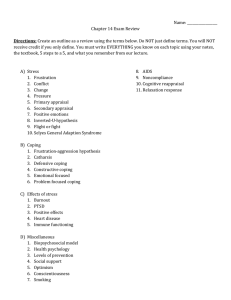
Personality and Individual Differences 186 (2022) 111351 Contents lists available at ScienceDirect Personality and Individual Differences journal homepage: www.elsevier.com/locate/paid Coping, social support, and family quality of life for caregivers of individuals with autism: Meta-analytic structural equation modeling Ruodan Wang a, Qing Liu a, *, Wenjuan Zhang b a b College of Education and Technology, Zhejiang University of Technology, Hangzhou, China Mental Health Education Center, Xidian University, Xi'an, Shaanxi, China A R T I C L E I N F O A B S T R A C T Keywords: Caregivers of individuals with autism Coping Social support Family quality of life Meta-analysis This study used the meta-analysis structural equation modeling (MASEM) method to explore the relationship between coping (positive and negative), social support, and family quality of life for caregivers of individuals with autism. Through a meta-analysis of 29 studies (N = 4864), the following results were found: (1) Positive coping by caregivers significantly positively predicted social support (β = 0.27) and family quality of life (β = 0.12). Negative coping significantly negatively predicted social support (β = − 0.18) and family quality of life (β = − 0.18). The social support of caregivers significantly positively predicted family quality of life (β = 0.30). (2) Positive coping and negative coping by caregivers had significant indirect effects on their family quality of life through social support (β = 0.08, β = − 0.05, respectively). It can be seen from the results that social support of caregivers of individuals with autism partially mediates the relationship between coping (positive and negative) and family quality of life. In addition, the results of the moderator analyses showed that caregivers with spouses were more likely to reduce social support when they adopted negative coping than caregivers without spouses (p = .022). 1. Introduction Autism spectrum disorder (ASD) is an early neurodevelopmental disorder characterized by social communication deficits, language development disorders, an intense preoccupation with a narrow range of subjects, and stereotypic behavior (American Psychiatric Association, 2013). In addition, the external manifestations of ASD are complex, including sleep problems, aggression, hyperactivity, self-injury behavior, impulsive behavior, and (lower or higher) sensitivity to stimuli. The problem behaviors of children with ASD have brought great challenges to their caregivers (usually parents). In the caring process, caregivers of individuals with ASD face pressure and difficulties from employment, financial crisis, alienation, irregular life, social stigma, and mental and physical exhaustion, which greatly reduce their family quality of life (FQOL) (Stanojević et al., 2017; Weiss et al., 2014). In 1983, some researchers proposed a double ABCX model for the adjust­ ment and adaptation of families facing stressors (Fig. 1), in which family adaptation (xX) is affected by the pile-up of demands (aA), adaptive resources (bB), family perception (cC), and coping (BC) (McCubbin & Patterson, 1983). Many studies have found that various predictors of FQOL and family adaptation are consistent, such as children's behavioral problems, social support, coherence, and mental health (McStay et al., 2015; Predescu & Şipoş, 2017). The double ABCX model can be suc­ cessfully applied to the study of FQOL in caregivers of people with ASD after continuous revision. The revised double ABCX model consists of four parts (aA stressors, bB external support, cC appraisal and coping, and xX family adaptation). Specifically, stressors, external support, appraisal, and coping all directly affect the FQOL, and external support, appraisal, and coping play a moderating role in the process of stressors affecting the FQOL (*Meleady et al., 2020). Some studies based on the double ABCX model found that coping and social support of caregivers of individuals with ASD have a significant predictive effect on their FQOL (*Ji et al., 2014; Ghanimi et al., 2018; Mourya & Singh, 2016), where positive coping is significantly positively correlated with social support and FQOL, and negative coping is significantly negatively correlated with social support and FQOL (*Cappe et al., 2018; *Lin et al., 2011). However, some studies have found that the correlation between positive coping and FQOL is not significant (*Pozo et al., 2014). Moreover, the correlation between negative coping and social support was not significant (*Khanna et al., 2011). Currently, there are few studies on the mediating role of social support for caregivers in coping with FQOL. At the same time, the results * Corresponding author at: Zhejiang University of Technology, Hangzhou 310014, China. E-mail address: psylq@zjut.edu.cn (Q. Liu). https://doi.org/10.1016/j.paid.2021.111351 Received 21 August 2021; Received in revised form 5 October 2021; Accepted 15 October 2021 Available online 23 October 2021 0191-8869/© 2021 The Authors. Published by Elsevier Ltd. This is an open (http://creativecommons.org/licenses/by-nc-nd/4.0/). access article under the CC BY-NC-ND license R. Wang et al. Personality and Individual Differences 186 (2022) 111351 related quality of life and well-being. Social support can be used as a potential intervention point to alleviate the inner pain of caregivers, and it has a significant impact on the satisfaction of FQOL (Garrido et al., 2020). At present, meta-analyses of the relationship between social support and FQOL for caregivers of people with ASD are rare. Schiller et al. (2021) showed through a meta-analysis that different types and sources of social support have a protective effect on caregivers' mental health. This study will use a meta-analysis to illustrate the impact of social support as a mediator variable on the FQOL for caregivers of children with ASD in the structural equation model. of the relationships between existing variables are also different. Therefore, it is necessary to discuss the relationship between the coping, social support and FQOL for autistic persons' caregivers, as well as whether there is a mediating and potential moderator effect among them. 1.1. Does social support of caregivers of ASD affect their family quality of life? Family quality of life (FQOL) refers to the degree to which family needs are met, the time that family members enjoy life together, and the opportunity to do things of great significance to the family together (Park et al., 2003), including physical and mental health, family inter­ action, nurturing, and support related to disability (Hoffman et al., 2006). Studies have shown that the quality of life of parents of children with ASD is lower than that of parents of normally developing children, and the parenting burden of mothers with children who have ASD is greater than that of mothers of normally developing children (Wang et al., 2018). Caregivers of autistic children are more likely to experience psychological distress and lower quality of life (Bromley et al., 2004; Pastor-Cerezuela et al., 2021). In general, although the improvement of caregivers' FQOL is helpful for the treatment and rehabilitation of per­ sons with ASD (Ghanimi et al., 2018), this group's material life, physical function, psychological function, and social function are significantly lower than those of normal developing children's parents (Perumal et al., 2014). At the same time, their emotional health satisfaction is even lower than other aspects of FQOL (Schlebusch et al., 2017; Smith, 2018). Marsack and Samuel (2017) explained the importance of support from social relationships to the happiness, health, and FQOL of caregivers of ASD. Social support refers to individuals who feel the care, love, and respect provided by the social network and receives the help provided by the social network (Cobb, 1976). Social support can generally be divided into formal and informal support. Formal support usually refers to the support that needs to be paid for, such as support from health care in­ stitutions, rehabilitation