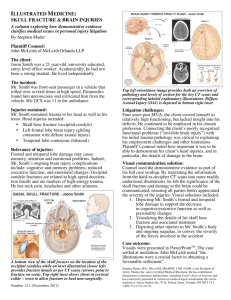
Definition: Birth injuries is defined as the injury that occurs during the birth of baby due to prolonged labor, mal presentation and the instrumental delivery such as: vacuum and forceps delivery. Forceps Forceps Forceps application Common new born injuries I. Skull injuries II. Soft tissue injuries III. Nerve injuries IV. Fracture bone I. Skull injuries: The injury that occurs in meninges, brain and great cerebral vein during the labor while passing through the birth canal is known as skull injuries. It may be caused by instrumentation such as forceps, vacuum and prolonged labor. Result of skull injuries the child may survive with impaired physical and mental states. Etiological factors: • Instrumental delivery such as vacuum, forceps delivery. • Excessive stretching in moulding. • Excessive compression of fetal head due to contracted pelvis, occipito- posterior position and large baby. • Rapid compression on fetal head: Breech delivery, precipitate labor. Etiological factors: • Upward compression as in breech delivery, face presentation. • Preterm baby because of lack of protection by their soft skull bones and wide suture as well as delicacy of the cerebral vessels and tissue, so they are prone to intracranial injuries. a) Caput succedaneum: • While the head descends to press over the dilating cervix, the over lying scalp is free from pressure, but the tissues in contact around the scalp is compressed. • This interferes with venous return and lymphatic drainage in the area of scalp, stagnation of fluid occurs. • Caput usually occurs after rupture of the membrane. Contin….. Caput succedaneum Causes • Friction between the fetal skull and maternal pelvis during the delivery. • Cephalo-pelvic disproportion ( by compression of bony pelvis) • Precipitate labor • Tearing of periosteum • Prolonged pressure on the head Clinical manifestation • Soft, puffy swelling of part of the scalp in a new born, present at birth. • Swelling may or may not have some degree of discoloration or bruishing. • Cross the suture line • Diffuse, pits on pressure • A caput is always unilateral. • Baby experience some discomfort so gentleness is needed while caring and handling. • Tends to decrease in size after delivery. • Resolve by 24 – 48 hours of life with no longer consequences. Diagnosis • A physical examination will confirm that the swelling is a caput succedenum. • No testing is necessary. Nursing Management • Provide explanation about the condition in very simple way. • Advise the mother to handle the baby very gently and apply dressing in abrasion if needed. Complication • Jaundice – results as the bruise breaks down of Red blood cells into bilirubin. Cephalhematoma • It is caused by the friction between the skull and pelvis during delivery. • The swelling with cephalhematoma is not present at birth rather it develops within the first 24 to 48 hours after birth. • The swelling is limited by the suture line of the skull. • It can cause hyperbilirubinemia when extensive, the infant need blood transfusion. Causes • Cephalopelvic disproportion • Precipitate labor • Tearing of the periosteum • Prolonged pressure on the head • Friction between fetal skull and maternal pelvis. Clinical features • Swelling of the infant’s head 24-48 hours after birth and enlarge slowly in the few days after birth. • Discoloration of the swollen site due to presence of coagulated blood. • It is circumscribed, soft fluctuant and incompressible • Present bilateral • Fracture of skull • Swelling may persists for weeks usually 6-8 weeks. Management • No treatment is necessary • The blood is absorbed and the swelling subsides within 6-8 weeks of infant's life. • Advise not to compress on affected region. Caput Succedenum Cephalohematoma Condition marked by localized soft tissue edema with poorly defined outline Condition marked by soft, fluctuant, localized swelling with well-defined outline Caused by pressure of the fetal head against the cervix during labor, which decreases blood flow to the area and results in edema Caused by subperiosteal hemorrhage Present at birth; does not increase in size Appears after birth; increases in size for 2–3 days Swelling crosses suture lines Swelling does not cross suture lines Disappears after birth within a few hours to several days Disappears from several weeks to even months after birth Complications are rare Complications include defective blood clotting, underlying skull fracture or intracranial bleeding, and jaundice c. Scalp injuries • Minor injuries of scalp such as abrasion in forceps delivery (tip of the blade), incised wound inflicted during caesarean section or episiotomy may be met with. • On occasion the incised wound may cause hemorrhage and requires stitches. • The wound should be dressed with an antiseptic solution like: 2 % mercurochrome and antibiotics ointment. 