial artery Review and explain procedure Inform collection takes 10-15 minutes No restrictions on food and fluids unless directed Prepare ice slurry in a cup Intra-procedure Care is taken if patient is allergic to latex Instruct to cooperate and follow Observe standard precautions Results are manually or computerized system Post-procedure Applies pressure to site 5 minutes Observe for s/sx of respiratory reactions P wave – atrial depolarization no more than 3 boxes Rate, regularity, resemblance 10 x number of p wave in a 6 seconds strip = rate P-R interval – time that the signal took from sinus node to atrioventricular node 3-5 boxes (0.12 – 0.20) P-R segment – should be isoelectric (no depression and elevation) represents the time that the atrioventricular node blocks the conduction (gatekeeps it) no more than 3 boxes Could indicate that there is a heart block if it takes too long. QRS interval – ventricular depolarization and atrial repolarization 3 boxes T -wave – ventricular repolarization J point, S-T segment – finishing of ventricular depolarization Q-T interval – time of conduction to ventricular repolarization 0.35 – 0.44 seconds Atrial Fibrillation Atrial Flutter Ventricular fibrillation Ventricular tachycardia Supraventricular tachycardia