centers, etc.; informal support usually refers to the support obtained without compensation, such as support from peers, religious groups, friends, and family (Ault et al., 2021). In the context of collectivist culture, mothers of autistic children report higher stress levels than mothers of healthy children (Ueda et al., 2020), but the combination of formal and informal support is of greater help to their families (McIntyre & Brown, 2018). Many studies have shown that social support has a positive effect on improving the FQOL of caregivers of individuals with ASD (BishopFitzpatrick et al., 2018; Ekas et al., 2016; Lei & Kantor, 2021; Obeid & Daou, 2015). McGrew and Keyes (2014) found that perceived social support can buffer the impact of stress on individuals, reduce the burden and depression level of caregivers of ASD, and improve their health- 1.2. Does coping of caregivers of ASD affect their social support? Coping refers to the use of cognitive and behavioral efforts to control, tolerate, and reduce internal and external needs and conflicts generated by stressful situations (Folkman, 1984). The coping style is similar to the coping strategy, which is the specific form of coping and refers to the main behavior mode and reaction state tendency adopted by individuals in facing the stress process (Craig et al., 2020; Spady, 1993). Different studies divide coping in different ways (Algorani & Gupta, 2021). The most common division is currently split into two dimensions: problemfocused coping and emotion-focused coping (Benson, 2010; Bozkurt et al., 2019). Problem-focused coping is generally seen as adaptive behavioral tendency, which produces more positive results than emotion-focused coping (*Khanna et al., 2011). Emotion-focused coping is considered as a maladaptive behavior tendency (Herman & Tetrick, 2009). Adaptive and maladaptive coping are usually regarded as posi­ tive and negative coping, respectively (Ward et al., 2021). Positive coping includes active responses, planning, active reconstruction, acceptance, humor, religion, the use of emotional support, and instru­ mental support, while negative coping includes self-distraction, denial, venting, substance abuse, behavior disengagement, and self-blame (Meyer, 2001). Brown et al. (2020) have shown that the avoidance dimension in negative coping is related to higher stress levels of parents of children with ASD, and positive coping is related to lower levels of depression. According to them, in terms of marital satisfaction, female caregivers tended to benefit more than male caregivers in positive coping. Lai et al. (2015) found that parents of children with ASD are more likely to adopt maladaptive coping than parents of normally developing children. Regarding the relationship between coping and social support, China's research and analysis has concluded that coping has a significant predictive effect on social support (a mediator variable) in the process of influencing mental health, with an effect coefficient of 4.887 (Jing et al., 2017). Positive coping dimensions such as seeking social support and being action-oriented are significantly positively correlated with the support index, while negative coping dimensions such as avoidance are Fig. 1. The double ABCX model of family adjustment and adaptation (McCubbin & Patterson, 1983). 2 R. Wang et al. Personality and Individual Differences 186 (2022) 111351 significantly negatively correlated with the social support index (*Whitehead et al., 2015). However, some studies on the relationship between the two have shown that some positive or negative dimensions of coping are not significantly associated with social support (Novara et al., 2015). Therefore, given the inconsistency of the research results, this study used a meta-analysis based on the structural equation model to explain the relationship between the two variables. status” as a moderator variable to observe whether it has an impact on the relationship between caregivers' coping, social support, and FQOL. 1.4.3. Sex of caregivers Mothers of children with ASD are more likely to use emotion-focused coping than fathers, which will increase their depression and anxiety problems and become one of the factors that reduce their FQOL (Dab­ rowska & Pisula, 2010; Meral et al., 2013). In contrast to the above conclusions, Ghanouni and Hood (2021) concluded in their article that there is no significant difference in coping ability between mothers and fathers of children with ASD, and mothers will use more support from family, friends, and spouses. This type of support tends to improve family happiness. In response to the above different views, this article will incorporate “sex of caregivers” into the potential moderator variables. 1.3. Does social support of caregivers of ASD mediate the relationship between coping and family quality of life? Stuart et al. described that positive coping could reduce the burden on all levels of the family system, and that negative coping has a negative effect on individual stress levels, and physical and mental health (Stuart & McGrew, 2009). Numerous studies have also discovered the importance of adopting positive coping for caregivers, which is related to increased happiness and decreased depression (McKee et al., 2020). According to Tajrishi's experiment, some scholars have concluded that the use of positive dimensional problem-focused coping strategies by caregivers of individuals with ASD can significantly improve their quality of life (Lovell & Wetherell, 2015; Pourmohama­ dreza-Tajrishi et al., 2015). According to the amended double ABCX model (*Meleady et al., 2020), coping and social support have a direct effect on FQOL, and they play a moderating role in the process of stressful events faced by care­ givers. As to whether social support acts as a mediator variable between coping and FQOL, some research supports this view. Social support has been found to play a mediating role in the relationship between coping and mental health (Jing et al., 2017), while other studies are mostly regression analyses about coping and social support of caregivers of people with ASD on FQOL. For example, Khanna et al. (2014) believe that caregivers fully perceive support from friends and family, and adopting positive coping will lead to higher FQOL. In general, in view of the unclear mediating role of caregivers' social support on the impact of coping on FQOL in previous studies, this article will further confirm this. 1.4.4. Age of persons with ASD Kousha et al. (2016) found that the age of autistic children strongly affects their mothers' mental health and quality of life. According to them, the older the children, the worse the parents' ability to use reasonable coping strategies and useful external resources, and the more obvious symptoms of anxiety and depression. However, some studies have shown that the FQOL perceived by caregivers of autistic in­ dividuals is unrelated to their age (Dardas & Ahmad, 2014; Robinson & Weiss, 2020). This may be caused by poor coping strategies and social support that did not meet the needs and expectations of these families. Based on the inconsistency of some research results, this article will use the “age of persons with ASD” as a moderator variable to explore its influence on the variables in the structural equation. 