2 % mercurochrome d. Fracture skull: • Fracture of the vault of the skull (frontal or anterior part of the parietal bone) may be of linear or depressed type. • Causes: • Effects of difficult forceps delivery in disproportion or due to wrong application of the forceps (blades not placed over the biparietal diameter. • Projected sacral promontory of the flat pelvis may produce depressed fracture even though the delivery is spontaneous. Skull Fracture Clinical features: • The fracture may be associated with cephalhaematoma, extradural or subdural hemorrhage or a hematoma. • Fracture sometimes causes pressure symptoms (swelling). • Neurological manifestation may occur later on due to compression effect. Treatment: • Treatment is conservative. • In severe case aspirated or excised surgically Figure Tentorium tear • Tentorium: The cerebellar tentorium or tentorium cerebelli is an extension of the dura mater that separates the cerebellum from the occipital lobes. • Due to excessive molding, • Vacuum cup there is compression of the engaging diameter and elongation of the diameter, that put too much strain on the muscles fibers and tentorium tear occurs. Clinical features • Baby is delivered still born • Respiratory depression • APGAR is 0-3 • Frequent high pitch cry • Neck retraction • In co-ordination ocular movements • Convulsion • Vomiting and • bulging of the anterior fontanel Treatment and management • The baby should be nursed in quiet surroundings. • Baby should be provided humidified oxygen. • Maintain cleanliness of the air passage. • Restrict handling the baby such as bathing, weighting and measuring should be withheld. • Nasogastric tube feeding is advisable. Treatment and management • Fluid balance should be maintained. • Administered vitamin K intramuscularly to prevent further bleeding due to low thrombin level in blood. • Administer prophylactic antibiotics. • Anticonvulsant is given to prevent convulsion. Soft tissue injuries • Bruises and lacerations on the face are caused by forcep blades. These are treated with application of antibiotics ointments. Injury by application of forceps Muscles: • Sternocleidomastoid ( SCM) injury : Injury is characterized by a well – circumscribed immobile mass in the mid point of the sternocleidomastoid. The head tilts towards the involved side. • The patient cannot move the head normally. Head is twisted to one side (Torticollis). • This occurs during delivery of the anterior shoulder in a vertex presentation or while rotating the shoulder during a breech delivery. Muscles: • It usually presents 1 or 2 weeks after birth as small painless lump of 2 cm on the side of the neck. • The swelling will resolve over several weeks. • Muscles – stretching exercise should be taught to parents to prevent from shortening of muscles. • Infants should sleep on the opposite side to the injury to increase passive stretching. Sternocleidomastoid hematoma: • This appears about -10 days after birth and is usually situated in the mid- position of the muscle fibers. • It is caused by rupture of the muscle fibers and blood vessels, followed by a hematoma and contraction. • It may be associated with difficult breech delivery or attempted delivery following shoulder dystocia or excessive lateral flexion of the neck even during normal delivery. There is transient torticollis . Management • Management is conservative. • Stretching of the involved muscles should be done several times a day. • Recovery is rapid (3-4 months) in majority of cases. • Surgery is needed if it persists after 6 months of physical therapy. Necrosis of the sub-cutaneous tissue • This occur while the superficial skin remains intact. After a few days, a small hard subcutaneous nodule appears. It is the result of the fat necrosis due to pressure, and takes 14-16 weeks to disappear. Management • No treatment is required and it has no clinical importance. Necrosis of the sub-cutaneous tissue Nerve injuries: • 1.Facial palsy • 2. Brachial palsy • a. Erb's palsy: Upper