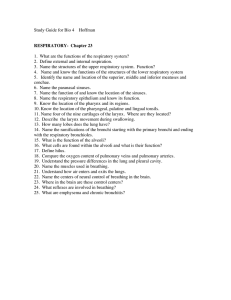
Oxygenation 1. What is the definition of Oxygenation? Is Ventilation, gas exchange, and transport of gases by which cellular oxygen supply is maintained. 2. What are the major mechanisms of Oxygenation? Pulmonary system- lungs breathing/ventilation, gas exchange in alveoli Kidneys-erythropoietin-RBCs Heart-pumps/distributes blood (O2 on RBCs) Brain- CO2 (35-45) and PH levels stimulate Medulla (brain) and other receptors stimulating us to take a breath 3. What part does respiratory system play in oxygenation process? Pulmonary system- breathing/ventilation, gas exchange in alveoli 4. Name anatomical structures of respiratory system and their functions Nose-airway (inhale/exhale) Mouth-airway (inhale/exhale) Throat (pharynx) carries air from nose and mouth Voice box (larynx) lets air pass from throat to trachea on the way to lungs Windpipe (trachea) carries O2 rich air to the lungs Large airway (bronchi) carries air to and from lungs Small airway (bronchioles) carries air into the small alveoli sacs Lungs (expand and deflate) 5. What are the mechanisms of regulation? CO2 level 35-45, neutral blood PH 7.35-7.45, breathing (active vs. passive) 6. What are the normal adaptation processes of the respiratory system? Automatic hemostatic (regulator)Elevated CO2 levels, mucus and cilia traps & remove foreign particles), and cough Voluntary (cognator)- Voluntarily take a deep breath and cough, coughing and breathing exercise to regulate respirations and cough intensities 7. When does the adaptation process becomes compromised? Respiratory or cardiac cannot provide the O2 demands of the body, or demands are too high 8. List 1st level assessment findings 02 deficiency 1st levelchange in LOC, behavior (decreased alertness, confusion, lethargy), visual acuity, chest pain , nasal flaring (indicative of severe respiratory distress), accessory muscle use, ((ineffective adaptations such as anxiety, emotional distress, gasping, tripoding (leaning in for air), pushing away O2 mask, fish out of waterflustered)), Resp patterns (normal 12-20/min)—Tachypnea >24/min (fast breathing), Bradypnea <10/min, Apneano breathing, lung sounds, diminished breath sounds (no ventilation), crackles, wheezing, secretions (normal is clear, watery, no blood/odor), exercise tolerance r/t exercise. 9. List 2nd level assessment findings 2nd level for O2 deficiency- Obstruction, pleural effusion, cancer, thoracic deformities, muscular dysfunction, respiratory center dysfunction, asthma, smoking, infection, COPD, etc. Gas exchange 2nd level-tissue damage, bronchitis pneumonia, emphysema, inadequate circulation to alveoli Other 2nd level affecting O2- stress, pain, anxiety, exercise, dietary habits, increased metabolic need (fever/pregnancy), Medications (bronchodilators, cardiac drugs), smoking, knowledge of respiratory, Cardiovascular health, environmental factors 10. List nursing diagnoses for respiratory component of ineffective oxygenation Nursing diagnosis: Ineffective breathing pattern 2nd level assessments: Thoracic deformity, abdominal distension, surgery, prolonged bedrest, asthma Nursing diagnosis: Impaired gas exchange 2nd level assessment: Pneumonia, emphysema, CHF, Pulmonary TB Nursing diagnosis: Risk for altered respiratory function 2nd level assessment- Prolong bedrest, post stroke, history of smoking, etc Nursing Diagnosis: Ineffective Airway clearance (always priority)** (e.g of PESIneffective airway clearance related to pulmonary secretions, E/B or M/B SOB (secretions of bronchi, cough, wheezing) 2nd level assessment- obstruction, post-thyroid surgery, post-surgical pt, post CVA, Tracheostomy, use of anesthesia, blood, tumor, food stuck, etc Nursing diagnosis- Activity intolerance 2nd level assessment- anemia, CHF or cardiac disease, respiratory disease (emphysema/ asthma) 11. List nursing interventions for respiratory component of ineffective oxygenation **Maintain Airway-Priority intervention for ineffective airway**, dyspnea mgt (meds, dilators), deep breathing/coughing exercises, O2 therapy, Promote removal of secretions via humidification and nebulization, pt education on fluids, adequate hydration, panned rests/walks, cardio-pulmonary reconditioning (rehab); Maintain ventilation via suctioning, implement artificial airway, chest tube (below bed level so gravity can assists w/ drainage/secretions). *Position pt on opposite side for altered ventilation (if pt has right side pneumonia, place them on left, vice versa) Note: **2L nasal cannula SAFEST dose/amt of O2** Nasal cannula-check for pressure injury behind ears 12. List evaluation criteria for respiratory component of ineffective oxygenation? (Goals=behavior +change +timeframe) Changes in vital signs, changes in subjective complaints, changes in appearance (skin, color, moisture, mucous membranes), changes in activity level, reports of fatigue. Sputum, lung sounds, respiratory rate b/w 18-24, pt able to clear airway secretions, pt’s spO2 is 92, ABG’s, O2 Sat 95-100%