1.4.5. Family financial status Through research, some scholars believe that family income affects the satisfaction of children with ASD. If there is no satisfaction, it dis­ rupts family life order and increases the stress of caregivers, thus reducing FQOL (*Cappe et al., 2018; Alenazi et al., 2020; Alhazmi et al., 2018; Omar et al., 2017). Gagat-Matula (2021) also supports this view. In his research, he found that compared with families with ordinary economic conditions, families with poorer finances prefer to adopt emotion-focused coping, lack vitality in seeking social support, and thus have a lower quality of life. However, some studies have pointed out that the social support received by families of individuals with ASD is not affected by financial status, which may be due to the lower cost of available support (Al-Tal et al., 2021). Therefore, in view of the different results of different studies on family financial status, this study will incorporate it into potential moderator variables to explore its impact. In summary, current research on the mediating role of social support between coping and FQOL is still unclear, and the results of the rela­ tionship between the two are still controversial. Therefore, this research will use the meta-analysis structural equation modeling (MASEM) method to explore the relationship between coping (positive and nega­ tive), social support, and FQOL for caregivers of individuals with ASD, and whether social support has a mediating effect on the pooled sam­ ples. If there is a mediating effect, what is the specific impact mechanism of the mediating effect? Do potential moderator variables affect the relationship between the three? Specifically, the hypotheses of this meta-analysis are as follows: 1.4. Do moderator variables affect the relationship between coping, social support, and family quality of life of caregivers of individuals with ASD? We considered several potential moderator variables that affect the relationship between variables in the structural equation model, including caregivers' age, marital status, sex of caregivers, age of persons with ASD, and family financial status. 1.4.1. Age of caregivers Studies have shown that as the age of parents increases, the fre­ quency of positive coping strategies decreases (*Salas et al., 2017). The use of negative coping strategies that accompany the above situation is a risk factor for quarrels in families, which can lead to social isolation and is detrimental to the FQOL (Vernhet et al., 2019). However, Schlebusch et al. (2017) found that regardless of the age of fathers or mothers, it does not affect disability-related support and does not affect the FQOL. In view of this, we will examine whether the “age of caregivers” affects the relationship between coping, social support, and FQOL. 1.4.2. Marital status The partner effect will influence fathers to adopt distracting coping strategies (negative), and avoiding social support and responsibilities, which makes mothers take on more challenges and subsequently have a poorer quality of life (Özgür et al., 2018; Wang et al., 2020). McAuliffe et al. (2017) compared married mothers and single mothers and found that although single mothers have a lower quality of life in the envi­ ronmental field, there is no difference in the physical, psychological, and social relations fields. Single mothers use more adaptive coping (acceptance), which is a positive coping style. From the above, based on the diversity of the research results, this article will include “marital 1) Positive coping of caregivers of individuals with ASD has a signifi­ cant positive impact on social support, while negative coping has a significant negative impact on social support. 2) Positive coping of caregivers of individuals with ASD has a signifi­ cant positive impact on FQOL while negative coping has a significant negative impact on FQOL. 3) The social support of caregivers of individuals with ASD positively predicts their FQOL. 3 R. Wang et al. Personality and Individual Differences 186 (2022) 111351 4) Social support plays a mediating role in the relationship between coping (positive and negative) and FQOL. 5) The relationship between coping, social support, and FQOL for caregivers of individuals with ASD was not affected by the potential moderator variables (age of caregivers, marital status, sex of care­ givers, age of persons with ASD, and family financial status). 1997) is mostly used; for the mediating variable “social support”, the Multidimensional Scale of Perceived Social Support (Zimet et al., 1988) is more used; for the dependent variable “family quality of life”, the WHOQOL-BREF (Whoqol Group, 1995) and the Beach Center Family Quality of Life Scale (Hoffman et al., 2006) are often used. The specific data collection for the above variables comes from cross-sectional studies. 2. Methods 2.1. Participants 2.3. Procedure After screening literature (see “Section 2.3. Procedure” for details), a total of 4864 caregivers of autistic persons were pooled. Most caregivers were recruited from special schools, clinics, and the Internet. The diagnosis of their children's autism was confirmed by authorities. In the collected samples, the age of caregivers ranged from 35.22 to 47.49 years (M), the married rate exceeded 50%, female caregivers accounted for more 50% (ranging from 50% to 100%), and the age of autistic persons ranged from 3.24 to 18.04 years (M). The research process of this meta-analysis has been approved by the local ethics committee and conforms to the ethical standards of the Helsinki declaration. 2.3.1. Literature search We used the electronic databases Web of Science, PsycINFO, PubMed, and MEDLINE to conduct literature searches. The date of the last search ended on June 15, 2021. Specifically, the search terms' combination for caregivers of ASD was set as autis* OR asperger OR ASD, and care* OR parent* OR mother* OR father*, the search term for coping was set as coping, the search terms' combination for social sup­ port was set as social support OR society support, and the search terms' combination for FQOL was set as quality of life OR living quality. 2.3.2. Inclusion and exclusion criteria The literature search and screening process followed the PRISMA guidelines (Moher et al., 2009); the specific process is shown in Fig. 2. We established the following criteria to determine whether studies should be included in the meta-analysis of structural equation modeling: on one hand, studies should quantitatively report effective information 2.2. Variables and instruments In the pooled research, for the independent variable “coping” of caregivers of individuals with autism, the Brief COPE scale (Carver, Fig. 2. PRISMA flow diagram. 4 R. Wang et al. Personality and Individual Differences 186 (2022) 111351 such as correlation coefficients and sample sizes about the relationship between the constructs (i.e., coping, social support, and FQOL of care­ givers of ASD); on the other hand, studies should simultaneously mea­ sure the relationship between the three variables, or coping (positive and negative) should be measured before other variables to ensure the accuracy of directions in the model. Studies that had nothing to do with the subject or caregivers of ASD were excluded; theoretical reviews, conceptual articles, or qualitative studies were excluded; non-English or non-Chinese literature was excluded; the best of different articles of the same data source were retained according to the quality after compar­ ison, and the others were eliminated. moderating effect to explain possible heterogeneity in this research (Jak & Cheung, 2020). Publication bias refers to the fact that studies with statistically sig­ nificant results are more likely to be published, resulting in small-study effects (Griffin et al., 2021). There are many ways to test publication bias, and the Egger test was used in this study (Egger et al., 1997). The Egger test, also called the Egger linear regression method, was used to test the degree of symmetry of the funnel distribution. If the test is sig­ nificant (p < .05), it means that the funnel is asymmetrical and there is publication bias (Yu et al., 2021). 