brachial palsy • b. Klumpke's palsy: Lower brachial palsy Facial palsy ( peripheral) • The facial (7th) nerve remains unprotected after its exists through the stylomastoid foraman. Causes: • It is caused by direct pressure of the forceps blades or by the hemorrhage and edema around the nerves. • Direct pressure on the ramus of mandible. Stylomastoid foraman Fig… of Ramus Clinical features of facial palsy • Unilateral facial weakness • The eyelid of the affected side remains open while mouth is drawn over to the normal side. • Paralyzed side is smooth. • On crying, the mouth is drawn to the un-injured side of the face. • Sucking remains affected. Facial ….. • Diagnosis: It is made by noting the eye of the affected side which remains open and fixed. • Treatment and management: • Protect the eyes, which remains open during the sleep. • The condition usually disappear within weeks unless complicated by intracranial damage. • Maintain oral hygiene. • If injury due to instrumental delivery dressing should be applied on injury area. • Apply antibiotic if injury is serious. Brachial palsy • The brachial plexus is a network (plexus) of spinal nerves (formed by the anterior rami of the lower four cervical nerves • (C5 (bending of elbow) C6 (helps in wrist extension) C7 (elbow straighten), C8 ( hand finger flexion) , and T1 ( chest wall, arm and hand). Brachial palsy • Either the nerve roots or the trunk of the brachial plexus are involved. • The damage of the nerve is due to stretching (common) or effusion or hemorrhage inside the sheath. Tearing of fibers is rare. • Causes: • Undue traction on the neck during the shoulder dystocia. • Treatment • Immobilization and prevention of the contractures. • Physical therapy and passive movements are advocated. • Full recovery takes weeks or even months. • X- ray, MRI should be done a. Erb's palsy( Waiter tips position) • This is the most common type when 5th and 6th nerve root are involved. • The resulting paralysis causes the arm to lie on one side (adducted) with extension of the elbow, pronation of the forearm and flexion of the wrist. Winging of the scapula is common. • Moro reflex is absent. Erb’s Palsy Causes • When the neck is twisted or stretched in delivery of the baby in after coming head in breech presentation. • Excessive lateral flexion of the neck when delivering the shoulder in vertex presentation and forceps delivery. • Treatment : • The treatment consists of use of splint so as to hold the affected arm . • Passive movement should be advocated. • If condition is fatal surgical intervention is needed. b. Klumpke's palsy • This type of palsy is due to affection of the lower cord of the plexus involving 7th and 8th cervical or even the first thoracic nerve. Affects in the movements of hand • Clinical features: • The arm is flexed at the elbow, the wrist extended. • The forearm is supinated and a claw-like deformity of the hand is observed. • When is involved, there may be homolateral ptosis ( drooping of upper eye lids) with small pupil due to sympathetic nerve involvement( Horner's syndrome). Treatment of klumpke’s palsy Treatment: • Immobilization and prevention of the contractures. • Physical therapy and passive movements are advocated. • Full recovery takes weeks or even months. • Surgical is recommended in severe cases. Fractures • The most commonly affected bones are those of the skull, clavical, humerus, femur and spine. a. Clavicle: Fracture can occur if there is shoulder dystocia or during a birth by the breech. The affected bone is usually the one, which is nearest the maternal symphysis pubis. It is possible to feel a distortion in the bone and crepitus formation during an examination. Fracture… b Humerus: Mid-shaft fractures can occurs during a birth by breech when extended arm is brought down and born. Considerable deformity is evident on examination and the baby will be reluctant to move the arm owing to the pain. c. Femur: Mid –shaft fractures can occur during a birth by the breech when the extended legs are brought down and born. Considerable deformity is evident on examination and the baby will be reluctant to move the leg owing to the pain. Treatment • In clinical fracture, a pad of cotton or wool is placed in the axilla and the upper arm is lightly bandaged to the side of the chest. • In fracture femur, the whole length of the affected limbs may be bandaged cast. • Healing usually occurs in about 3 weeks. •Thankyou