3. Results 2.3.3. Selection and coding of studies Two authors discussed the relevant content of articles together during the selection process to determine whether the articles should be included in the meta-analysis. After that, the two authors separately coded and checked the information required for the selected articles. In the case of very few data deviations, the two authors made a final de­ cision after reviewing and discussing them. Each study was coded using Microsoft Excel spreadsheets according to the following sample char­ acteristics: author information, sample size, country of sample, publi­ cation time, measurement tools of variables, reliability of measurement tools, correlations between variables, sex of caregivers (the proportion of females), family financial status (the percentage of the lowest income level in a research), marital status (married rate), age of caregivers (average age of caregivers of individuals with ASD), and age of persons with ASD. This study collected 29 different studies from 28 articles, with a total of 4864 participants. The positive coping and FQOL (20 studies, n = 3046), negative coping and FQOL (16 studies, n = 2512), positive coping and social support (19 studies, n = 3351), negative coping and social support (16 studies, n = 3086), social support and FQOL (15 studies, n = 2703) were analyzed by MASEM, and a total of 106 effect sizes related to r were extracted. 3.1. Heterogeneity of structural equation model and test of mediation effect Table 1 shows the first-stage pooled correlation matrix based on the random effects model. After the heterogeneity test, the results showed high heterogeneity among the studies (Q test was significant and I2 was greater than 50%). The TSSEM results are listed in Table 2. Table 2 shows that the direct effects of the hypothetical structural equation model were all significant (confidence interval does not include 0). Positive coping with caregivers had a positive impact on social support and FQOL (β = 0.27, β = 0.12, respectively), while negative coping had a negative impact on social support and FQOL (β = − 0.18 and β = − 0.18, respectively). Increasing social support can improve FQOL (β = 0.30). In addition, positive coping of caregivers had a significant positive impact on their FQOL through social support (β = 0.08), and negative coping of caregivers had a significant negative impact on their FQOL through social support (β = − 0.05), showing that social support partially mediated the relationship between coping (positive and negative) and FQOL. Fig. 3 shows the assumed and verified the structural equation model. 2.3.4. Calculation of effect size This study used the Pearson correlation coefficient “r” as the effect size to analyze the strength and direction of the relationship between structural variables. If a study reports correlation coefficients between different dimensions of a variable and other variables, the mean value is taken as the final correlation coefficient index; when multiple mea­ surements are taken, the index of the first measurement is used (Deng et al., 2016; Roorda et al., 2011; Tehrani & Yamini, 2020). According to the above two previous experiences, combined with “Section 2.3.2. In­ clusion and exclusion criteria”, 28 full-text articles were included in the analysis, of which 29 were independent studies, and the total number of subjects was 4864. All included articles followed the relevant ethical standards. 2.3.5. Statistical analysis The data collected in this study was processed using the meta for package and meta SEM package in R (Cheung, 2014; Viechtbauer, 2010). Meta-analysis structural equation modeling (MASEM) was used to examine the relationships between variables and fit the structural equation model. To verify the mediating effect of a variable in the structural equation model, we used the two-stage method of metaanalysis structural equation modeling (TSSEM) proposed by Cheung and Chan (2005). In the first stage, the correlation coefficients of various studies were combined into a correlation matrix. In the second stage, a combined correlation matrix was used to verify the proposed structural equation model. Since the research data came from samples with different conditions, after considering sampling errors and different variations between studies (heterogeneity), we used the random effects model to draw more general conclusions. There are two methods for quantitative analysis of heterogeneity: Cochran's Q test, if it is significant, there is obvious heterogeneity (Cochran, 1954; Hedges & Olkin, 2014); the other is statistical value I2; specifically, I2's low-, medium-, and high- classification standards are 25%, 50%, and 75% (Higgins et al., 2003). The latter judgment of het­ erogeneity is currently more popular. The information characteristics of the moderating variables included in this study were all continuous variables. Therefore, we used one-stage meta-analysis structural equa­ tion modeling (OSMASEM) to test moderator variables to analyze the 3.2. Analysis of the moderating effect of a structural equation model OSMASEM was used to test the moderating effects of the moderator variables (age of caregivers, marital status, sex of caregivers, age of persons with ASD, and family financial status). After standardizing the moderator variables, this study analyzed whether they had any influ­ ence on all paths involved in the structural equation model. The results Table 1 Stage 1: pooled correlations (and I2) among the variables in the mediation based on the random effects model. Variable Positive coping Negative coping Social support Family quality of life Positive coping 1 20 (88.52%) 20 (83.22%) Negative coping Social support Family quality of life 0.06 1 0.26*** 0.18*** − 0.16*** − 0.22*** 19 (72.39%) 16 (75.92%) 1 0.36*** 16 (55.28%) 15 (77.30%) 1 Note. The upper diagonal of the matrix contains the number of studies involved in the analyses for each pair of correlation and homogeneity indices (I2). Each pair of correlations is listed in parentheses, and the lower diagonal of the matrix contains correlations among the variables in the mediation model. *** p < .001. 5 R. Wang et al. Personality and Individual Differences 186 (2022) 111351 increase their degree of social support, while adopting negative coping decreases their degree of social support (Hypothesis 1 is supported). This outcome further supports previous empirical research (Jing et al., 2017; Pisula & Banasiak, 2020; Ruiz-Robledillo et al., 2014; Schneider-Matyka et al., 2018). It is worth noting that despite their significant predictive power, positive coping has a stronger correlation with social support than negative coping. This may indicate that caregivers can obtain more social support from the outside world through positive strategies such as actively seeking help and cognitive reconstruction, thereby perceiving the availability and usefulness of the support they receive. However, by adopting negative coping strategies such as avoidance and disengage­ ment, caregivers feel fewer social support changes, and therefore the association is less. Second, both coping and social support have predictive effects on the FQOL of caregivers of people with ASD (Hypothesis 2 and Hypothesis 3, respectively, supported). By accepting the ASD's facts, looking for treatments, and adopting correct coping strategies (such as positive cognitive reappraisal and reasonable emotional venting), caregivers can improve the mental health aspect of the FQOL. Instead, negative coping strategies such as self-closure and avoiding reality will adversely affect their physical and mental health, thereby decreasing their overall quality of life. This result is consistent with the revised double ABCX model (*Meleady et al., 2020) and the conclusions drawn from previous studies (*Pyszkowska & Wrona, 2021; Chowdhury et al., 2019; Siah & Tan, 2016; Vaz et al., 2021). However, when Dardas and Ahmad (2015) studied the role of fathers' coping with ASD between parenting stress and quality of life, they found that coping had no significant impact on the father's quality of life. The reasons discussed may be due to factors such as male-related personal styles, family characteristics, and culture, which have led to weaker coping effects. Finally, when analyzing the constructed structural equation model, we found that social support plays a role in mediating the relationship between coping and FQOL (Hypothesis 4). This shows that coping of caregivers of individuals with ASD can indirectly impact their FQOL through social support. It can also directly impact FQOL, regardless of the impact of social support. The verification of this structural equation model further explores the double ABCX model (*Meleady et al., 2020; McCubbin & Patterson, 1983), which illustrates the relationship and influence path between coping, social support, and FQOL. Through analysis of the moderating effect, we concluded that marital status has a moderating effect on the model (Hypothesis 5 is not supported). Spe­ cifically, caregivers with spouses were more likely to reduce social support when they adopted negative coping strategies than caregivers without spouses. This may be because caregivers with spouses adopt a series of hostile emotional vents, escape, avoidance, excessive selfblame, and other negative coping, making the other one in the mar­ riage and closest family members more emotional (“one disaster after another”). Hence, this situation greatly reduces social support from other spouses and families. This study verified the overall relationship between coping (positive and negative), social support, and FQOL for caregivers of individuals with ASD through meta-analysis structural equation modeling (MASEM). This extended and expanded the double ABCX model. The results show that the methods and interventions that combine coping (internal provision) and social support (external provision) are effective in improving family quality of life for autistic persons' caregivers. This not only illustrates the importance of adjusting and changing negative coping, but also explains the significance of cognitive acuity of social resources (Ghanimi et al., 2018). It provides a reference for related medical service personnel, community workers, and other important persons in the social network of caregivers (Mourya & Singh, 2016). Professionals can cooperate with caregivers to help them develop parenting plans and teach positive coping strategies to manage various difficult problems they may encounter (Marsack-Topolewski & Wilson, 2021). Relevant experts can provide caregivers with telemedicine and mutual assistance platforms, and encourage family members and friends Table 2 Stage 2: Standardized Parameter Estimates (β) and 95% Confidence Intervals. Parameter estimates Coefficient 95% CI Lower Upper Direct effect, positive coping–social support Direct effect, negative coping–social support Direct effect, social support–family quality of life Direct effect, positive coping–family quality of life Direct effect, negative coping–family quality of life Indirect effect, positive coping–family quality of life Indirect effect, negative coping–family quality of life Correlation, positive coping and negative coping Residual variance, social support Residual variance, family quality of life 0.27 − 0.18 0.30 0.12 − 0.18 0.20 − 0.26 0.21 0.01 − 0.25 0.34 − 0.09 0.40 0.23 − 0.11 0.08 0.05 0.12 − 0.05 − 0.09 − 0.03 0.06 0.90 0.83 − 0.04 0.85 0.76 0.17 0.94 0.88 Note. Variance, positive coping, and variance, negative coping is equal to 1 by definition (because of analyzing a correlation matrix analysis). CI = confidence interval. Fig. 3. Meta-analysis structural equation model in this research. showed that the moderating effect of marital status was significant (χ2(5) = 13.135, p < .05) after omnibus tests, with a statistically sig­ nificant impact on the path of negative coping affecting social support. When the marriage rate increased by one standard, the direct effect of negative coping on social support increased by 0.12. Thus, caregivers with spouses were more likely to reduce social support when they adopted negative coping strategies than caregivers without spouses. 3.3. Publication bias tests Egger's linear regression test showed that the relationship between positive coping and negative coping was Z = − 1.79, p = .07; the rela­ tionship between positive coping and social support was Z = 0.77, p = .44; the relationship between positive coping and FQOL was Z = 1.79, p = .07; the relationship between negative coping and social support was Z = 0.51, p = .61; the relationship between negative coping and FQOL was Z = − 1.20, p = .23, and the relationship between social support and FQOL was Z = 0.25, p = .80. It can be seen from the above that p-values were not significant, and therefore there was no publication bias or small-study effect. 4. Discussion The objective of this study was to use TSSEM and OSMASEM methods of meta-analytical structural equation modeling (MASEM) to test the hypotheses of the relationship between coping, social support, and FQOL for caregivers of individuals with ASD by collecting multiple sample data. Results demonstrated that coping (positive and negative) and social support significantly affect FQOL in caregivers of individuals with ASD, and in the structural equation model constructed by the three, social support plays a partial mediating role. In addition, marital status plays a significant moderating role in the path of negative coping that affects social support. First, caregivers of ASD individuals adopting positive coping can 6 R. Wang et al. Personality and Individual Differences 186 (2022) 111351 of caregivers to provide instrumental and emotional support in order to reduce parenting pressure and improve FQOL (Ault et al., 2021; Yan et al., 2021). drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work. 4.1. Limitations of the present study and future directions Declaration of competing interest On one hand, although the path relationships of the structural equation model were proved, the collected data all came from crosssectional studies. Therefore, the sequence of occurrences between var­ iables is still worth exploring with longitudinal research methods for later researchers to form meta-analyses of longitudinal studies. This will make the results more realistic and reliable. Furthermore, this study did not consider the relationship between different dimensions of each variable, and therefore future research should refine related research between different dimensions of the three variables to clarify the in­ fluence mechanism and size of effects between dimensions. On the other hand, many studies have shown that compared with fathers and other caregivers of ASD, mothers have a higher level of caregiving involvement, and their mental health status should be paid more attention to by researchers (Al-Kandari et al., 2017; Cetinbakis et al., 2020; Papadopoulos, 2021; Singh et al., 2017). Therefore, in the future, when researchers study and analyze various psychological con­ structs of ASD caregivers, they can target the mothers of ASD, so that this group has more strategies for improving FQOL, and the research also has more unique research meaning. In addition, because of Chinese and English language restrictions, the included sample sizes were small; individual moderator variables' in­ formation provided in some articles was incomplete and not included, which made us lose the opportunity to explore the role of other moderator variables; when screening and coding literature as well as resolving inconsistencies, in addition to two of the authors' co-screening and independent coding, a third or more authors can also rule on dis­ agreements and participate in screening and coding; the method of testing publication bias only used Egger's test, which may affect the accuracy of the results. Therefore, future research can integrate the strengths of different scholars to include more samples, use more testing methods, and flexible and comprehensive ideas to explore more scien­ tific research facts. The author has declared that no competing interests exist. References Stanojević, N., Nenadović, V., Fatić, S., & Stokić, M. (2017). Exploring factors of stress level in parents of children with autistic spectrum disorder. Specijalna Edukacija i Rehabilitacija, 16(4), 445–463. https://doi.org/10.5937/specedreh16-13861 Weiss, J. A., Wingsiong, A., & Lunsky, Y. (2014). Defining crisis in families of individuals with autism spectrum disorders. Autism, 18(8), 985–995. https://doi.org/10.1177/ 1362361313508024 McCubbin, H. I., & Patterson, J. M. (1983). The family stress process: The double ABCX model of adjustment and adaptation. Marriage and Family Review, 6(1–2), 7–37. https://doi.org/10.1300/J002v06n01_02 McStay, R., Trembath, D., & Dissanayake, C. (2015). Raising a child with autism: A developmental perspective on family adaptation. Current Developmental Disorders Reports, 2(1), 65–83. https://doi.org/10.1007/s40474-014-0037-z Predescu, E., & Şipoş, R. (2017). Family quality of life in autism spectrum disorders (ASD). Autism: Paradigms, Recent Research and Clinical Applications, 87. https://doi. org/10.5772/66201 *Meleady, J., Nearchou, F., Bramham, J., & Carr, A. (2020). Family adaptation among parents of children on the autism spectrum without a comorbid intellectual disability: A test of the double ABCX model. Research in Autism Spectrum Disorders, 78, Article 101637. https://doi.org/10.1016/j.rasd.2020.101637 *Ji, B., Zhao, I., Turner, C., Sun, M., Yi, R., & Tang, S. (2014). Predictors of health-related quality of life in Chinese caregivers of children with autism spectrum disorders: A cross-sectional study. Archives of Psychiatric Nursing, 28(5), 327–332. https://doi. org/10.1016/j.apnu.2014.06.001 Ghanimi, F., Danesh, E., Dadkhah, A., & Taghiloo, S. (2018). Mediation role of coping strategies and perceived social support in relation to perceived stress and quality of life in parents with ASD children. Mourya, R. K., & Singh, R. N. (2016). Quality of life among parents of children with neuro-developmental disabilities in relation to family environment, coping style and social support. Indian Journal of Community Psychology, 12(2), 379–390. *Cappe, É., Poirier, N., Sankey, C., Belzil, A., & Dionne, C. (2018). Quality of life of French Canadian parents raising a child with autism spectrum disorder and effects of psychosocial factors. Quality of Life Research, 27(4), 955–967. https://doi.org/ 10.1007/s11136-017-1757-4 (Doctoral dissertation. *Lin, L. Y., Orsmond, G. I., Coster, W. J., & Cohn, E. S. (2011). Families of adolescents and adults with autism spectrum disorders in Taiwan: The role of social support and coping in family adaptation and maternal well-being. Research in Autism Spectrum Disorders, 5(1), 144–156. https://doi.org/10.1016/j.rasd.2010.03.004 *Pozo, P., Sarriá, E., & Brioso, A. (2014). Family quality of life and psychological wellbeing in parents of children with autism spectrum disorders: A double ABCX model. Journal of Intellectual Disability Research, 58(5), 442–458. https://doi.org/10.1111/ jir.12042 *Khanna, R., Madhavan, S. S., Smith, M. J., Patrick, J. H., Tworek, C., & BeckerCottrill, B. (2011). Assessment of health-related quality of life among primary caregivers of children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 41(9), 1214–1227. https://doi.org/10.1007/s10803-0101140-6 Park, J., Hoffman, L., Marquis, J., Turnbull, A. P., Poston, D., Mannan, H., & Nelson, L. L. (2003). Toward assessing family outcomes of service delivery: Validation of a family quality of life survey. Journal of Intellectual Disability Research, 47(4–5), 367–384. https://doi.org/10.1046/j.1365-2788.2003.00497.x Hoffman, L., Marquis, J., Poston, D., Summers, J. A., & Turnbull, A. (2006). Assessing family outcomes: Psychometric evaluation of the beach center family quality of life scale. Journal of Marriage and Family, 68(4), 1069–1083. https://doi.org/10.1111/ j.1741-3737.2006.00314.x Wang, Y., Xiao, L., Chen, R. S., Chen, C., Xun, G. L., Lu, X. Z., & Ou, J. J. (2018). Social impairment of children with autism spectrum disorder affects parental quality of life in different ways. Psychiatry Research, 266, 168–174. https://doi.org/10.1016/j. psychres.2018.05.057 Bromley, J., Hare, D. J., Davison, K., & Emerson, E. (2004). Mothers supporting children with autistic spectrum disorders: Social support, mental health status and satisfaction with services. Autism, 8(4), 409–423. https://doi.org/10.1177/ 1362361304047224 Pastor-Cerezuela, G., Fernández-Andrés, M. I., Pérez-Molina, D., & Tijeras-Iborra, A. (2021). Parental stress and resilience in autism spectrum disorder and down syndrome. Journal of Family Issues, 42(1), 3–26. https://doi.org/10.1177/ 0192513X20910192 Perumal, V., Veeraraghavan, V., & Lekhra, O. P. (2014). Journal of Pharmacology Research, 8(6), 791–797. https://doi.org/10.13140/2.1.4813.6320 Schlebusch, L., Dada, S., & Samuels, A. E. (2017). Family quality of life of South African families raising children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(7), 1966–1977. https://doi.org/10.1007/s10803-0173102-8 5. Conclusion This study used the TSSEM method in the meta-analysis structural equation modeling to determine if the social support of caregivers of people with ASD can positively predict their FQOL. The results showed that positive coping can increase caregivers' social support and improve FQOL, and negative coping can reduce social support and FQOL of caregivers. Social support for caregivers of persons with ASD plays a mediating role in coping (positive and negative), thus affecting the family quality of life. Analysis of the moderating effect showed that caregivers with spouses were more likely to reduce social support when they adopted negative coping than caregivers without spouses. Consent for publication Not applicable. Availability of data and materials All data, models, and codes generated or used during the study appear in the submitted article. Authors' contributions All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas, took part in 7 R. Wang et al. Personality and Individual Differences 186 (2022) 111351 Smith, S. (2018). Parent perceptions of family quality of life raising a child with autism spectrum disorder in the Bahamas. Doctoral dissertation. University of South Florida. ProQuest Dissertations & Theses Global. Marsack, C. N., & Samuel, P. S. (2017). Mediating effects of social support on quality of life for parents of adults with autism. Journal of Autism and Developmental Disorders, 47(8), 2378–2389. https://doi.org/10.1007/s10803-017-3157-6 Cobb, S. (1976). Presidential Address-1976. Social support as a moderator of life stress. Psychosomatic Medicine, 38(5), 300–314. https://doi.org/10.1097/00006842197609000-00003 Ault, S., Breitenstein, S. M., Tucker, S., Havercamp, S. M., & Ford, J. L. (2021). Caregivers of children with autism spectrum disorder in rural areas: A literature review of mental health and social support. Journal of Pediatric Nursing, 61, 229–239. https:// doi.org/10.1016/j.pedn.2021.06.009 Ueda, M. M., Ding, Y., Blumberg, F., Zhang, C., Yu, Q., & Lantier, K. (2020). Maternal parenting style in relation to parenting stress and behavioral outcomes in Japanese children with and without autism. Journal of Developmental and Physical Disabilities, 32(6), 983–1006. https://doi.org/10.1007/s10882-020-09727-z McIntyre, L. L., & Brown, M. (2018). Examining the utilisation and usefulness of social support for mothers with young children with autism spectrum disorder. Journal of Intellectual and Developmental Disability, 43(1), 93–101. https://doi.org/10.3109/ 13668250.2016.1262534 Bishop-Fitzpatrick, L., Mazefsky, C. A., & Eack, S. M. (2018). The combined impact of social support and perceived stress on quality of life in adults with autism spectrum disorder and without intellectual disability. Autism, 22(6), 703–711. https://doi.org/ 10.1177/1362361317703090 Edition, F. (2013). Diagnostic and statistical manual of mental disorders. American Psychiatric Association, 21. In American Psychiatric Association. Ekas, N. V., Pruitt, M. M., & McKay, E. (2016). Hope, social relations, and depressive symptoms in mothers of children with autism spectrum disorder. Research in Autism Spectrum Disorders, 29–30, 8–18. https://doi.org/10.1016/j.rasd.2016.05.006 Lei, X., & Kantor, J. (2021). International Journal of Disability, Development and Education, 1–14. https://doi.org/10.1080/1034912X.2021.1940881 Obeid, R., & Daou, N. (2015). The effects of coping style, social support, and behavioral problems on the well-being of mothers of children with autism spectrum disorders in Lebanon. Research in Autism Spectrum Disorders, 10, 59–70. https://doi.org/10.1016/ j.rasd.2014.11.003 McGrew, J. H., & Keyes, M. L. (2014). Caregiver stress during the first year after diagnosis of an autism spectrum disorder. Research in Autism Spectrum Disorders, 8 (10), 1373–1385. https://doi.org/10.1016/j.rasd.2014.07.011 Garrido, D., Carballo, G., & Garcia-Retamero, R. (2020). Siblings of children with autism spectrum disorders: Social support and family quality of life. Quality of Life Research, 29(5), 1193–1202. https://doi.org/10.1007/s11136-020-02429-1 Schiller, V. F., Dorstyn, D. S., & Taylor, A. M. (2021). The protective role of social support sources and types against depression in caregivers: A meta-analysis. Journal of Autism and Developmental Disorders, 51(4), 1304–1315. https://doi.org/10.1007/s10803020-04601-5 Folkman, S. (1984). Personal control and stress and coping processes: A theoretical analysis. Journal of Personality and Social Psychology, 46(4), 839–852. https://doi. org/10.1037//0022-3514.46.4.839 Craig, F., Savino, R., Fanizza, I., Lucarelli, E., Russo, L., & Trabacca, A. (2020). A systematic review of coping strategies in parents of children with attention deficit hyperactivity disorder (ADHD). Research in Developmental Disabilities, 98, Article 103571. https://doi.org/10.1016/j.ridd.2020.103571 Spady, B. L. (1993). The relationship between coping style and actual coping strategies used during cardiac catheterization. Master dissertation. Algorani, E. B., & Gupta, V. (2021). Coping mechanisms [Internet] https://www.ncbi.nlm. nih.gov/books/NBK559031. Benson, P. R. (2010). Coping, distress, and well-being in mothers of children with autism. Research in Autism Spectrum Disorders, 4(2), 217–228. https://doi.org/10.1016/j. rasd.2009.09.008 Bozkurt, G., Uysal, G., & Düzkaya, D. S. (2019). Examination of care burden and stress coping styles of parents of children with autism spectrum disorder. Journal of Pediatric Nursing, 47, 142–147. https://doi.org/10.1016/j.pedn.2019.05.005 Herman, J. L., & Tetrick, L. E. (2009). Problem-focused versus emotion-focused coping strategies and repatriation adjustment. Human Resource Management, 48(1), 69–88. https://doi.org/10.1002/hrm.20267 Ward, R. N., Brady, A. J., Jazdzewski, R., & Yalch, M. M. (2021). Stress, resilience, and coping. In (pp. 3–14). Apple Academic Press. Meyer, B. (2001). Coping with severe mental illness: Relations of the brief COPE with symptoms, functioning, and well-being. Journal of Psychopathology and Behavioral Assessment, 23(4), 265–277. https://doi.org/10.1023/A:1012731520781 Brown, M., Whiting, J., Kahumoku-Fessler, E., Witting, A. B., & Jensen, J. (2020). A dyadic model of stress, coping, and marital satisfaction among parents of children with autism. Family Relations, 69(1), 138–150. https://doi.org/10.1111/fare.12375 Lai, W. W., Goh, T. J., Oei, T. P., & Sung, M. (2015). Coping and well-being in parents of children with autism spectrum disorders (ASD). Journal of Autism and Developmental Disorders, 45(8), 2582–2593. https://doi.org/10.1007/s10803-015-2430-9 Jing, S., Jianhua, B., & Zongwei, Z. (2017). The relationship between coping style and mental health of parents of children with autism: The mediating role of social support. Chinese Journal of Hospital Statistics, 03. CNKI:SUN:JTYY.0.2017-03-011. *Whitehead, K., Dorstyn, D., & Ward, L. (2015). Psychological adjustment in families affected by autism spectrum disorder. Journal of Developmental and Physical Disabilities, 27(5), 703–717. https://doi.org/10.1007/s10882-015-9446-0 Novara, C., Garro, M., & Rienzo, G. D. (2015). Coping styles and social support in emergency workers: Family as a resource. Revista Romaneasca Pentru Educatie Multidimensionala, 7(1), 129–140. https://doi.org/10.18662/rrem/2015.0701.09 Stuart, M., & McGrew, J. H. (2009). Caregiver burden after receiving a diagnosis of an autism spectrum disorder. Research in Autism Spectrum Disorders, 3(1), 86–97. https://doi.org/10.1016/j.rasd.2008.04.006 McKee, S. L., Liu, X., Truong, D. M., Meinert, A. C., Daire, A. P., & Mire, S. S. (2020). The family adjustment measure: Identifying stress in parents of youth with autism. Journal of Child and Family Studies, 29(2), 592–604. https://doi.org/10.1007/ s10826-019-01569-4 Lovell, B., & Wetherell, M. A. (2015). Child behaviour problems mediate the association between coping and perceived stress in caregivers of children with autism. Research in Autism Spectrum Disorders, 20, 17–23. https://doi.org/10.1016/j.rasd.2015.08.003 Pourmohamadreza-Tajrishi, M., Azadfallah, P., Hemmati Garakani, S. H., & Bakhshi, E. (2015). The effect of problem-focused coping strategy training on psychological symptoms of mothers of children with down syndrome. Iranian Journal of Public Health, 44(2), 254–262. https://www.ncbi.nlm.nih.gov/pmc/articles/pmc 4401884/. Khanna, R., Jariwala-Parikh, K., West-Strum, D., & Mahabaleshwarkar, R. (2014). Health-related quality of life and its determinants among adults with autism. Research in Autism Spectrum Disorders, 8(3), 157–167. https://doi.org/10.1016/j. rasd.2013.11.003 *Salas, B. L., Rodríguez, V. Y., Urbieta, C. T., & Cuadrado, E. (2017). The role of coping strategies and self-efficacy as predictors of life satisfaction in a sample of parents of children with autism spectrum disorder. Psicothema, 29(1), 55–60. https://doi.org/ 10.7334/psicothema2016.96 Vernhet, C., Dellapiazza, F., Blanc, N., Cousson-Gélie, F., Miot, S., Roeyers, H., & Baghdadli, A. (2019). Coping strategies of parents of children with autism spectrum disorder: A systematic review. European Child & Adolescent Psychiatry, 28(6), 747–758. https://doi.org/10.1007/s00787-018-1183-3 Özgür, B. G., Aksu, H., & Eser, E. (2018). Factors affecting quality of life of caregivers of children diagnosed with autism spectrum disorder. Indian Journal of Psychiatry, 60 (3), 278. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_300_17 Wang, H., Hu, X., & Han, Z. R. (2020). Parental stress, involvement, and family quality of life in mothers and fathers of children with autism spectrum disorder in mainland China: A dyadic analysis. Research in Developmental Disabilities, 107, Article 103791. https://doi.org/10.1016/j.ridd.2020.103791 McAuliffe, T., Cordier, R., Vaz, S., Thomas, Y., & Falkmer, T. (2017). Quality of life, coping styles, stress levels, and time use in mothers of children with autism spectrum disorders: Comparing single versus coupled households. Journal of Autism and Developmental Disorders, 47(10), 3189–3203. https://doi.org/10.1007/s10803-0173240-z Dabrowska, A., & Pisula, E. (2010). Parenting stress and coping styles in mothers and fathers of pre-school children with autism and down syndrome. Journal of Intellectual Disability Research, 54(3), 266–280. https://doi.org/10.1111/j.13652788.2010.01258.x Meral, B. F., Cavkaytar, A., Turnbull, A. P., & Wang, M. (2013). Family quality of life of Turkish families who have children with intellectual disabilities and autism. Research and Practice for Persons with Severe Disabilities, 38(4), 233–246. https://doi.org/ 10.1177/154079691303800403 Ghanouni, P., & Hood, G. (2021). Stress, coping, and resiliency among families of individuals with autism: A systematic review. Review Journal of Autism and Developmental Disorders, 8, 389–402. https://doi.org/10.1007/s40489-021-00245-y Kousha, M., Attar, H. A., & Shoar, Z. (2016). Anxiety, depression, and quality of life in Iranian mothers of children with autism spectrum disorder. Journal of Child Health Care, 20(3), 405–414. https://doi.org/10.1177/1367493515598644 Dardas, L. A., & Ahmad, M. M. (2014). Predictors of quality of life for fathers and mothers of children with autistic disorder. Research in Developmental Disabilities, 35 (6), 1326–1333. https://doi.org/10.1016/j.ridd.2014.03.009 Robinson, S., & Weiss, J. A. (2020). Examining the relationship between social support and stress for parents of individuals with autism. Research in Autism Spectrum Disorders, 74, Article 101557. https://doi.org/10.1016/j.rasd.2020.101557 Alenazi, D. S., Hammad, S. M., & Mohamed, A. E. (2020). Effect of autism on parental quality of life in Arar city, Saudi Arabia. Journal of Family & Community Medicine, 27 (1), 15. https://doi.org/10.4103/jfcm.JFCM_157_19 Alhazmi, A., Petersen, R., & Donald, K. (2018). Quality of life among parents of South African children with autism spectrum disorder. Acta Neuropsychiatrica, 30(4), 226–231. https://doi.org/10.1017/neu.2018.5 Omar, T. E., Ahmed, W. M., & Basiouny, N. S. (2017). Challenges and adjustments of mothers having children with autism. Alexandria Journal of Pediatrics, 30(3), 120. htt p://www.ajp.eg.net/text.asp?2017/30/3/120/230766. Gagat-Matula, A. (2021). The financial situation of families and the quality of life and coping with stress of children with ASD during the SARS-CoV-2 pandemic. Risks, 9 (5), 95. https://doi.org/10.3390/risks9050095 Al-Tal, S. M., Al-Jawaldeh, F. E., Al-Taj, H. M., & Aleid, W. A. (2021). Family support for children with autism spectrum disorder during the COVID-19 pandemic. Journal of Educational and Psychological Sciences, 5(5). https://doi.org/10.26389/AJSRP. R130920, 186-164. Carver, C. S. (1997). You want to measure coping but your protocol’too long: Consider the brief cope. International Journal of Behavioral Medicine, 4(1), 92–100. https://doi. org/10.1207/s15327558ijbm0401_6 Zimet, G. D., Dahlem, N. W., Zimet, S. G., & Farley, G. K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52(1), 30–41. https://doi.org/10.1207/s15327752jpa5201_2 Whoqol Group. (1995). The World Health Organization quality of life assessment (WHOQOL): Position paper from the World Health Organization. Social Science & Medicine, 41(10), 1403–1409. https://doi.org/10.1016/0277-9536(95)00112-K Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & Prisma Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. 8 R. Wang et al. Personality and Individual Differences 186 (2022) 111351 support and low morning cortisol levels in parents of children with autism spectrum disorder. Research in Developmental Disabilities, 35(3), 686–695. https://doi.org/ 10.1016/j.ridd.2013.12.007 Schneider-Matyka, D., Libersbach, E., Szkup, M., Stanisławska, M., Starczewska, M., & Grochans, E. (2018). The assessment of social support provided for and stress-coping strategies adopted by parents of chronically ill children. Nursing Problems / Problemy Pielęgniarstwa, 26(2), 164–170. https://doi.org/10.5114/ppiel.2018.78875 *Pyszkowska, A., & Wrona, K. (2021). Self-compassion, ego-resiliency, coping with stress and the quality of life of parents of children with autism spectrum disorder. PeerJ, 9, Article e11198. https://doi.org/10.7717/peerj.11198 Chowdhury, M. S. H., Islam, M. Z., Bhuiyan, M. R., Rafi, A., & Kawsar, A. A. (2019). Parenting stress and coping capacity linked with quality of life among parents of children with autism Spectrum disorder. Journal of Armed Forces Medical College, Bangladesh, 15(1), 48–54. https://doi.org/10.3329/jafmc.v15i1.48642 Siah, P. C., & Tan, S. H. (2016). Relationships between sense of coherence, coping strategies and quality of life of parents of children with autism in Malaysia: A case study among Chinese parents. Disability, CBR and Inclusive Development, 27(1), 78–91. https://doi.org/10.5463/dcid.v27i1.485 Vaz, S., Thomson, A., Cuomo, B., Falkmer, T., Chamberlain, A., & Black, M. H. (2021). Co-occurring intellectual disability and autism: Associations with stress, coping, time use, and quality of life in caregivers. Research in Autism Spectrum Disorders, 84. https://doi.org/10.1016/j.rasd.2021.101765 Dardas, L. A., & Ahmad, M. M. (2015). For fathers raising children with autism, do coping strategies mediate or moderate the relationship between parenting stress and quality of life? Research in Developmental Disabilities, 36C, 620–629. https://doi.org/ 10.1016/j.ridd.2014.10.047 Marsack-Topolewski, C. N., & Wilson, K. P. (2021). Coping strategies used by aging parental caregivers of adults with autism spectrum disorder. Families in Society, 102 (1), 119–132. https://doi.org/10.1177/1044389420913121 Yan, T., Hou, Y., & Deng, M. (2021). Direct, indirect, and buffering effect of social support on parental involvement among Chinese parents of children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 1–13. https://doi. org/10.1007/s10803-021-05170-x Al-Kandari, S., Alsalem, A., Abohaimed, S., Al-Orf, F., Al-Zoubi, M., Al-Sabah, R., & Shah, N. (2017). Brief report: Social support and coping strategies of mothers of children suffering from ASD in Kuwait. Journal of Autism and Developmental Disorders, 47(10), 3311–3319. https://doi.org/10.1007/s10803-017-3225-y Cetinbakis, G., Bastug, G., & Ozel-Kizil, E. T. (2020). Factors contributing to higher caregiving burden in Turkish mothers of children with autism spectrum disorders. 66 (1), 46–53. https://doi.org/10.1080/20473869.2018.1478630 Papadopoulos, D. (2021). Mothers' experiences and challenges raising a child with autism spectrum disorder: A qualitative study. Brain Sciences, 11(3), 309. https:// doi.org/10.3390/brainsci11030309 Singh, P., Ghosh, S., & Nandi, S. (2017). Subjective burden and depression in mothers of children with autism Spectrum disorder in India: Moderating effect of social support. Journal of Autism and Developmental Disorders, 47, 3097–3111. https://doi.org/ 10.1007/s10803-017-3233-y PLoS Medicine, 6(7), Article e1000097. https://doi.org/10.1371/journal. pmed.1000097 Deng, X. P., Luo, X. W., & Wu, Y. Z. (2016). The mediating effect of parental involvement between family socioeconomic status and academic performance: Meta-analysis structural equation modeling. Advances in Psychological Science, 24(12), 1844. https://doi.org/10.3724/SP.J.1042.2016.01844 Roorda, D. L., Koomen, H. M. Y., Spilt, J. L., & Oort, F. J. (2011). The influence of affective teacher–student relationships on students' school engagement achievement: A meta-analytic approach. Review of Educational Research, 81(4), 493–529. https:// doi.org/10.3102/0034654311421793 Tehrani, H. D., & Yamini, S. (2020). Parenting practices, self-control and anti-social behaviors: Meta-analytic structural equation modeling. Journal of Criminal Justice, 68. https://doi.org/10.1016/j.jcrimjus.2020.101687, 101687 Cheung, M. W. L. (2014). metaSEM: An R package for meta-analysis using structural equation modeling. Frontiers in Psychology, 5, 1521. https://doi.org/10.3389/ fpsyg.2014.01521 Viechtbauer, W. (2010). Conducting meta-analyses in R with the metafor package. Journal of Statistical Software, 36(3), 1–48. https://doi.org/10.18637/jss.v036.i03 Cheung, M. W. L., & Chan, W. (2005). Meta-analytic structural equation modeling: A two-stage approach. Psychological Methods, 10(1), 40–64. https://doi.org/10.1037/ 1082-989X.10.1.40 Cochran, W. G. (1954). The combination of estimates from different experiments. Biometrics, 10(1), 101–129. https://doi.org/10.2307/3001666 Hedges, L. V., & Olkin, I. (2014). Statistical methods for meta-analysis. Cambridge: Academic Press. Higgins, J. P., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ, 327(7414), 557–560. https://doi.org/ 10.1136/bmj.327.7414.557 Jak, S., & Cheung, M. W. L. (2020). Meta-analytic structural equation modeling with moderating effects on SEM parameters. Psychological Methods, 25(4), 430–455. https://doi.org/10.1037/met0000245 Griffin, J. W., Bauer, R., & Scherf, K. S. (2021). A quantitative meta-analysis of face recognition deficits in autism: 40 years of research. Psychological Bulletin, 147(3), 268–292. https://doi.org/10.1037/bul0000310 Egger, M., Davey Smith, G. D., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315(7109), 629–634. https://doi.org/ 10.1136/bmj.315.7109.629 Yu, B. C. L., Chio, F. H. N., Mak, W. W. S., Corrigan, P. W., & Chan, K. K. Y. (2021). Internalization process of stigma of people with mental illness across cultures: A meta-analytic structural equation modeling approach. Clinical Psychology Review, 87, Article 102029. https://doi.org/10.1016/j.cpr.2021.102029 Pisula, E., & Banasiak, A. (2020). Empowerment in polish fathers of children with autism and down syndrome: The role of social support and coping with stress – A preliminary report. Journal of Intellectual Disability Research, 64(6), 434–441. https:// doi.org/10.1111/jir.12681 Ruiz-Robledillo, N., De Andrés-García, S., Pérez-Blasco, J., González-Bono, E., & MoyaAlbiol, L. (2014). Highly resilient coping entails better perceived health, high social 9